Chief Complaint: Blurred vision in the left eye (OS)
History of Present Illness: A 19-year-old female initially presented to her local physician complaining of headaches, especially while reading. She was referred to her local optometrist who maximized her vision with an updated refraction. Shortly thereafter, however, the patient experienced continued blurred vision in the left eye only. Believing her lens correction to be too strong, she returned for another examination. A dilated fundus examination revealed that the optic discs had a "lumpy-bumpy" appearance, suspicious for optic disc drusen and she was referred to the University of Iowa Hospitals and Clinics for further evaluation. Other than mildly blurred vision, the patient denied any other ocular symptoms.
Past Ocular History: No past ocular surgery or trauma.
Medical History: History of seasonal allergies and sinus infections.
Medications: None
Family History: Known history of cataracts, arthritis, and cancer in the family.
Social History: The patient is an active, young female who works as a frame stylist for a local optical shop. She does smoke and drinks alcohol socially.
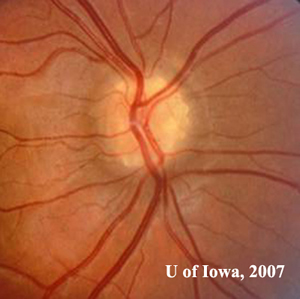
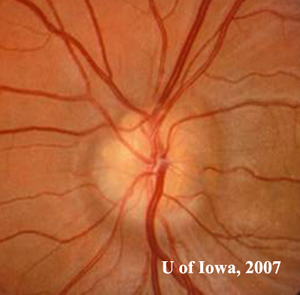
| 1A: Numerous round, yellowish elevations visible in the optic nerve head, OD | 1B: Similar "lumpy-bumpy" or "rock candy" yellow elevations within the optic nerve head, OS |
 |
 |
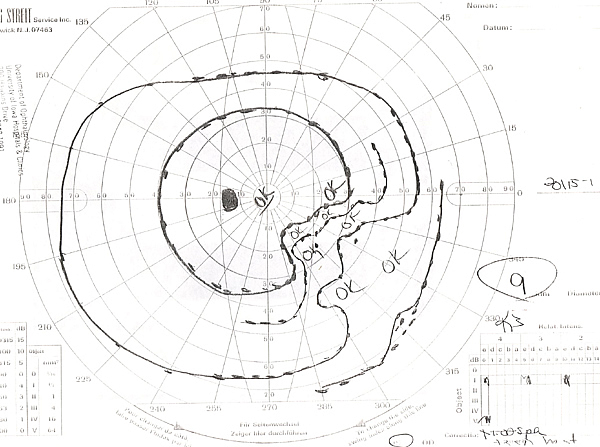
| 2A: Goldmann Visual Field, OS - There is a dense nasal step defect | 2B: Goldmann Visual Field, OD - Several scotomas are evident, including the appearance of a partial arcuate-style defect inferiorly |
 |
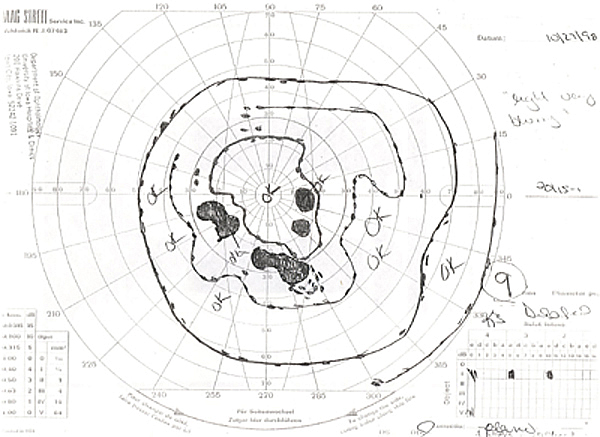 |
Course: Examination of the patient's optic nerves led to a high suspicion of multiple optic disc drusen. Futher testing including standardized echography which confirmed the presence of numerous highly reflective drusen within both optic nerve heads, OD > OS. Goldmann perimetry revealed enlargement of the blind spots and other small peripapillary scotomas. The patient’s vision was refracted to make sure her vision was correctly appropriately and she was instructed to return in 6 months.
Discussion:Optic Nerve Head Drusen (ONHD) are often incidental findings discovered during routine eye examinations. Drusen are depositions of mucopolysaccharides and proteinaceous material that accumulate anterior to the lamina cribosa within the optic nerve head. Some believe that these depositions occur as a result of axonal degeneration of the optic nerve (Wilkins 2004, Giovannini 2005) or axoplasmic transport stasis secondary to congenitally crowded optic nerve heads (Spencer 1978). ONHD are found in approximately 1% of the general population, with bilateral distribution in 75-85% (Auw-Haedrich 2002, Sowka 2001). They are more common among Caucasians and are believed to have an autosomal dominant pattern of inheritance with incomplete penetrance (Davis 2003). However, this remains unproven. Both Lorentzen (1961) and Antcliff and Spalton (1999) were unable to verify this pattern of inheritance. An inherited optic nerve head dysplasia might be the primary risk factor for developing ONHD (Lee 2005). According to Lorentzen the condition is transmitted as an "irregularly dominant fashion" (Lorentzen 1961). The primary pathology arises from an inherited dysplasia of the optic disc and its blood supply which predispose to formation of optic disc drusen (Auw-Haedrich 2002).
