Current Complaint: Right-sided periocular swelling.
History of Present Illness: A 76-year-old female recently diagnosed with acute myelogenous leukemia (AML) and admitted for induction chemotherapy (day 13) presented with a two day history of worsening right-sided periorbital swelling and erythema. She denied pain, pain with eye movement, discharge or itching. She reported tearing but no foreign body sensation. She felt that her vision had been declining over the past 2 days and that her eye felt full.
Review of symptoms: She had been febrile for 4 days and felt overall weak and tired. She reported that her nose had been stuffy but without discharge for about 2 weeks. She denied headache.
Past Ocular History: History of central retinal vein occlusion (CRVO) OS, primary open angle glaucoma, myopia and presbyopia
Medical History: AML (diagnosed one month prior), hypertension, hypercholesterolemia
Systemic Medications: Cytarabine, daunorubicin, daptomycin, meropenem, ciprofloxacin, acyclovir, fluconazole, captopril, atenolol, heparin
Ocular Medications: Cosopt® (dorzolamide hydrochloride-timolol maleate) OU twice daily, latanoprost OU at bedtime nightly
Family and Social History: Noncontributory
Examination:
Vitals: BP 148/65 | Pulse 64 | Temp 38.1°C (100.6°F) | Resp 18 | SpO2 98%
Visual acuity:
Pupils: symmetric and reactive, no RAPD
Intraocular pressure:
Confrontation visual fields: full
Extraocular motility:
Hertel exophthalometry: 23mm OD and 21mm OS
External:
Anterior Segment Examination:
Dilated Fundus Examination:
 |
 |
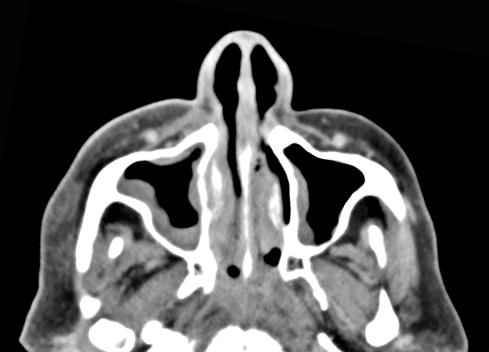
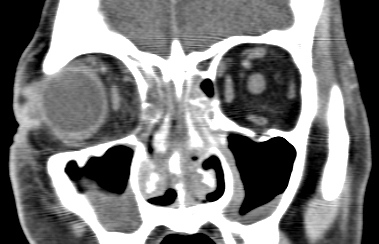
A maxillofacial CT scan was performed:
 |
 |
 |
A complete blood count revealed pancytopenia with a preponderance of blasts, consistent with her diagnosis of AML, see Complete Blood Count above.
Course: Otolaryngology was urgently consulted and on bedside endoscopy the patient was noted to have diffuse edema which despite decongestion obscured the view of the right middle turbinate. The left middle turbinate appeared ischemic and did not bleed with probing.
The clinical suspicion of invasive fungal sinusitis and its grave nature as well as need for possible larger surgery, should it be confirmed, was discussed with the patient and her family. The patient was typed and crossed, transfused platelets and taken emergently to the operating room for biopsy and functional endoscopic sinus surgery with oculoplastics on standby.
