Chief Complaint: Referral for cystoid macular edema
History of Present Illness (HPI): A 12-year-old male was referred to the pediatric ophthalmology clinic after being diagnosed with cystoid macular edema at an outside eye clinic. The patient had been participating in baseball when his parents noticed that he was losing track of flyballs more frequently and struggling with accuracy in the batting cages. Initially, the patient received corrective lenses, but his vision did not improve. Subsequently, he was referred to an ophthalmologist who diagnosed him with cystoid macular edema and referred him to the pediatric genetic eye service. The patient denies experiencing any concerns with his vision, photophobia, or pain, but recalls noticing "floaters" described as "little strings."
Past Ocular History
Past Medical History
Medications
Allergies
Social History
Family History
OCULAR EXAMINATION
| Sphere | Cylinder | Axis | |
|---|---|---|---|
| Right | +0.75 | +0.50 | 108 |
| Left | +1.50 | +0.50 | 115 |
| OD | OS | |
|---|---|---|
| Lids/Lashes | Normal | Normal |
| Conunctiva/Sclera | Clear and quiet | Clear and quiet |
| Cornea | Clear | Clear |
| Anterior Chamber | Deep and quiet | Deep and quiet |
| Iris | Normal architecture | Normal architecture |
| Lens | Clear | Clear |
| OD | OS | |
|---|---|---|
| Disc | Normal | Normal |
| Macula | Blunted foveal reflex | Blunted foveal reflex |
| Vessels | Normal | Normal |
| Periphery | Normal | Normal |
DIAGNOSIS: Juvenile X-Linked Retinoschisis (JXLR)
CLINICAL COURSE
Juvenile X-linked Retinoschisis was provisionally diagnosed, prior to genetic testing, based on the patient’s initial presentation, which was supported by the presence of schisis on optical coherence tomography (OCT). The patient was started on dorzolamide 2% ophthalmic solution, administered three times daily, and was advised to prioritize eye protection during sports or activities that could pose a risk of eye injury, due to the potential risk for vitreous hemorrhage and retinal detachment. The patient underwent regular follow-ups every 6 months with OCT imaging used to monitor cystic changes. Additionally, more family history was discovered, revealing that the patient's three male cousins and great-uncle were also affected by the condition.
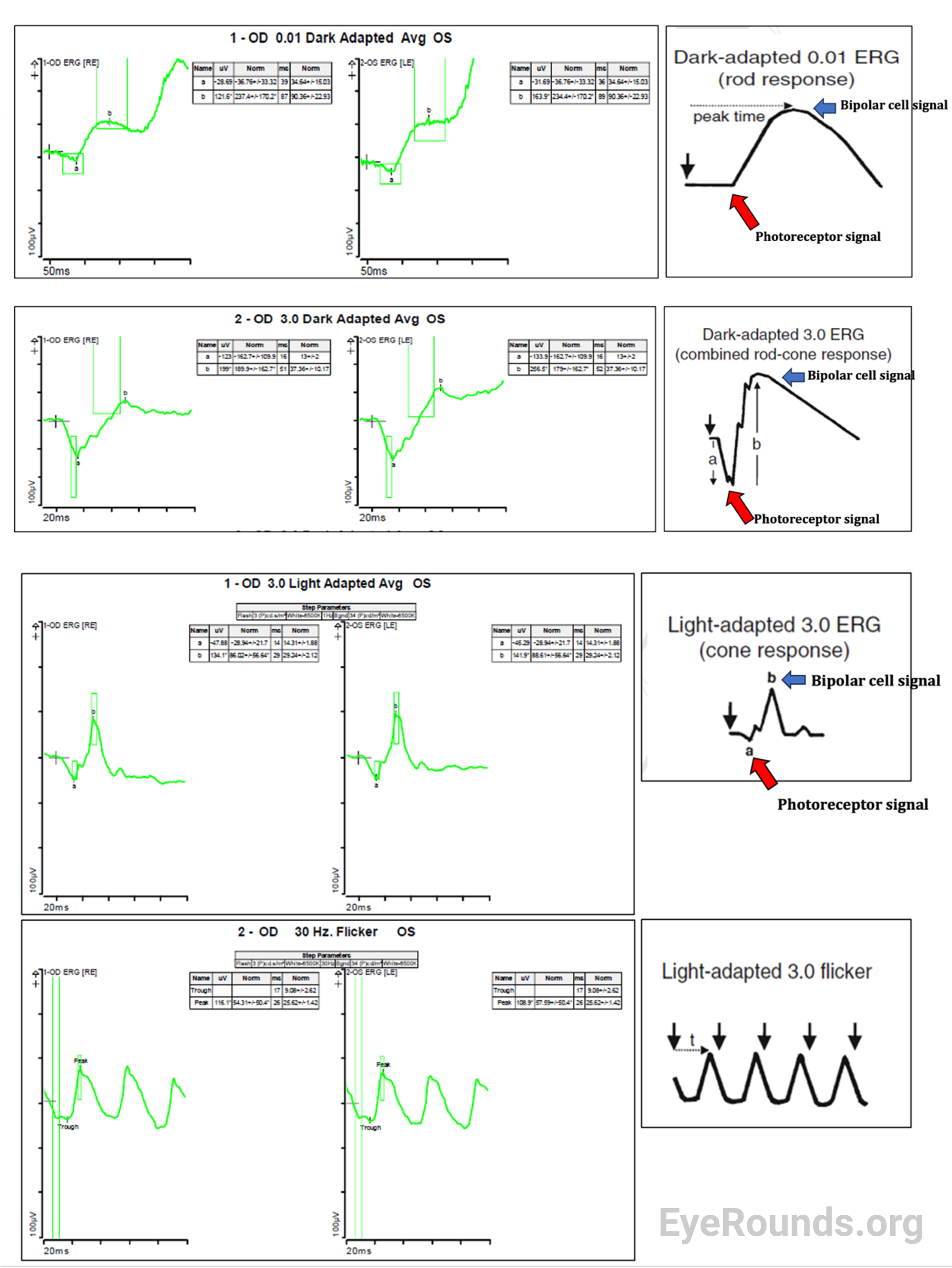
