Chief Complaint: Three weeks of left eye pain
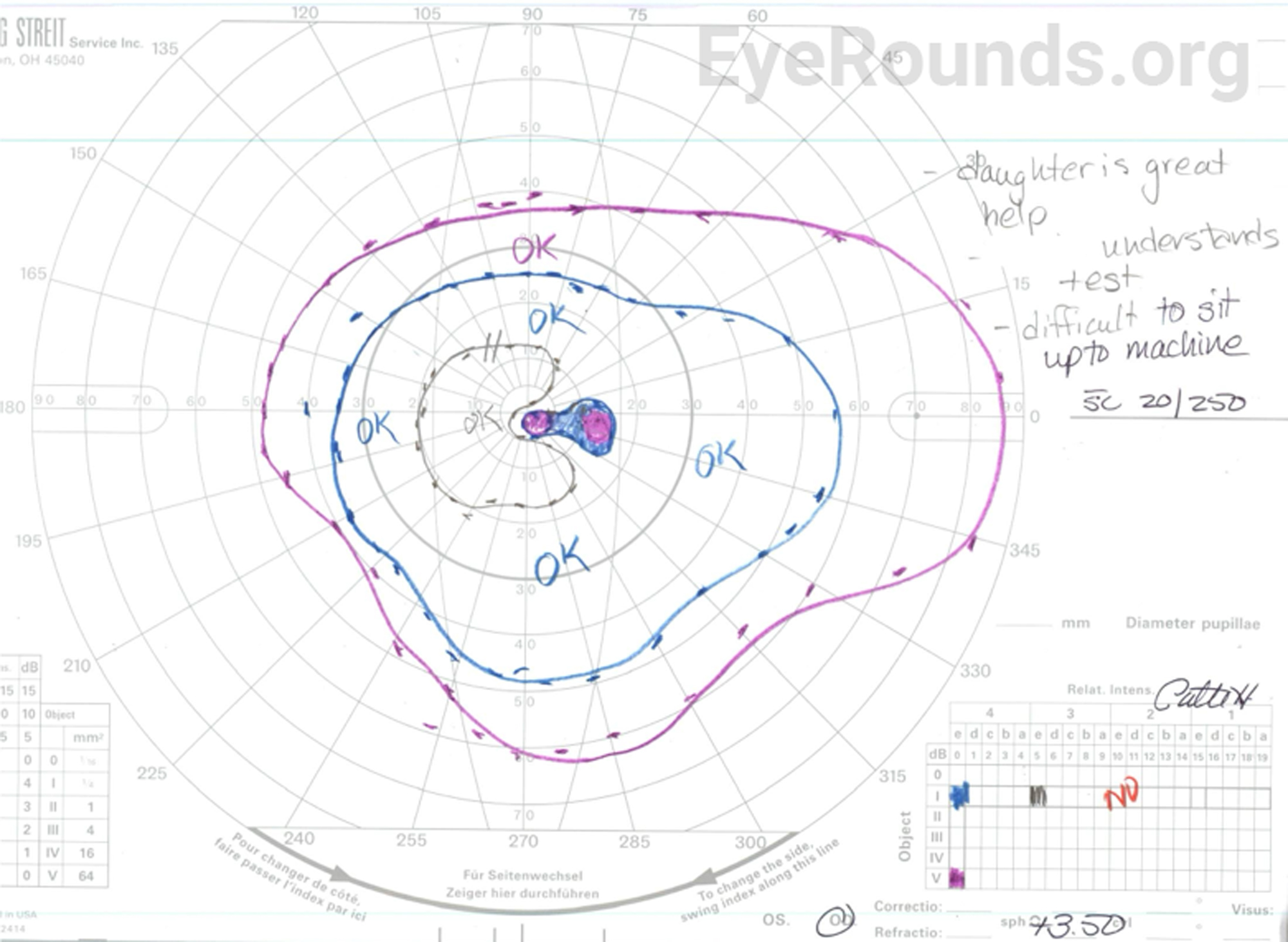
History of Present Illness (HPI): A 64-year-old Congolese female who followed with the University of Iowa Neuro-Ophthalmology service for optic neuropathy of unclear etiology returned for regular follow-up. She endorsed three-weeks of left eye pain and reported seeing a worm writhing beneath the conjunctiva of her left eye (Video 1, Figure 3), but it had since disappeared. She denied ongoing eye pain. She additionally reported progressive bilateral vision loss.