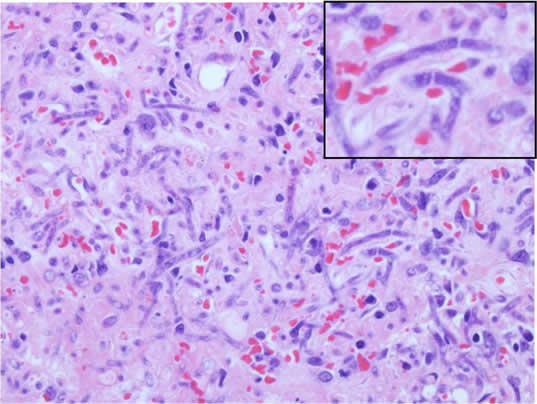
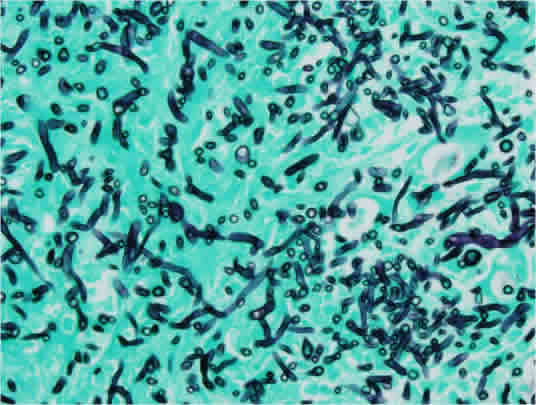
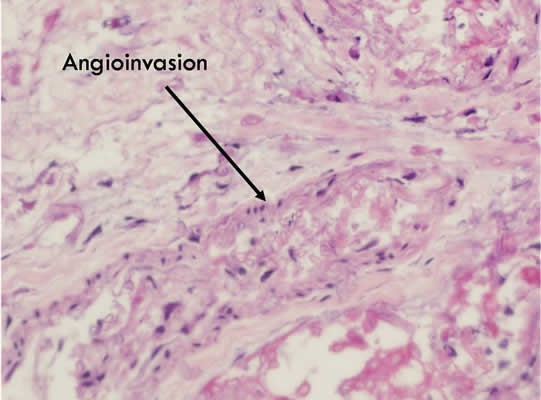
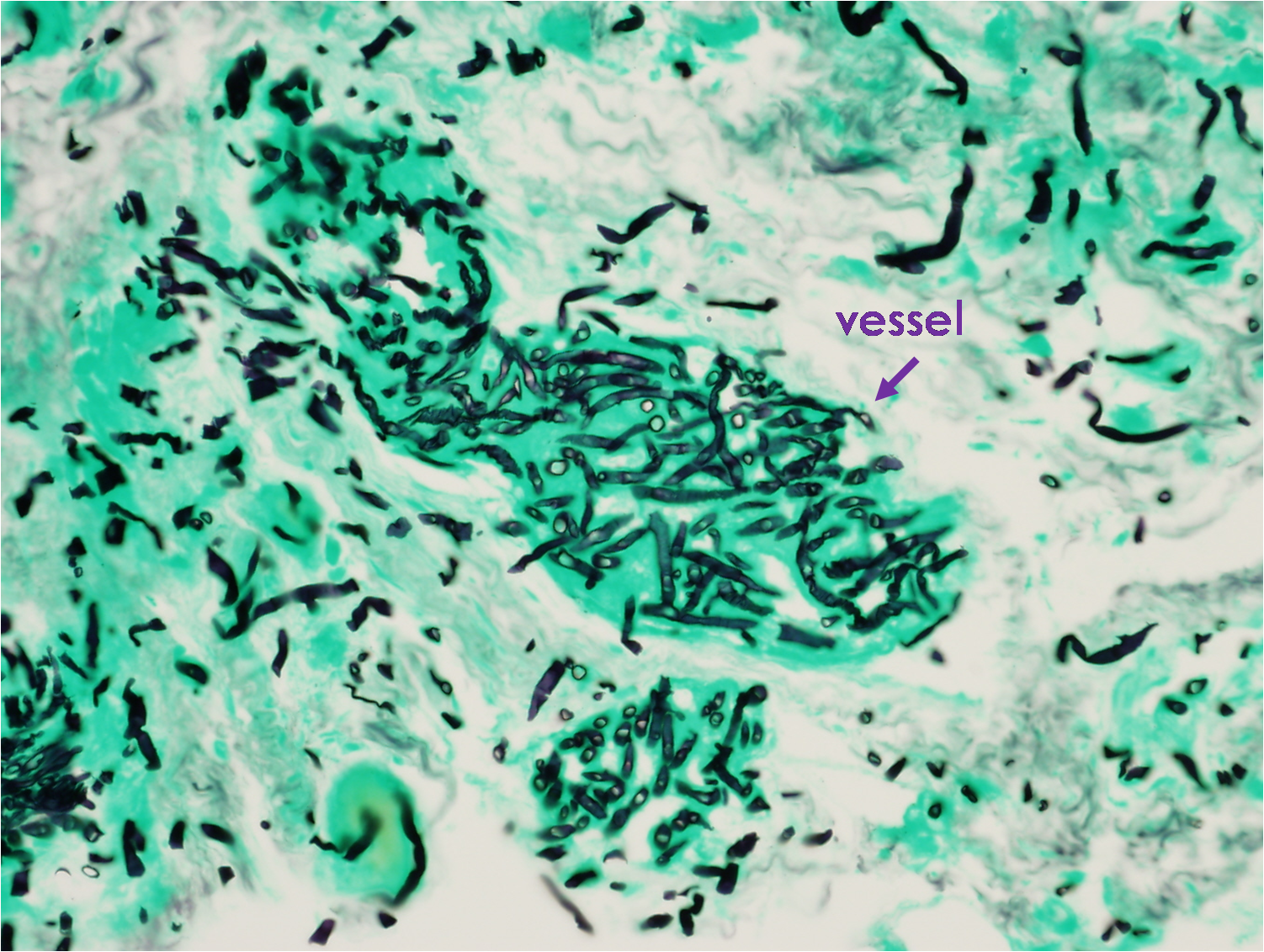
Fresh sections were sent to pathology and invasive mucormycosis was identified in the majority of specimens including the right maxillary sinus, left maxillary sinus and bilateral ethmoids with involvement of the posterior ethmoid on the right. Transcaruncular medial orbitotomy with external anterior and posterior ethmoidectomies were performed on the right. The right medial orbital fat, anterior and posterior ethmoids were also found to be involved.
 |
 |
 |
 |
The patient was placed on postoperative intravenous amphotericin b, and amphotericin b nasal washings. Post-operative MRI images did not demonstrate invasion of the left orbit or intracerebral involvement. The operative and biopsy findings were discussed with the patient and the family. We explained that standard surgical treatment for invasive fungal disease includes removing all infected tissue, which would include subtotal or total exenteration of the right orbital cavity including the infected soft tissue and orbital structures, as well as extensive sinus surgery of the ethmoid, maxillary sinus and sphenoid sinus bilaterally. A biopsy of the tissue around the left orbit would also be necessary. It was felt that surgical intervention could stabilize her disease until her granulocyte count improved; however, it would be unlikely to yield a cure given her neutropenic state. After extensive discussion with the patient's family, the family elected to place the patient on comfort care. The patient succumbed to her disease 5 days later.