Electroretinograms (ERGs) were repeated four years after initial diagnosis and conducted on the same equipment with similar electrodes. Results showed relatively stable to slightly decreased dark adapted ERG waveforms (Dark adapted 0.01 stable OU, Standard combined response b-wave decreased 37% OD and 13% OS, a-wave increased 12% OD and 27% OS) from 2018. (Figure). Newly collected light adapted ERG waveforms showed decreased amplitudes in all test conditions (Light adapted 3.0 b-wave decreased 13% OD and 11% OS, a-wave decreased 15% OD and 29% OS, 30 Hz Flicker decreased 25% OD). ERG amplitudes may vary by up to 25% in normal retinas between sessions.
OCT imaging four years after initial presentation demonstrated an increase in both the number and size of cysts in the right eye. The left eye had increased retinal thickness but improved vision. No retinal detachment or tear was detected in subsequent fundus photos.
The patient and family were informed of potential risks of even mild ocular trauma, which could result in vitreous hemorrhage or retinal detachment. As a precautionary measure, the use of sports goggles was strongly recommended for any contact sports. The patient reported successful eye protection by using women's lacrosse goggles, which fit snugly to the face and are worn under special wrestling headgear during practices and matches. Subsequently, over several years of wrestling while wearing these goggles, no significant eye injuries were sustained.
DISCUSSION
Juvenile X-linked Retinoschisis (JXLR) is a genetic vitreoretinal disorder that affects many males worldwide, with an estimated prevalence of 1 in 5,000 to 20,000.[1] JXLR is the most common cause of macular dystrophy in young men and can result in significant visual impairment and vision loss. The underlying mechanism of JXLR is the absence or reduced function of a protein called retinoschisin, a 224 amino acid protein which is encoded by the RS1 gene on the X chromosome (Xp22.1-p22.3). Over 200 causative mutations in the RS1 gene have been identified, and 40% of RS1 mutations result in a null protein, which is associated with more severe disease.[2] Although JXLR is typically observed in males due to the recessive X-linked inheritance pattern, females can also be affected in rare cases if they inherit two affected X chromosomes.
