Chief Complaint: Blurry vision, headaches, and difficulty moving the right eye for the past two weeks
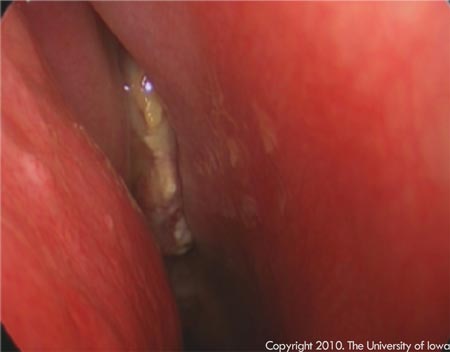
History of Present Illness: The patient is a previously healthy 11-year-old boy who presented to clinic complaining of blurry vision, headaches, and difficulty moving his right eye for the past two weeks. The patient had complained to his mother about these symptoms after his friend had bumped him in the head while they were swimming. The patient's mother brought the patient to their local ophthalmologist to be evaluated. After examining the patient, the ophthalmologist sent the patient to an outside hospital for an MRI of the brain and orbit. The MRI showed a heterogeneous mass originating in the patient's ethmoid and/or sphenoid sinus with intracranial extension and encasement of the right optic nerve causing mass effect on the right medial rectus and the right superior oblique muscles. The patient was subsequently sent to the University of Iowa for further evaluation by the Oculoplastics Service as well as the Pediatric Hematology/Oncology, Otolaryngology, and Neurosurgery Services.
Past Ocular History: None
Review of Systems: No nausea, vomiting, seizures, balance problems, or mental status changes
Medications: No prior-to-admission medications
External: Normal OU
Extraocular motility: -2 abduction deficit OD, normal OS
Pupils: Equal, round, no RAPD OU
Tonometry: Soft to palpation OU
Slit lamp exam: Normal OU
Dilated fundus exam: Normal OU
 |
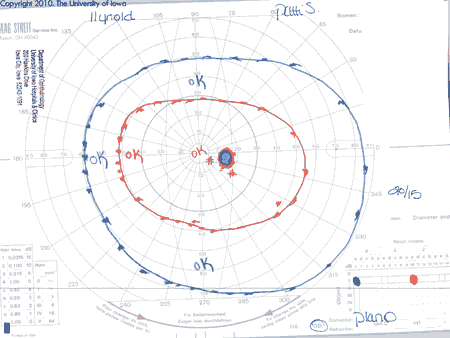
Assessment: Previously healthy 11-year-old boy with a sinus mass extending into the right posterior orbit; exam, imaging, and GVF OD consistent with compressive optic neuropathy. The patient underwent the following procedures:
 |
Extraocular motility: -1 Abduction deficit OD, normal OS
Pupils: Mild RAPD OD, No RAPD OS
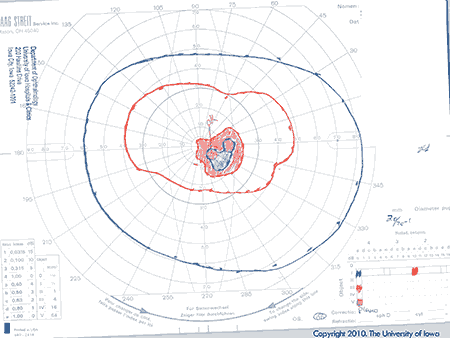 |
The patient was diagnosed with parameningeal embryonal rhabdomyosarcoma with extension into the posterior right orbit. High-dose steroids led to partial resolution of the optic nerve compression. Previous work up by Pediatric Hematology revealed no metastatic disease based on bone marrow biopsy, CSF cytology, and bone scan. PET scan showed increased radiotracer uptake in the right ethmoid air cell and sphenoid sinus lesion, consistent with a malignant lesion and regional lymph node involvement. Based on these features, the patient was classified as having Group III Stage 3 T2bN1Mo disease and stratified to the Intergroup Rhabdomyosarcoma Study (IRS) intermediate-risk group.
| Low risk | Stage 1: Clinical Groups I and II and N0. All favorable sites (orbit and head/neck, nonparameningeal, genitourinary tract, nonbladder prostate) Stage 1: Clinical Group III, N0 and NX. Orbit only Stage 2: Clinical Group I, N0 and NX. All other (unfavorable sites, tumor < 5cm in widest diameter |
|---|---|
| Intermediate risk | Stage 1: Clinical Group II, N1. All favorable sites (see above) Stage 1: Clinical Group III, N0, NNX1 and N1. All favorable sites except orbit Stage 2: Clinical Group II and III, N0, NNX1 or N1. All other sites Stage 3: Clinical Group II and III, N0, NNX1 or N1. All other sites |
| High-risk protocol | Stage 4: Clinical Group IV, N0, NNX1 or N1. Any site with metastatic disease, including tumor cells in CSF, pleural, or peritoneal fluid or omental implants |
 |
Rhabdomyosarcoma (RMS) is typically a malignancy of childhood comprising 5% of all childhood malignancies and 20% of all childhood soft tissue malignancies (Shields and Shields 2003). There are approximately 250-300 new cases diagnosed each year in the United States (Hayes-Jordan and Andrassy 2009). The average age of presentation is 8 to 10 years old. There is a slight male to female predominance (5:3) and no known predilection for race. Ocular RMS can be primary, secondary, or rarely metastatic; it arises from undifferentiated, pluripotent mesenchymal elements. Forty-five percent of all cases of RMS arise in the head and neck. Of these, 25-35% arise in the orbit (Shields and Shields 2003). It is one of the few life threatening diseases that may initially present to an ophthalmology clinic. Additionally, diagnosing the condition at an earlier stage and prompt initiation of treatment have been associated with more favorable outcomes (Shields et al. 2001). Thus, it is crucial for ophthalmologists to promptly recognize and accurately diagnosis this malignancy.