Diagnosis: Mucormycosis
Discussion: Mucormycosis (zygomycosis) and Aspergillus infections are aggressive fungal infections that carry high mortality rates. The family of the Mucoraceae is divided into the subspecies absidia, rhizopus and mucor. There is some controversy to the terminology used to refer to infections caused by this species. Mycologists prefer zygomycosis and others use phycomycosis since other member of this class can cause similar infection; however, clinicians more commonly use mucormycosis and this terminology will be used throughout the remainder of this discussion. Mucormycosis is ubiquitous in nature; found in soil and on decaying vegetation. It has the ability to rapidly grow and release large numbers of spores that become airborne and gain entrance to the human body through inhalation or ingestion. Given its ubiquitous nature, humans are exposed on a regular basis; however it rarely causes an infection in one with an intact immune system which can phagocytize the spores.[1] In the immunocompromised, germination and hyphae formation occur and a variety of infections can develop including orbitorhinocerebral infection, as well as pulmonary, gastrointestinal, cutaneous, renal and isolated central nervous system infections.[2]
Risk factors include, but are not limited to:
The most common presentation is rhinoorbitalcerebral mucormycosis and will be of focus of the following discussion. Inoculation is presumed to start with inhalation of spores in a susceptible host. The presentation typically is a rapidly progressive infection but cases of indolent disease have been reported. Common symptoms include sinusitis, nasal stuffiness and purulent discharge, headache, and fever. Pain may be present or absent at the time of presentation.[3] The infection can spread to adjacent structures and cause more widespread and devastating disease. Signs of disease include the following:
Invasive fungal infections carry a high mortality rate and prognosis depends on the underlying condition. Mortality rates quoted in literature range from 20-70%.[4] Managing this infection is primarily surgical but requires close medical management and often a collaboration of multiple specialties. Imaging with CT and MRI are helpful in determining extent of the disease.[5] The sinus mucosa typical appears heterogenous on scan. The sinuses may be only mildly thickened as noted in our patient. Medical care includes treatment of underlying medical disease and discontinuation of immunosuppressive medications with rapid turnaround in granulocyte count if possible.
Definitive treatment for invasive fungal disease is surgical debridement because systemic medications cannot reach the infected tissue due to vaso-occlusion. Surgical management includes aggressive debridement of all necrotic tissue, sometimes requiring multiple debridements.[6] The involved tissue rarely bleeds, so debridement until normal, well-perfused, bleeding tissue is encountered is the ideal endpoint. During debridement, it is imperative to send frozen and permanent sections and fresh tissue to confirm the diagnosis. If clinical suspicion is high, but initial specimens are negative, additional specimens, including the arteries should be biopsied. The wide surgical debridement of devitalized tissue can often be extensive and disfiguring. Orbital exenteration, along with removal of the sinuses, may be necessary. Reconstructive surgery should only be considered after full recovery of infection.
Amphoterin B is the first-line antifungal of choice. Systemic IV amphotericin B should be administered immediately with goal of achieving the highest possible tissue levels without causing toxicity.[7] It is derived from Streptomyces nodosus and actsby binding to sterols in the cell membrane of the fungi, changing the permeability of the membrane. Local irrigation or packing of the debrided areas with amphotericin B can be an adjunct to therapy and help deliver medication to the poorly perfused tissue. Posaconazole is a broad spectrum oral agent that can be tried in those that have failed or not tolerated amphotericin B or as an option for step down therapy.[8,9] Until an IV dose is available, it should not be initial therapy. Other antifungals including, voriconazole, fluconazole, flucystosine are not effective against mucormycosis (zycomycetes).[10]
The definitive diagnosis can be made by histological examination. Hyphae are typical and specific for each fungus. Mucor presents large, broad non-septate hyphae with right-angle branching, and Aspergillus shows septate hyphae that branch at 45° angles.
Hyperbaric oxygen therapy has been proposed as an adjunctive therapy. The proposed mechanism is that an increase of free oxygen radicals stimulates the oxygen-dependent peroxidase system, thereby enabling leukocytes to kill microorganisms. Case reports discuss benefits but the role of hyperbaric oxygen is not yet known.[11]
Epidemiology:Aggressive fungal opportunistic infection that can cause of variety of infections, most common presentation is orbitorhinocerebral infection Fungus directly invades blood vessels and causes tissue destruction and necrosis Carries a high morbidity and mortality rate Most present as rapidly progressive infection Acute surgical emergency |
Signs:
|
Symptoms:
|
Treatment:The keys to successful therapy include high clinical suspicion and recognition of the signs and symptoms that can lead to early diagnosis. Imaging with CT and MRI to aid in determination of extent of disease. Multidisciplinary approach
|
Rogers GM, Melicher Larson J, Carter KD. Invasive Fungal Orbitorhinocerebral Mucormycosis. EyeRounds.org. February 16, 2010; Available from: http://www.EyeRounds.org/cases/108-Orbitorhinocerebral-Mucormycosis.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.