Retinoschisin is predominantly secreted by retinal photoreceptors and bipolar cells, playing a pivotal role in mediating cell-cell interactions through its conserved discoidin domain.[3,4] This interaction establishes the foundational structural scaffolding of the retinal architecture. The absence of a functional RS1 protein disrupts the regular adhesion between retinal layers, ultimately resulting in the emergence of fluid-filled cavities or cysts within the retina, which is referred to as retinoschisis. These cysts typically manifest in the inner nuclear layer, creating a spatial division between the outer plexiform and inner plexiform layers of the retina. This disruption notably interferes with the normal transmission of signals within the retina, impeding efficient retinal signal transmission.[5,6] In summary, the loss of a normally functioning RS1 gene, and subsequently the retinoschisin protein, appears to lead to the loss of retinal layer adhesion. Retinoschisis can cause severe, bilateral vision loss from macular atrophy, vitreous hemorrhage, retinal detachment, and/or amblyopia in pediatric patients.[3,4] Foveal involvement is routinely demonstrated in essentially all affected patients, whereas peripherally located schisis is observed in up to 50 percent of patients.[4]
Children typically present with JXLR during elementary school, often due to vision difficulties. However, the disease has been detected as early as infancy, primarily through the observation of nystagmus or strabismus, and subsequent identification of cysts via OCT. The severity of the disease course is generally greater with earlier presentations. Significant variation in disease severity exists, partially due to the high number of mutations that contribute to the disease; however, even within families with the same mutation, variance in expressivity can be observed.[7]
Examination and Diagnostic Testing
A foveal spoke wheel lesion, which is characteristic of foveal schisis, can be observed in some patients on 90 diopter slit lamp exam, direct ophthalmoscopy, or fundus photography. On OCT imaging, schisis can be seen in the inner retinal layers, particularly the inner nuclear layer in the macula.
The stereotypical ERG phenotype associated with JXLR is the electronegative b-wave. Electronegative b-waves occur when the amplitude of the b-wave is so reduced, that it is below the baseline in the 3.0 Dark adapted protocol, producing a reduced b/a ratio. However, these findings are only present in around 50% of patients, therefore a normal ERG does not rule out a diagnosis of JXLR and should not be used as diagnostic criteria, but rather as supportive evidence for genetic testing.3 The super-bright DA 10.0 flash may elicit electronegativity even when it is not demonstrable on standard DA 3.0 testing. The electronegative b-wave is illustrated in the figure below.
Treatment/Management
Carbonic anhydrase inhibitors (CAI) such as brinzolamide or dorzolamide are the primary medical treatment for JXLR, and they have demonstrated efficacy in reducing intraretinal cyst formation in some patients.[8,9] However, the benefits of CAIs may be short-lived and it is not known whether the use of CAIs prevents the long-term progression of the disease. Moreover, the use of CAIs carries the risk of rebound cyst formation and intraocular pressure if treatment is suddenly discontinued. There are limited studies demonstrating the long-term efficacy or safety of CAIs in JXLR patients. One study found that use of topical CAIs leads to a significant improvement in visual acuity and reduction in intraretinal cysts in most patients.[10] Recent research has suggested that adherence to CAI treatment can be challenging in pediatric patients and may require involvement of a caregiver. The exact mechanism of how CAIs improve vision is not well understood, but they have been shown to improve visual acuity and, to a lesser extent, central macular thickness. Interestingly, visual acuity improvement has been observed in pediatric patients even without cyst resolution on OCT.[10,11]
In the management of Juvenile X-linked retinoschisis, affected children are commonly advised to avoid sports or high-contact activities due to the heightened risk of vitreous hemorrhage or retinal detachment, which can worsen vision loss even with mild to moderate ocular trauma. However, as demonstrated in this case report, regular use of properly fitting sports goggles during contact sports may prevent injury for many patients. It is important to note that retinal detachment and vitreous hemorrhage can still occur even in the absence of trauma and may require surgical intervention.
Gene therapy research involving mouse models with a nonfunctional RS1 gene is currently ongoing, and preliminary results have shown promising outcomes in mouse cohorts. Two human trials have been initiated utilizing AAV vectors to deliver a normal copy of the gene to the vitreous. However, these human trials have reported adverse ocular outcomes, including inflammation, which need to be further investigated and addressed for the safe and effective implementation of gene therapy for JXLR.[12,13]
Differential Diagnosis
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Gehrke E, Strampe MR, Drack AV. Diagnosis and management of Juvenile X-linked Retinoschisis (JXLR). EyeRounds.org. Posted December 5, 2023; Available from https://EyeRounds.org/cases/354-Morning-Glory-Disc-Anomaly.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.