Several new choroidal nevi
An 89-year-old male was referred to the University of Iowa retina service for evaluation of multiple choroidal nevi which were noted incidentally almost a year after starting intravitreal ranibizumab and aflibercept for exudative age-related macular degeneration. He had no known history of cancer, but was formerly a heavy smoker.
He reported anorexia, an unintentional weight loss of 30 pounds over the prior 6 months, and a mild chronic cough. In the month prior to his ocular examination, a colonoscopy and upper endoscopy were performed and were normal with the exception of diverticulosis.
|
Right (OD) |
Left (OS) |
|---|---|---|
Visual Acuity |
20/30-2 |
20/25+1 |
Pupils |
No afferent pupillary defect |
No afferent pupillary defect |
Visual Fields |
Full |
Full |
Extraocular Motility |
Full |
Full |
Tonometry |
10 mmHg |
12 mmHg |
Amsler Grid |
Normal |
Normal |
Slit lamp exam |
|
|
Lids/Lashes |
Marked lower lid ectropion |
Mild lower lid ectropion |
Conjunctiva/Sclera |
Dilated episcleral vessels but no abnormal pigment |
Dilated episcleral vessels but no abnormal pigment |
Cornea |
Clear |
Clear |
Anterior chamber |
Deep and quiet |
Deep and quiet |
Iris |
Normal architecture |
Normal architecture |
Lens |
Intraocular lens |
Intraocular lens with 1+ posterior capsular opacification |
Vitreous |
Posterior vitreous detachment; no anterior vitreous cells |
Posterior vitreous detachment; no anterior vitreous cells |
Fundus |
See Figure 1 |
See Figure 1 |
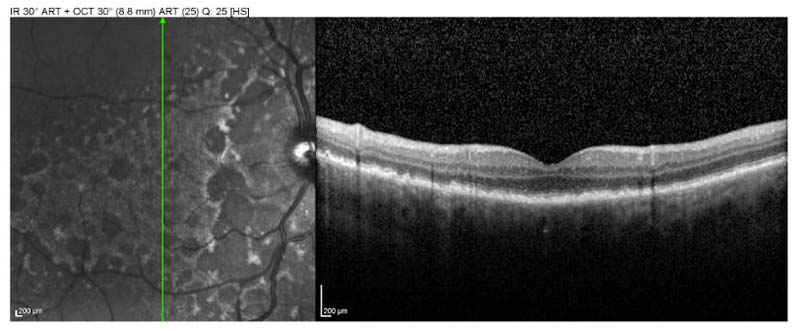 |
| Right eye |
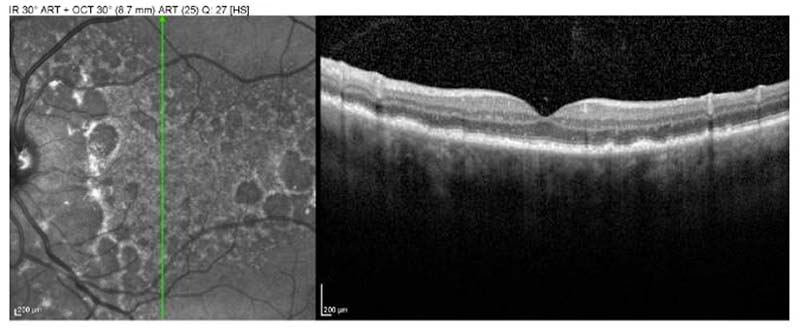 |
| Left Eye |
The patient was diagnosed with bilateral diffuse uveal melanocytic proliferation (BDUMP). Multiple choroidal nevi in the presence of chronic cough and unintentional weight loss in a former smoker were highly suspicious for possible malignancy; consequently the patient underwent a metastatic evaluation. The evaluation revealed Stage 3B adenocarcinoma of the lung. Unfortunately, his lung cancer progressed despite treatment and eventually chemotherapy was discontinued. He continued to receive bilateral anti-VEGF injections for exudative age-related macular degeneration, and had stable to improved visual acuity 7 months after presentation (20/30-2 OD and 20/20 OS). Ten months after his original presentation to the eye clinic, his vision had mildly decreased in each eye to 20/40. One month later, he died.
Bilateral diffuse uveal melanocytic proliferation (BDUMP) is a rare paraneoplastic syndrome resulting in severe vision loss and benign proliferation of choroidal melanocytes. The melanocytes are histopathologically unrelated to the non-ocular tumor. The condition was first reported in 1966 by Machemer, and there are approximately 31 reported cases in the literature (1-3,8).
Typically, BDUMP presents as bilateral vision loss in an adult patient between the ages of 50 and 80 years old. In 85% of cases, pigmented choroidal lesions are observed. Bilateral exudative retinal detachment and rapid cataract formation often follow the initial vision loss. Surgical removal of cataracts and resolution of associated retinal detachment with treatment of systemic malignancy may improve vision to a limited degree (if these conditions are present), but patients nonetheless have a very guarded prognosis as a result of the presence of systemic malignancy. The etiology of retinal detachment is unclear, but it is thought that a poorly-functioning retinal pigment epithelium (RPE) and breakdown of the blood-retina barrier are involved. The etiology of rapid cataract formation (as rapid as 3 months) has been hypothesized to result from ciliary body involvement, leading to inadequate aqueous volume, poor nutrient composition, or release of toxins (1).