Past Ocular History
Past Medical History
Medications
Allergies
Family History:
Social History:
Review of Systems:
OCULAR EXAMINATION
| OD | OS | |
|---|---|---|
| External | Normal | Normal |
| Lids/Lashes | Normal | Normal |
| Conunctiva/Sclera | Nasal pterygium and temporal pinguecula, complexion-associated melanosis, 1+ diffuse injection, no subconjunctival worm observed | Nasal and temporal pterygia, complexion-associated melanosis, no subconjunctival worm observed |
| Cornea | Mild endothelial pigment | Mild endothelial pigment |
| Anterior Chamber | Deep and quiet, rare pigment | Deep and quiet, rare pigment |
| Iris | Normal architecture | Normal architecture |
| Lens | 2+ nuclear sclerosis | 2+ nuclear sclerosis |
| Vitreous | Normal | Normal |
| OD | OS | |
|---|---|---|
| Disc | Pallor most marked temporally with temporal cupping | Pallor most marked temporally with temporal cupping |
| C:D Ratio | 0.7 | 0.7 |
| Macula | Normal | Normal |
| Vessels | Normal | Normal |
| Periphery | Normal | Normal |
Video 1. Patient-captured video of a worm moving in the subconjunctival space of her left eye.
Differential Diagnosis
CLINICAL COURSE
Given her subjective history of eye pain and visualization of a worm moving within the subconjunctival space on video, the patient was referred to the UIHC infectious disease (ID) service. Visualization of a worm moving in the subconjunctival space is pathognomonic for loiasis. Therefore, filarial, Onchocerca, and Strongyloides serologies were obtained. Additionally, the patient was referred to the UIHC dermatology service for skin biopsies to test for co-infection with Onchocerca. The patient tested positive for IgG4 anti-L1-SXP-1, which is indicative of loiasis. Eosinophil count was 200/mm3 (normal = 40-390/mm3). All other tests returned negative or within normal limits, indicating her candidacy for treatment with diethylcarbamazine (DEC). DEC was obtained through the Centers for Disease Control and Prevention (CDC), and the patient completed a 21-day course (300 mg three times per day) with no adverse side effects. She continues to follow with neuro-ophthalmology for optic neuropathy of unclear etiology, which is the likely cause of her progressive bilateral vision loss.
DIAGNOSIS: Loiasis
DISCUSSION
Overview
Loiasis, also known as African eye worm, is a symptomatic infection with the filarial nematode Loa loa [1-4]. The disease is endemic, and essentially restricted to equatorial rain forest and savannah regions of Central and West Africa [3-5]. The disease is often asymptomatic but can present with migration of adult worms beneath the bulbar conjunctiva and non-pitting, episodic edema with pruritis, known as Calabar swelling [1-4].
Etiology/Epidemiology
Loiasis is endemic to Central and West Africa. It is estimated that 14.4 million people live in high-risk areas (≥40% estimated prevalence) and 15.2 million people live in intermediate risk areas (between 20-40% estimated prevalence), with the DRC and Cameroon accounting for approximately 40-80% of this at-risk population [2,5,6]. The prevalence tends to be higher in males than females (likely due to occupational exposure), increases with age (cumulative exposure), and is higher in individuals of low socioeconomic status [3,6].
