Chief Complaint: 17-year-old male presents for surgical treatment of longstanding left exotropia
History of Present Illness: This patient has a longstanding sensory left exotropia and is interested in strabismus surgery. His left eye has turned out since birth. He thinks that patching was attempted when he was younger. However, he thinks the patching was not successful, because of his non-compliance as a child.
Past Ocular History: Left amblyopia and left sensory exotropia
Medical History: Sinusitis and seasonal allergies
Medications: None
Allergies: No known drug allergies
Family History: Mother has a history of strabismus surgery. His paternal grandmother has diabetes.
Social History: Quit smoking 3 months ago. Smoked ½ pack per day for 7 years He is attending a state school for boys due to delinquent behavior.
Physical Exam: General: well-appearing patient with no acute distress
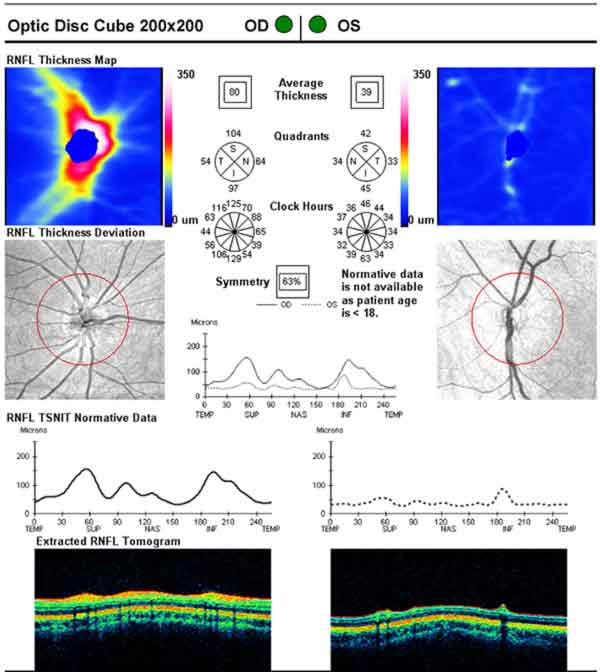
Clinical Course: Refraction did not improve his visual acuity. Optic nerve optical coherence tomography (OCT) was obtained (figure 2). An MRI of the brain was obtained to rule out midline abnormalities, given his behavioral issues. The study demonstrated a hypoplastic left nerve and tract (figure 3 and 4). Otherwise normal cerebrum and cerebellum, with no midline intracranial abnormalities. The pituitary gland was present. He underwent a left medial resection and left lateral recession with an adjustable suture. Initially, his ocular alignment measured 15 prism diopters of esotropia and 2 months later measured 5 prism diopters exotropia. The patient was happy with the outcome.
 |
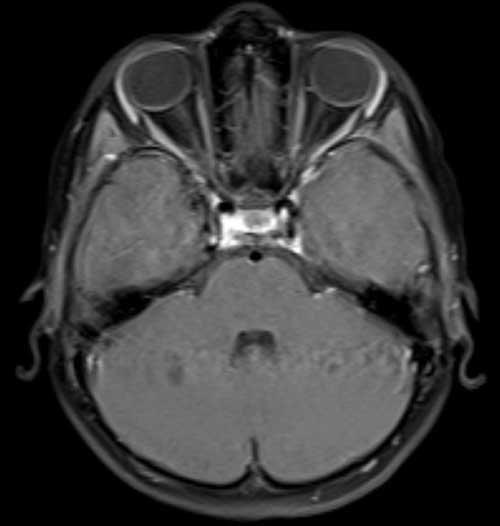 |
Optic nerve hypoplasia is a rare congenital disorder that may be an isolated finding or occur in association with another syndrome. There is an extremely wide range of severity: visual acuity in the affected eye(s) correlate to the severity of hypoplasia, falling anywhere between 20/15 to no light perception. Histologically, the retinal nerve fiber layer and ganglion cell number are decreased, while the outer retinal layer is unaffected.[1] Even if visual acuity is normal, patients with optic nerve hypoplasia can have visual field defects, most commonly in the nasal or inferior fields of vision.[2] It can be a bilateral (75% of cases[3]) or a unilateral finding and may be associated with absence of the septum pellucidum, thinning or absence of the corpus callosum, cerebral hemisphere abnormalities, anencephaly, and/or dysfunction with the hypothalamic-pituitary axis. Therefore brain imaging should be performed on all infants with a diagnosis of optic nerve hypoplasia.
