Chief Complaint: Diplopia and proptosis of right eye
History of Present Illness: The patient is an 80-year-old male who presented to the Emergency Department with complaints of sudden vision loss in the right eye (OD). His symptoms began that morning with diplopia when he left home to walk his dog. By the time he returned home, he had profound vision loss OD and his wife noticed his right eye was protruding. The patient denied associated pain, headache, tinnitus or nausea. He denied a history of spontaneous bleeding or recent head trauma. He was seen by an outside emergency department where his intraocular pressure OD was found to be 60mmHg and he was no light perception (NLP) with a large relative afferent pupillary defect (RAPD) by reverse OD. A lateral canthotomy and inferior cantholysis were performed at the outside hospital. He received a dose of intravenous mannitol and was subsequently transferred to our hospital emergency department for further management.
Past Ocular History: Bilateral posterior chamber intraocular lens placement
Past Medical History:
Medications:
Family History: Heart disease, type I diabetes mellitus, no known history of stroke
Social History: Drinks three glasses of wine daily
Review of Systems: Positive for nausea and vomiting thought to be associated with increased intraocular pressure. Negative for coughing or history of straining.
Vital signs:
Ocular Exam:
Labs: Normal complete blood count, Prothrombin time, Partial Prothrombin Time and International Normalized Ratio (PTT and INR)
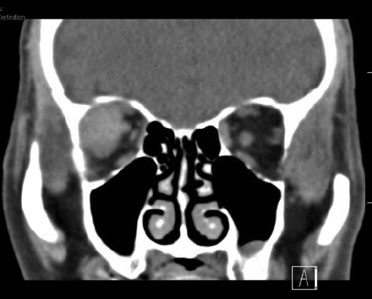
Course: A computed tomography (CT) scan demonstrated a right lateral extraconal well-demarcated mass and proptosis OD (Figure 1). A diagnosis of spontaneous retrobulbar hemorrhage was made due to the rapid onset of symptoms, presence of an extraconal lesion consistent with a hematoma on CT and moderate proptosis. CT angiography was performed and was negative for AV malformation, varix, or other vascular abnormality. Serial intraocular pressure (IOP) checks were performed and the IOP increased into the 40s with return of symptoms of nausea. We performed a complete right inferior and superior cantholysis and his IOP subsequently came back down to 30mmHg with improvement of nausea. His central retinal artery remained perfused. He received 250mg IV acetazolamide as well as repeat doses of topical dorzolamide/timolol and brimonidine. He was admitted overnight for observation and discharged home on brimonidine and dorzolamide/timolol twice daily, OD. One week later the patient was again seen in the emergency room for right sided headache and nausea. His visual acuity OD was 20/320 and IOP OD was 18mmHg. Repeat CT showed mild enlargement of the hematoma with increased medial buckling of the right optic nerve (Figure 2). No immediate intervention was performed and the patient followed up in the oculoplastics clinic three days later. The patient's visual acuity was 20/125 OD and a central scotoma OD was found on Goldmann visual field test suggesting optic nerve compression (Figure 3). A right lateral orbitotomy was performed two days later with drainage of the hematoma. One month later during clinic follow-up his visual acuity was 20/25 OD with a full visual field on repeat Goldmann visual field testing (Figure 4).
