Chief Complaint: Central scotoma in the right eye.
History of Present Illness: This 56-year-old female presented presented for evaluation with reduced vision and an oval-shaped central scotoma in the central visual field of the right eye for two months.
Past Ocular History: History of cataract extraction in both eyes - Right eye 6 years ago and left eye 13 years ago.
Medical History: None
Medications: None
Family History: Noncontributory
Social History: Noncontributory
Ocular Exam:
 |
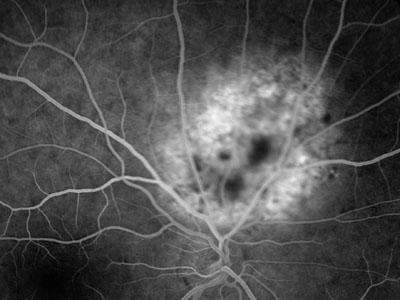
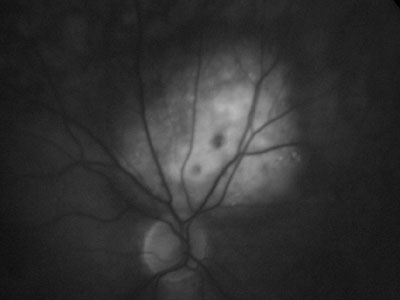
| 2A: Early phases of flourescein angiograph with hyperflourescence within the lesion in a coarse vascular pattern | 2B: Marked dye persistance within the lesion 20 minutes after injection |
 |
 |
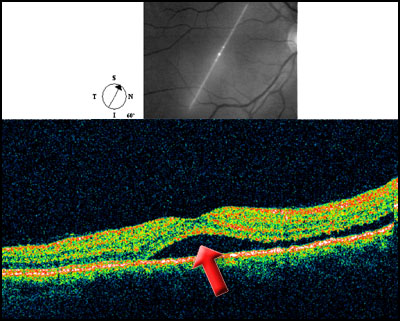
| 2C: Optical coherence tomography (OCT) section through the macula demonstrating sub-retinal fluid (red arrow) prior to treatment. Visual acuity 20/70. | |
 |
|
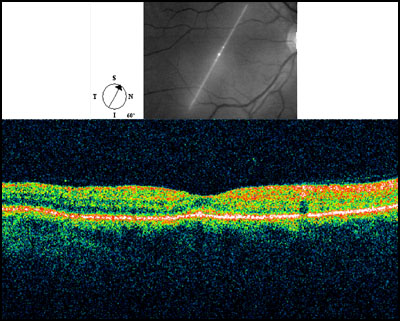
Course: The patient's examination, FFA and OCT were all consistent with choroidal hemangioma. The patient underwent photodynamic therapy employing the technique described in the literature (Michels, 2005). After infusion of 6mg/m2 of verteporfin (Visudyne) intravenously the lesion was illuminated for 163 seconds with the activating laser. Two months later vision had improved from 20/70 to 20/30 and the sub-retinal fluid had resorbed clinically and on OCT (Figure 3)
 |
Choroidal hemangioma are vascular hamartomas that are present in two distinct forms: a discrete or circumscribed form, and a diffuse form. The diffuse form is typically associated with Sturge-Weber syndrome and discrete lesions are more common in non-syndromic cases. Discrete lesions are typically located near and temporal to the optic disc and are solitary. On examination their most distinguishing feature is their color, usually orange-red or orange-yellow, although other variations have been noted. Symptoms associated with the lesion are usually absent until adulthood. The visual defects that are observed are due to retinal degeneration overlying the tumor as well as serous retinal detachments caused by the lesion.
Fluorescein angiography and ultrasonography are helpful in making the diagnosis of a discrete choroidal hemangioma. On angiography, the lesion will quickly develop diffuse hyperfluorescence and in the arteriovenous phases the initially mottled pattern of fluorescence becomes more confluent. A "coarse vascular pattern" of spotty hyperfluorescence is often described. In later stages, compartmentalized accumulation of dye occurs in the outer retina. Hypofluorescence is also sometimes observed outlining the lesion, correlating to melanocytes that have been pushed to the margin of the tumor. Hemangioma also have a characterstic ultrasonography presentation. The lesions are usually dome shaped with a high internal reflectivity of regular structure. Also, spontaneous vascular movements are not present. In cases where choroidal hemangiomas are associated with increased pigmentation, the highly refective echographic signature of the lesion is helpful in distinguishing from choroidal melanomas, which have a characteristic low to medium reflectivity.
Photocoagulation has long been the accepted method for treating discrete choroidal hemangiomas that are associated with serous retinal detachment. Extent of treatment is limited to the amount needed to resolve the serous fluid. Recently, photodynamic therapy has shown promise in its efficacy and safety in treating symptomatic hemangiomas (Michels, 2005 and Vincuna-Kojchen 2006) and was the method chosen in this case. Additional long-term studies are underway, but intial results are promising. Other therapies have been tried, including low-dose external beam irradiation, proton therapy, and plaque radiotherapy for certain cases of choroidal hemangioma with mixed results.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENTObservation may be all that is indicated in non-vision threatening lesions Treatment is usually indicated with serous retinal detachments and vision loss:
If diffuse hemangioma, work-up for Sturge-Weber Syndrome should be initiated. Glaucoma may need to be addressed |
Zablocki G, Hagedorn C, Brady KD. Choroidal Hemangioma: Central scotoma in the right eye. EyeRounds.org. January 23, 2007; Available from: http://webeye.ophth.uiowa.edu/eyeforum/cases/65-Choroidal-Hemangioma-Photodynamic-Therapy.htm, 2007

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.