In nearly half of the cases of BDUMP there is a history or known diagnosis of non-ocular malignancy at the time of diagnosis of BDUMP (2). In the other half of cases, the primary systemic malignancy is discovered subsequent to the diagnosis of BDUMP, as was the case in our report. BDUMP is associated with multiple visceral cancers including lung, colon, pancreatic, gallbladder, ovarian, uterine, and cervical. Gynecologic cancers (i.e. ovarian carcinoma) are the most prevalent systemic tumors associated with BDUMP in women. In men, the most frequent causative cancers are pancreatic and lung. BDUMP has no known gender predilection (1).
The pathogenesis of BDUMP is currently unknown; however, a feature that may point to its pathogenesis is the development of hyperpigmentation at other, non-ocular sites in the body. Approximately 26% of BDUMP patients have pigmented lesions of the skin and mucous membranes. In addition, acanthosis nigricans is associated with many of the same visceral adenocarcinomas that occur with BDUMP. As such, one hypothesis for the pathogenesis of BDUMP is that the primary non-ocular tumor releases endocrine factors which lead to proliferation of uveal melanocytes and systemic hyperpigmentation. This idea has biologic plausibility, because the cancers known to cause BDUMP are tumors that are well-known to cause other paraneoplastic syndromes through factor release. In addition, certain BDUMP patients have simultaneous development of paraneoplastic states such as hypercoagulability and hypercalcemia (1).
Another hypothesis for the pathogenesis suggests that anti-retinal autoantibodies may be in part responsible for destruction of photoreceptors (1,3).
Gass in 1990 (6) described the five cardinal ocular signs that accompany vision loss in patents with BDUMP:
The differential for BDUMP includes choroidal metastases of skin melanoma and choroidal nevi associated with neurofibromatosis I (7). BDUMP should be considered in the differential of patients with pigmented fundus lesions, especially when presenting bilaterally, with bilateral vision loss, and a history of non-ocular tumors (2).
Though BDUMP has a clinical presentation similar to uveal melanoma, the two may be easily distinguished because choroidal melanoma is typically focal and dome or mushroom-shaped. Diffuse choroidal melanoma is more similar to BDUMP, but does not involve the entire uveal tract and is unilateral (1).
The presentation of bilateral vision loss is antecedent to the discovery of a primary non-ocular tumor in nearly half the cases (2). The vision in BDUMP patients typically progresses to legal blindness within 1 year of presentation. Survival following the diagnosis of BDUMP is between 8 and 24 months (1,2) and the majority die within three years (7). Death typically occurs due to complications from the underlying systemic malignancy. Management of BDUMP must include extensive workup for occult malignancy and repeated screenings until the underlying malignancy is found.
In the past, treatment for BDUMP involved bilateral enucleation due to the concern for uveal melanoma. External beam radiation has also been used in the past (due to concern for melanoma) without any significant improvement. These therapies are no longer employed. Other therapies including drainage of subretinal fluid and corticosteroids have also been attempted, but failed to demonstrate any significant improvement. (1,3,7,8,10) There is one case in the literature of a patient's exudative retinal detachment improving with periorbital corticosteroid injection (9) but that treatment modality has not been replicated again in the literature.
More recently, plasma exchange (PE) has been suggested as a potential therapeutic approach for BDUMP. Although the mechanism of BDUMP is not yet known, several reports have shown improved visual acuity, resolution of subretinal fluid, and decreased choroidal thickening with the use of PE (3,7,8). Unfortunately, frequent courses of plasma exchange are associated with the possibility of immunosuppression and relapse after PE is completed. Because it is thought by some that BDUMP represents an autoimmune response to cancer, suppression of the response may trigger cancer growth (7,8).
There is some controversy as to the benignity of the melanocytic proliferation seen in BDUMP. Most cases report benign-appearing spindle-shaped cells on histopathology; however, some case reports show the presence of enough malignant melanocytes for a diagnosis of melanoma (4). One study done by Margo (5) showed a lack of p53 immunoreactivity after immunostaining of eight eyes with BDUMP. Since p53 overexpression is common in malignancies such as uveal melanoma, it appears that the melanocytic proliferation in BDUMP may be through a different mechanism. There is no report in the literature of metastasis of uveal tumors seen in BDUMP.
Our case is atypical, due to the preservation of good visual acuity for months after the diagnosis. The use of anti-VEGF agents has not been reported in the literature for the treatment of exudative RD in BDUMP. Consequently, it is not known whether the anti-VEGF therapy the patient received for his exudative AMD may have improved the outcome for his BDUMP. Indeed, his bilateral macular edema, subretinal fluid, and irregularly elevated RPE may have actually been the earliest manifestations of his BDUMP rather than manifestations of exudative AMD.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Hayes JR, Welder JD, Boldt HC. Bilateral Diffuse Uveal Melanocytic Proliferation (BDUMP): 89-year-old male presents with multiple choroidal nevi, both eyes. Dec 7, 2014; Available from: https://eyerounds.org/cases/197-BDUMP.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.