In a 2011 study, 11 countries known or suspected to be endemic for loiasis were surveyed using the Rapid Assessment Procedure for Loiasis (RAPLOA) to generate a loiasis prevalence map (Figure 2). The RAPLOA is a questionnaire used to estimate individuals’ history of “eye worm”, or local names for L. loa, to predict whether loiasis is endemic in an area [5]. The study identified two hyper-endemic regions. The western hyper-endemic region includes the entirety of Equatorial Guinea and Gabon and areas of Cameroon, the DRC, the Central African Republic, and Chad (south of 6° N latitude). The eastern hyper-endemic region is the northeastern area of the DRC [5].
Parasitology
Vector Characteristics
L. loa is transmitted by tabanid flies from the genus Chrysops. In humans, L. loa is primarily transmitted by C. dimidiata and C. silacea [3,6]. These flies typically live near forested or muddy areas across Central and West Africa corresponding with the area of loiasis endemicity [3,6]. The Chrysops fly population, and consequently the rate of L. loa infection, peaks during the early months of the rainy season [3,6]. Interestingly, both C. dimidiata and C. silacea are attracted to the smoke of wood fires [3,6]. Both species express strong diurnal biting preferences, which is uncommon among other Chrysops species [6]. Up to 18% of Chrysops flies may be infected with L. loa in endemic regions [3].
Parasite Characteristics
The lifecycle of L. loa is demonstrated in Figure 3. L. loa microfilariae circulate through the peripheral blood, pass through the lymphatic system, and accumulate in the vascular beds of hosts’ lungs [3,4,6]. Microfilariae demonstrate diurnal periodicity that coincides with vector biting patterns [3,6]. Following ingestion by the vector, microfilariae mature through several larval stages in the midgut and thoracic musculature of the fly. Maturation into the infective L3 larval stage takes 7-12 days [4,6]. Afterward, L3 larvae migrate back to the head of the fly where they are inoculated into the host during the fly’s next blood meal [3,4]. Upon inoculation, L3 larvae traverse the subcutaneous tissue and lymphatic system of the host where they develop to sexual maturity [3,4]. Adult worms are found between the connective tissue layers of the skin and between the fascia of somatic muscles [4]. Fertilized adult female worms can produce 10,000-39,000 microfilariae per day, though they do not reach detectible levels until five to six months after the initial inoculation [4,6]. Only between 5-20% of microfilariae are present in the peripheral blood to be ingested by Chrysops vector flies at any given point [6]. The average life expectancy of adult L. loa is estimated to be at least nine years [6]. The average life expectancy of microfilariae is thought to be between three to five months; however, some studies suggest up to 12 months [6].
Signs/Symptoms
The first clinical signs of L. loa infection may appear as early as 2 months after initial infection, although the latent period can extend up to 20 years [3,4,6,7]. Most cases of loiasis are asymptomatic or mild [3]. Pathognomonic manifestations of the disease include migration of adult worms beneath the bulbar conjunctiva and Calabar swelling [2-4].
The primary ocular manifestation of loiasis is migration of adult worms about the orbit, typically beneath the bulbar conjunctiva. Adult female worms are 40-70 mm long and 0.5 mm in diameter and adult male worms are 30-34 mm long and 0.35-0.43 mm in diameter [3]. Common symptoms associated with migration include foreign body sensation, mild to severe discomfort and pain, local inflammation, and pruritis [2-4]. Less commonly, adult worms can migrate across the palpebra, which can result in palpebral or periorbital edema [2,4]. Rarely, adult worms can invade the anterior chamber or vitreous [4, 8-10] Associated symptoms can include pain, photophobia, and vision loss [2,3]. Slit lamp examination may reveal fibrinous membranes, cell, flare, or keratic precipitates [2].
Calabar swelling is transient, non-pitting, non-erythematous subcutaneous edema that spontaneously regresses and recurs at irregular intervals [2-4]. It can occur anywhere on the body, but most commonly occurs on the limbs near joints, resulting in painful and restricted movement [2-4]. Calabar swelling is caused by migration of mature L. loa larvae away from the site of inoculation by vector flies [2,3].
