Chief Complaint: Swollen left eye and sinus infection
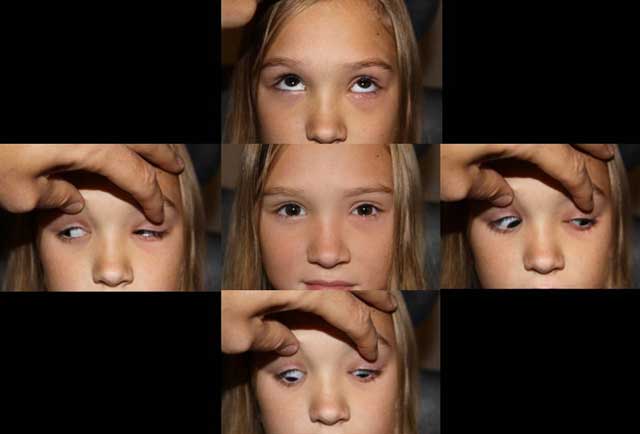
History of Present Illness: 9-year-old female with left nasal pain 4 days prior to presentation. Her left eye was swollen and red and seemed to be worsening. The patient also stated that it had been more difficult to open her left eye and there had been some mattering on her eyelids. She also noticed diplopia in all gazes.
She initially presented to her pediatrician who thought she had a preseptal cellulitis and started her on amoxicillin.
However, after one day on amoxicillin, the patient returned to her pediatrician because her symptoms were worsening. She was switched to Augmentin and had 5 doses when she presented to our institution.
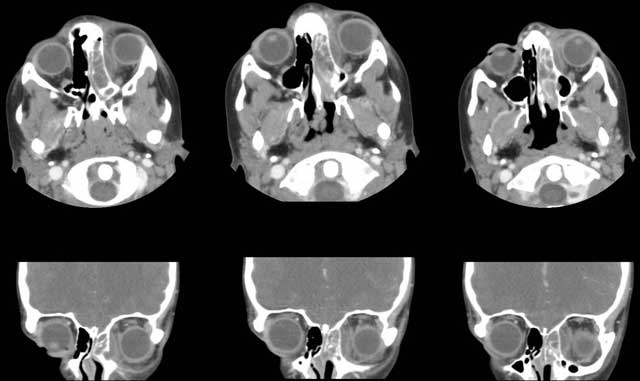
The patient's pediatrician also ordered a maxillofacial CT at her return visit. (see below)
Past Ocular History: none
Medical History: none
Medications:
Allergies: none
Family History: Non contributory.
Review of Systems: Afebrile, mild headache, clear mild rhinorrhea, no neck stiffness
External Exam
EXTERNAL/SLIT LAMP EXAM
Vital signs: BP 115/68, Pulse 76, T 36.9
Laboratory tests:
(Elevated abnormal values are in ITALICS)
 |
 |
 |
 |
Hospital Course: The patient was admitted into the hospital and treated with IV ceftriaxone and clindamycin. She was also treated with Afrin® (oxymetazoline) spray. Otolaryngology was consulted to address the sinusitis.
Her symptoms improved quickly after the initiation of IV antibiotics treatment. Her motility was almost full after one day of treatment. The patient was monitored every 12 hours by ophthalmology. By admission day 3, the patient was feeling better with full motility and much improved erythema and edema of her left eye. Diplopia was resolved.
Her sinus symptoms had also improved.
The patient was discharged home on hospital admission day 4 with a two-week course of clindamycin and nasal steroids.
 |
 |
Orbital cellulitis is an infection of the soft orbital tissue posterior to the orbital septum. This is in contrast to preseptal cellulitis which is a soft tissue infection of the eyelids anterior to the orbital septum. If a diagnosis of preseptal cellulitis is entertained, a well-defined event should be elicited from the patient (e.g. injury, stye, bug bite, etc). If a convincing event cannot be elicited, an orbital etiology should always be investigated with orbital imaging. The patient in this case was diagnosed initially with a preseptal cellulitis with no predisposing event.
The most common bacterial organisms in orbital cellulitis include Streptococcus species, Staphylococcus aureus, Pseudomonas, Enterococcus, Klebsiella, and Haemophilus influenzae type B. Methocillin-resistant staph aureus is becoming more common in orbital cellulitis. If a fungal infection is suspected, consider Mucor and Aspergillus species.
90% of cases occur as a secondary extension of acute or chronic bacterial sinusitis, especially the ethmoid sinuses. Other extensions of periorbital structures include the face/eyelids, dacryocystitis and dental infections. Exogenous causes include trauma and orbital/periorbital surgery. An orbital foreign body (specifically organic) should always be entertained in the setting of an orbital cellulitis that is not responding to antibiotic therapy. Endogenous causes include septic embolization from bacteremia. There may also be intraorbital causes including endophthalmitis and dacryoadenitis.
Orbital clinical findings include proptosis, ptosis, restriction of ocular motility, ocular pain, and chemosis. If there is decreased visual acuity, or a visual field or relative afferent pupillary defect, one must consider compressive optic neuropathy which warrants urgent aggressive management.
Systemic clinical findings are essential in the workup of possible orbital cellulitis. Pertinent findings include leukocytosis and fever. In this patient, she had already been treated with a four day course of antibiotics which explains her afebrile state as well as her normal WBC count. However she still exemplified elevated neutrophils, monocytes, ESR and CRP which also demonstrate an infectious etiology.
CT of the orbits and the paranasal sinuses is essential. Evidence of sinusitis mandates otolaryngology involvement. Lumbar puncture is necessary if meningeal signs and symptoms develop. Conjunctival cultures add very little information. Nasal cultures may be appropriate if there is significant nasal discharge in the setting of sinusitis. Blood cultures are appropriate in the setting of septicemia. If surgical drainage of the orbita and/or sinus is performed, cultures should be obtained.
Surgical intervention is less likely in orbital cellulitis in children (≤ 9 years old) because the infection is caused by a single gram positive organism. IV antibiotic therapy is the initial treatment of choice. Progression (worsening motility deficit, pain, optic nerve dysfunction) in a child after 24-48 hours of IV antibiotic therapy would lead one to drain the abscess. However, if this were an adult patient, with evidence of an abscess formation, early surgical intervention to drain the involved sinus and orbital abscess is usually indicated along with medical therapy given that the infection is more likely to be polymicrobial.
Consider surgical management if the patient has any of the following:
Clinical improvement does not correlate accurately with repeat CT scan analysis. It may take 48-72 hrs for the abscess to improve on imaging.
The majority of patients respond well to medical and/or surgical treatments. Rarely, orbital cellulitis may spread posteriorly to the cavernous sinus, meninges and the brain parenchyma.
Diagnosis: Orbital Cellulitis
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENTIn children
In adults
|
Infectious orbital inflammation
Non-infectious orbital inflammation
Hong ES, Allen RC. Orbital Cellulitis in a Child. EyeRounds.org. January 12, 2010; Available from: http://www.EyeRounds.org/cases/103-Pediatric-Orbital-Cellulitis.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.