The presenting symptoms of ocular RMS include: proptosis (80-100%), globe displacement (80%), blepharoptosis (30-50%), conjunctival and eyelid swelling (60%), palpable mass (25%), and pain (10%) (Shields and Shields 2003). Although trauma does not cause RMS, it is not unusual for a patient to present with a history of recent injury preceding the ocular or orbital findings. RMS must be considered in all patients, particularly children, who present with proptosis. Decreased visual acuity tends to be a late clinical finding, and consequently, indicative of advanced disease. Initial work-up includes imaging—CT, MRI, or both—which subsequently guides surgical planning for incisional versus excisional biopsy. Final diagnosis is based on histopathology. Fine needle aspiration does not produce enough tissue to make an adequate histopathologic diagnosis. There are four histopathologic subtypes of RMS: embryonal, alveolar, pleomorphic, and boytroid (Holds et al. 2010). Embryonal RMS is associated with a 94% survival rate and accounts for 80% of orbital RMS. Contrariwise, alveolar RMS is the most malignant subtype (with a 10% 10-year survival rate) and comprises 9% of orbital RMS. Pleomorphic RMS is the least common and the most differentiated form; it is most commonly found in adults. Boytroid RMS is a rare variant of embryonal RMS and is not found as a primary tumor of the orbit (Holds et al. 2010). Histopathologic diagnosis of RMS requires immediate involvement of a pediatric hematologist/oncologist to further guide evaluation and management. A complete work-up includes: labs, bone marrow biopsy, bone scan, PET scan, CT of the chest/abdomen/pelvis, and cerebral spinal fluid analysis with cytology when applicable (Hayes-Jordan and Andrassy 2009).
Most of the data regarding the treatment of ocular RMS are gleaned from the Intergroup Rhabdomyosarcoma Study Group (IRS Group) that began in 1972 to investigate the therapy and biology of RMS and undifferentiated sarcoma in previously untreated patients who were less than 21 years old. Since then, five successive clinical protocols (four large clinical trials and one pilot study) involving almost 5,000 subjects have been completed. Treatment is based on pre-surgical staging combined with post-surgical grouping. Staging is based on: primary tumor site, primary tumor size, clinical regional node status, and distant spread. Interestingly, RMS is the only malignancy where staging includes the anatomic site of tumor origin. Grouping is based on pre-treatment and operative outcomes including: final pathologic verification of margins, residual tumor, node involvement, and cytological examination of fluid when applicable. Treatment includes a combination of surgery, chemotherapy, and radiation based on the previously mentioned IRS groups which divide patients into low-risk, intermediate-risk, and high-risk groups.
Origin in the orbit has the most favorable prognosis of any anatomic site. While nearly 35 years ago orbital RMS was associated with a 30% survival rate (Shields et al. 2001), data based on IRS trials I, II, III, and IV show a current survival rate of 93% (Kodet et al. 1997; Shields and Shields 2003). The significant increase in the survival rate of orbital RMS has been mostly attributed to earlier diagnosis and treatment than in the past.
Epidemiology
|
Signs
|
Symptoms
|
Treatment
*Based on IRS Clinical Trial V risk groups, see Table 1 |
Shields JA, Shields CL. Rhabdomyosarcoma: Review for the Ophthalmologist. Surv Ophthalmol 2003; 48(1):39-57.
Hayes-Jordan A, Andrassy R. Rhabdomyosarcoma in children. Curr Opin Pediatr 2009; 21(3):373-378.
Shields CL, Shields JA, Honavar SG, and Demirci H. Clinical spectrum of primary ophthalmic rhabdomyosarcoma. Ophthalmology 2001; 108:2284-2292.
Holds JB, Chang WF, Dailey RA, Foster JA, Kazim M, and McCulley TJ. Orbit, Eyelids, and Lacrimal System. Section 7, Basic and Clinical Science Course. San Francisco: American Academy of Ophthalmology; 2010; Chapter 5, p.78-81.
Kodet R, Newton WA Jr, Hamoudi AB, et al. Orbital rhabdomyosarcoma and related tumors in childhood: relationship of morphology to prognosis—an intergroup rhabdomyosarcoma study. Med Pediatr Oncol 1997; 29:51-60.
Saylor MA, Allen RC. Rhabdomyosarcoma: Eleven-year-old male with two weeks of blurry vision and headaches. EyeRounds.org. December 8, 2010. Available from https://eyerounds.org/cases/127-Rhabdomyosarcoma.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.