Other systemic manifestations, though less common, include asthenia, headaches, motor deficits, encephalitis, psychiatric symptoms, pulmonary infiltrates, endocardial fibrosis, hematuria, proteinuria, and renal failure [4,11].
Laboratory findings include microfilaremia (present in 30% of cases), eosinophilia, and elevated levels of IgE [3,11].
Differences between permanent residents of endemic areas and expatriates have been identified. Notably, permanent residents tend to demonstrate fewer symptoms, lower levels of eosinophilia, and greater levels of microfilaremia. Additionally, infected permanent residents tend to be younger than infected expatriates, likely due to early, chronic exposure to the source of infection [12].
Diagnosis
Definitive diagnosis is made by direct visualization of adult worms as they migrate across the subconjunctiva. Surgical removal of an adult worm can allow for laboratory identification and confirmation of infection [2,3].
Diagnosis can also be made by detection of microfilariae in the peripheral blood [3,4]. A fresh blood sample may show live microfilariae moving on a wet smear. Microfilarial load is determined by counting microfilariae in a Giemsa-stained sample of a known volume of peripheral blood. In samples with low microfilarial burden, alternative methods of determining concentration may be required (examples include the Knott technique, centrifugation of hemolyzed blood with saponin or formalin, or filtration through a membrane filter) [4]. Of note, microfilarial load and the accuracy of concentration testing is greatest between the hours of 10:00 AM to 2:00 PM [3].
Measurement of L. loa-specific IgG4 (recombinant L1-SXP-1) using ELISA antibody assays has been used in the past to detect occult infection, although this technique has low sensitivity and specificity [2,11]. Measurement of the recombinant L1-SXP-1 using a luciferase immunoprecipitation system (LIPS) assay has 100% specificity in uninfected individuals [11]. Measurement of recombinant L1-SXP-1 using a recently developed lateral flow assay (LFA) is 94% sensitive and 100% specific; this assay is now available for point-of-care testing [11,12].
Previously, the best method for the diagnosis of L. loa infection was PCR of species-specific sequences encoding a 15-kDa protein (95% sensitivity and 100% specificity), although this technique produces negative results during the latent period [4].
Treatment/Management/Guidelines
Treatment of loiasis involves surgical removal of visible adult worms in the process of migrating across the subconjunctival space and antimicrobial therapy to kill the remaining microfilariae and adult worms [2,3].
Surgical extraction of migrating adult worms is a minor procedure that can be done in the clinic. The worm should be grasped externally using forceps to prevent migration. 2% lidocaine with epinephrine 1:100,000 is injected subconjunctivally to simultaneously provide local anesthesia and paralyze the worm. The worm is then accessed and removed via small peritomy. Post-operative care includes systemic pharmacologic treatment (described below), topical antibiotics, and topical steroids [2,3].
When microfilarial load is low (below 2500 mf/mL), diethylcarbamazine (DEC) is the first line pharmacological agent in the treatment of loiasis. It is effective against both adult worms and microfilariae [2,3]. When microfilarial load is high, the risk of adverse effects from DEC increases dramatically. This risk can be mitigated by sequentially treating with an alternative agent, such as albendazole, mebendazole, or ivermectin, until microfilariae load decreases, then treating with DEC. [2,3]
Of note, ivermectin is highly effective in the treatment of loiasis. However, its use is associated with severe neurological side effects when administered to individuals who are co-infected with loiasis and onchocerciasis or lymphatic filariasis. The reason for these adverse reactions is unclear [3,4].
EPIDEMIOLOGY OR ETIOLOGY
|
SIGNS
LABORATORY FINDINGS
|
SYMPTOMS
|
TREATMENT/MANAGEMENT
|
Najdawi W, Lewis CY, Dawoud SA, Thurtell MJ. Loa loa Filariasis (African Eye Worm). EyeRounds.org. January 4, 2024. Available from http://EyeRounds.org/cases/352-loa-loa-filariasis.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.