Children with bilateral optic nerve hypoplasia more commonly have associated neurologic abnormalities (57%) when compared to children with unilateral optic nerve hypoplasia (32%). Failure of the retinal ganglion cell layer to differentiate is the main cause of optic nerve hypoplasia, although the true pathogenesis remains unknown.[1] A 2009 case study reported a patient found to have optic nerve hypoplasia and a pericentric inversion of upon chromosomal analysis.[4] Infants born to mothers with diabetes are at increased risk for optic nerve hypoplasia. Other known risk factors include quinine, phenytoin, or alcohol ingestion by the mother during pregnancy.
Infants with unilateral optic nerve hypoplasia with absent light perception in the affected eye usually present with strabismus and an afferent pupillary defect. For infants with bilateral optic nerve hypoplasia, they commonly present with a course, pendular nystagmus.[2,3] The classic finding in patients with optic nerve hypopasia is a decreased diameter of the optic disc. Other common findings with fundus examination include optic disc pallor, vascular tortuosity, and abnormalities in the retinal vasculature. Externally, patients may have microphthalmia, aniridia, or cranial nerve IV/VI palsies. In a chart review of 100 infants with optic nerve hypoplasia, 32% were developmentally delayed, 13% had cerebral palsy, and 12% had seizures.[3]
The optic nerve forms in human embryos at around 6 weeks gestation. Extension of the optic nerve fibers to the chiasm is complete by 8 weeks gestation.[2] Embryologic development of the corpus callosum and septum pellucidum occurs roughly at the same time as the optic nerve, hence the increased rate of coexisting anomalies. When optic nerve hypoplasia occurs with absence of the septum pellucidum, it is known as septo-optic dysplasia (de Morsier syndrome). Only about 10% of children with optic nerve hypoplasia have septo-optic dysplasia, and about 50% of these children have associated endocrine abnormalities.[3] Even though endocrine abnormalities are a rare finding in patients with optic nerve hypoplasia, all patients should be seen by an endocrinologist to rule out the possibility of potentially fatal endocrine complications such as sudden infant death due to thermoregulation problems, dehydration, and congenital hypothyroidism. The growth charts of patients with de Morsier syndrome should be monitored closely because of the potential for decreased release of growth hormone. Optic nerve hypoplasia can also be associated with cerebrohepatorenal syndrome of Zellweger, an extremely rare leukodystrophy characterized by decreased peroxisomes in renal, liver, and brain cells.[2]
Patients with unilateral optic nerve hypoplasia may have normal to severely diminished acuity. Those with poor vision may have strabismus. Treatment options include observation, a pirate patch, prism, corrective spectacles to minimize the appearance, and surgery. Primarily, the surgical site should be the affected eye and the surgeon should consider altering the standard surgical amount as patients with neurologic deficits do not have a normal response to surgery.[5,6]
Diagnosis: Optic Nerve Hypoplasia
EPIDEMIOLOGY:
|
SIGNS:
|
SYMPTOMS:
|
TREATMENT:
|
1. Zeki SM, Dutton GN: Optic nerve hypoplasia in children. The British journal of ophthalmology 1990, 74(5):300-304.
2. Ouvrier R, Billson F: Optic nerve hypoplasia: a review. Journal of child neurology 1986, 1(3):181-188.
3. Garcia ML, Ty EB, Taban M, David Rothner A, Rogers D, Traboulsi EI: Systemic and ocular findings in 100 patients with optic nerve hypoplasia. Journal of child neurology 2006, 21(11):949-956.
4. Cheung RT, Wong AM: Optic nerve hypoplasia associated with chromosome 9 inversion. Canadian journal of ophthalmology 2009, 44(5):610-611.
5. Pickering JD, Simon JW, Lininger LL, Melsopp KB, Pinto GL: Exaggerated effect of bilateral medial rectus recession in developmentally delayed children. Journal of pediatric ophthalmology and strabismus 1994, 31(6):374-377.
6. Habot-Wilner Z, Spierer A, Glovinsky J, Wygnanski-Jaffe T: Bilateral medial rectus muscle recession: results in children with developmental delay compared with normally developed children. J AAPOS 2006, 10(2):150-154.
Additional Reading
Floyd MS, Benson C, Longmuir SQ. Unilateral Optic Nerve Hypoplasia in a patient desiring surgical treatment for his exotropia. EyeRounds.org. August 30, 2011. Available from: https://eyerounds.org/cases/138-UnilateralOpticNerveHypoplasia.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.