 |
 |
|
|
|
Orbital compartment syndrome refers to the situation in which the orbital pressure is elevated due to a space occupying lesion within the orbit, which is a closed compartment. An orbital hemorrhage is the most common cause of orbital compartment syndrome, which is usually due to trauma, surgery, retrobulbar injection or patient comorbidities. In our patient's case, the cause was considered to be a spontaneous retrobulbar hemorrhage possibly exacerbated by increased use of aspirin. Orbital compartment syndrome can also be caused by orbital cellulitis, abscess, inflammation, air or tumors. Depending on the etiology different orbital spaces may be affected. Visual loss occurs when the elevation of orbital pressure causes a decrease in central retinal artery perfusion or compression of the long and short posterior ciliary arteries resulting in retina and optic nerve ischemia respectively. Increased orbital pressure can also cause vision loss secondary to central retinal vein occlusion or compressive optic neuropathy.[1]
Diagnosis is clinical and should be suspected in patients presenting with acute proptosis, rapid vision loss, ophthalmoplegia and fixed dilated pupils or RAPD, especially if there is recent trauma.[1,2] Perfusion of the central retinal artery can be assessed by applying digital pressure to the globe and evaluating how much pressure is required to occlude the artery. If the central retinal artery is not perfused or can be compressed with minimal digital pressure the IOP must be decreased until the retina is perfused. Orbital imaging is indicated to aid in the diagnosis. CT is preferred over MRI because it can be rapidly done. One study suggests that increased distance from the globe to the orbital apex and degree of tenting of a stretched globe of the affected proptotic eye on CT scan can be helpful in predicting vision loss.[3]
If an orbital compartment syndrome is compromising blood flow to the optic nerve or central retinal artery, it is important to lower the IOP in these patients quickly - if you are entertaining the idea of a canthotomy/cantholysis, better to do it sooner than later. One must remember that just 90 minutes of elevated pressure can cause permanent vision loss due to decreased perfusion of the optic nerve making prompt recognition and treatment imperative.[4]
IOP can be reduced by increasing the volume of the orbit in conjunction with ocular hypotensive medications, such as timolol, dorzolamide, brimonidine, and oral/IV acetazolamide. There is some evidence that adjuvant use of intravenous corticosteroids and mannitol may be helpful in lowering intraocular pressure and preventing vision loss, although we do not routinely use these in our institution.[4] The fastest and most commonly used method to increase the volume of the orbit is by performing a lateral canthotomy with inferior and superior cantholysis (http://www.EyeRounds.org/tutorials/lateral-canthotomy-cantholysis.htm). This results in the anterior extent of the orbit no longer being confined by the eyelids. By releasing the eyelids, the eye can "come forward". Often only an inferior cantholysis is enough to decrease the pressure, but addition of a superior cantholysis can allow for more decompression if needed. In general, a lateral canthotomy with cantholysis is painful in the acute setting because the tissues are inflamed, which limits the diffusion of local anesthetics. Failure to decrease the pressure is often due to incomplete cantholysis of the upper and lower lateral canthal tendons. Some advocate making a full thickness cut through the central upper and lower lids if one is unable to confidently perform an adequate canthotomy/cantholysis. Others advocate releasing the orbital septum of the lower lid with scissors in addition to the canthotomy/cantholysis. If the pressure does not improve to the point that the optic nerve is perfused with the above interventions, an orbital decompression should be performed. A floor decompression can potentially be performed in the acute setting with a hemostat; however, a controlled decompression of the medial wall and orbital floor would be preferable if time permits.
Repair of a canthotomy/cantholysis can be performed on an elective basis. Often, patients will heal well without the need of repair. We usually wait 2-4 weeks before repair. Additionally, patients should be instructed to avoid nose blowing and Valsalva, such as coughing or straining which could make a hemorrhage worse.
Our patient is interesting in that he had a persistent orbital compartment syndrome even after his intraocular pressure normalized. His central retinal artery remained perfused the entire time. The GVF showed a central scotoma and he had an RAPD which was more consistent with optic nerve compression, rather than retinal damage due to non-perfusion. Due to this, we elected to drain the hematoma which resulted in rescue of his vision. Perhaps the resilience of his central retinal artery was due to high systemic systolic pressures or a relatively quick improvement in his IOP after presentation.
Orbital Compartment Syndrome secondary to spontaneous retrobulbar hemorrhage
Epidemiology:
|
Signs:
|
Symptoms:Acute onset:
|
Treatment:
|
McAllister AR, Sobel RK, Allen RC. Spontaneous Retrobulbar Hemorrhage with Subsequent Orbital Compartment Syndrome. EyeRounds.org. April 18, 2013; Available from: http://www.EyeRounds.org/cases/168-Orbital-Compartment-Syndrome.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.