There are two main types of ONHD: visible drusen (as in this case) and "buried" drusen. Buried drusen are often found in younger age children (pre-teenage years) and can obscure the edges of the optic disc and cup. The optic disc can appear to have no "optic cup", resulting in the appearance of papilledema, which is a major part of the differential diagnosis (Davis 2003). As patients get older, particularly past the teenage years, the drusen become more visible. The drusen begin to protrude from the edge of the optic disc and cup, especially on the inferior nasal side (Wilkins 2004).
Patients with ONHD are often asymptomatic, thus the high rate of incidental discovery. The earliest symptoms of ONHD are abnormalities in peripheral vision or transient visual obscurations, such as flickering or "graying out" (Giovannini 2005, Davis 2003). Patients do not complain of central vision loss because central visual acuity is generally spared with optic disc drusen. Central acuity may be affected if subretinal choroidal neovascularization is present.
Visual inspection alone is often insufficient to confirm ONHD and rule out more concerning possible diagnoses. For example, it is mandatory that the physician distinguish pseudopapilledema from true papilledema. In some cases this will require appropriate radiologic neuroimaging to rule out intracranial mass or lesion. Glaucoma as a cause of the peripheral field loss must also be evaluated. Though intraocular pressures (IOP) are elevated in most types of glaucoma, this is not always the case and the distinction between glaucomatous damage and benign ONHD is not always so straitforward. Visual field examinations with either static or dynamic perimetry should be conducted to evaluate peripheral field loss. Field defects can be present due to ONHD alone. A study to Auw-Haedrich in 2002 revealed that Goldmann Visual Fields (GVF) may show areas of nerve fiber defects (most commonly inferior nasal area), enlargement of the blind spot with or without constriction of the peripheral fields. Additionally, many suggest that the presence of ONHD makes the nerve more susceptible to glaucomatous damage at lower pressures. As such, one must carefully follow visual fields in suspicious cases and treat elevated IOP appropriately if there is progression of field loss.
As optic nerve drusen enlarge, they can compress and compromise nerve fibers and the vascular supply, leading to multiple complications including visual field defects, vascular occlusion, and hemorrhage (Sowka 2001). Vascular compromise to the optic nerve head may result in Anterior Ischemic Optic Neuropathy (AION)]. In patients with drusen, typical risk factors for AION are not necessarily present, with many of the patients affected being in their mid-20s or younger with no signs of any cardiovascular disease (Davis 2003).
Drusen have also been implicated in multiple types of vascular occlusive complications. Central retinal artery occlusion (CRAO) has been reported when drusen are present in conjunction in patients with systemic hypertension, migraine headaches, oral contraceptive use, high altitude, or atrial septal defect (Auw-Haedrich 2002). Approximately 10% of the venous retino-choroidal collateral supply is connected to ONHD, with central retinal venous occlusion as the major source. These vessels are the result of increased venous pressure from compression of the veins by drusen. As the patient ages, the vessels become more prominent due to enlarging drusen (Auw-Haedrich 2002).
Optic nerve drusen can also result in juxtapapillary choroidal neovascularization with subsequent hemorrhage. Choroidal neovascularization in younger patients is associated with a much better prognosis than in adults. In younger patients, resolution will occur with mild to moderate visual symptoms. In seven reported cases, six of the patients regained 20/40 vision or better without treatment (Harris 1981).
Optic neve drusen are associated with several ocular and systemic diseases. In retinitis pigmentosa the incidence of disc drusen is reportedly between 0 and 10%, but the drusen are often not visible, scleral canals are normal, and no disc elevation is present. Drusen is also associated with rare disorders such as pseudoxanthoma elasticum (with a prevalence of about 1:160,000) and angioid streaks (with a prevalence of 1:80,000). Although these two conditions are fairly rare, 85% of people with pseudoxanthoma elasticum also have angioid streaks, making drusen a common connection between the two conditions (Davis 2003).
No definitive treatment currently exists for optic nerve drusen. Patients with documented optic nerve drusen should be followed with serial visual field exams, optic nerve fiber analysis, and repeat intraocular pressure checks. If visual field loss occurs in the presence of drusen, medication to lower intraocular pressure should be considered. It may be difficult to distinguish optic nerve drusen from progressing glaucoma as the cause based solely on visual field testing (Davis 2003, Auw-Haedrich 2002).
Most cases of subretinal neovascularization associated with optic disc drusen resolve without treatment and with only mild symptoms. Laser photocoagulation should only be considered in cases if central visual acuity is threatened. (Davis 2003, Auw-Haedrich 2002).
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Patel V, Oetting TA. Optic Nerve Drusen: 19-year-old female with blurred vision. EyeRounds.org. August 14, 2007; Available from: http://www.EyeRounds.org/cases/72-Optic-Nerve-Drusen-Visual-Field-Loss.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.