Chief Complaint: 44-year-old male with diplopia
History of Present Illness: This 44-year-old male with a history of hypertension awoke with the worst headache of his life. He was admitted to the University of Iowa Hospitals and Clinics for decreasing level of consciousness. When his condition was stabilized, neuro-ophthalmology was consulted to evaluate a bilateral abduction deficit.
Ocular History: Patient was unable to provide
Medical History: Hypertension, Hepatitis C, reflux
Medications: atenolol, ranitidine.
Family and Social History: History of drug and alcohol abuse
 |
||
 |
 |
 |
 |
If video fails to load, use this link: https://vimeo.com/134675900
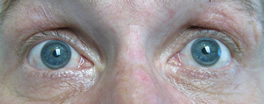
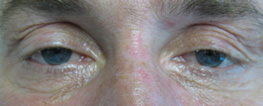
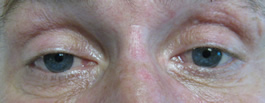
Motility video – note vertical gaze palsy in up and down gaze in addition to abduction deficit in left and right gaze.
Where is the patient's lesion based on the following clinical findings?
Neuroanatomical Review: The combination of esotropia (bilateral abduction deficits), vertical gaze palsy, alternating levels of consciousness and Cheyne Stokes breathing pattern led us to localize the lesion to the mesodiencephalic junction.
The rostral interstitial nucleus of the medial longitudinal fasciculus (riMLF) is an important center for vertical saccades. This nucleus is located at the mesodiencephalic junction (junction of thalamus and midbrain). This area of the rostral midbrain is supplied by the posterior-thalamo-subthalamic branch of the basilar communicating artery which is a branch off the basilar tip (1). This artery, being at the end of the basilar artery, is a known location for emboli.
Abducens palsy vs. other types of abduction deficits
When evaluating patients with abduction deficits one must think about the pathway involved. Lesions anywhere along the pathway from the extra ocular muscles to the supranuclear areas that control horizontal saccades may be implicated in the etiology for the motility deficit.
Bilateral abduction deficits in the setting of trauma or subarachnoid hemorrhage often indicate increased intracranial pressure causing a bilateral cranial nerve VI palsy. This sudden rise in intracranial pressure can lead to downward displacement of the brainstem which can compress cranial nerve VI in the pre-pontine cistern as it makes a 90° bend and exits the pontomedullary junction to ascend along the clivus towards the cavernous sinus. Other causes for acquired bilateral abduction deficits in the setting of trauma, subarachnoid hemorrhage, or stroke, include damage to the convergence pathway, thalamic esodeviation, or breakdown of a pre-existing phoria due to loss of conscious control.
Caplan, in 1980 defined the phrase, pseudoabducens palsy as "a failure of ocular abduction which is not due to dysfunction of the sixth nerve", and postulated that increased convergence activity was the cause (2). The neurologic pathways for convergence are not discrete nerve tracts. Instead, a network of fibers descend from the temporal-parietal-occipital junction where the pathway is thought to originate, through the medial thalamus, to the level of the rostral midbrain where they synapse with the medial rectus subnuclei of the cranial nerve III nucleus. Damage to these fibers is thought to lead to decreased inhibition and therefore increased neuronal activity, causing increased convergence and an esodeviation (3). Previous reports in the literature have identified thalamic infarcts to have a characteristic inward and downward deviation of the eyes where the eyes appear to be "peering at the tip of the nose (4,5,6). This finding may be caused by damage to these descending convergence fibers at the level of the thalamus. Please see the following video as a demonstration of thalamic esotropia in the setting of bilateral internuclear ophthalmoplegia (INO).
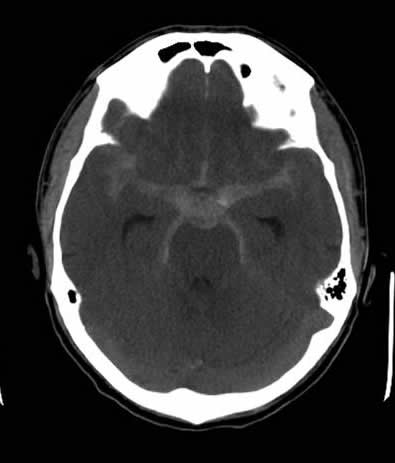
For evaluation of the worst headache of his life, a CT of the brain without contrast was obtained which revealed a subarachnoid hemorrhage (See Figure 2A). CT angiography revealed a basilar artery aneurysm which was successfully coiled (See Figure 2B).
13 days after the hospital admission and coiling of the aneurysm, neuro-ophthalmology was consulted for evaluation of bilateral abduction deficits.
 |
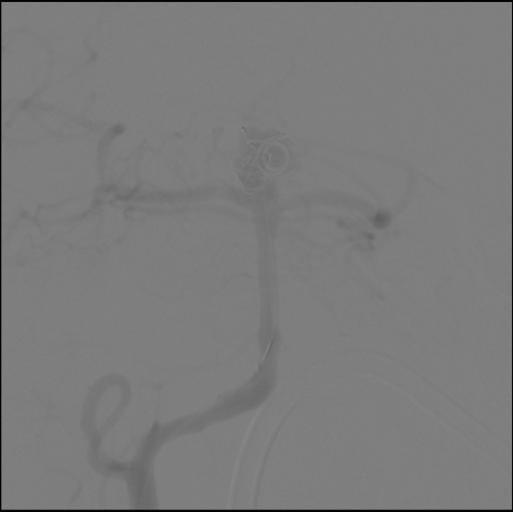 |
| Figure 2A. CT scan of the brain showing diffuse subarachnoid hemorrhage | Figure 2B. CTA showing basilar artery aneurysm with coil in place |
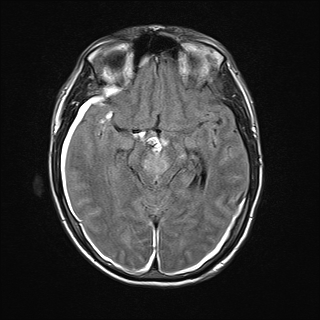
The findings in our patient of vertical gaze palsy in both up and down gaze, bilateral abduction deficits (likely pseudoabducens palsy) localized to a lesion in the mesodiencephalic junction in the territory supplied by the posterior thalamo-subthalamic paramedian artery, a branch off the tip of the basilar artery. MRI confirmed a subacute infarction in this region (See Figure 3A, 3B, 3C, 3D). The infarction may have been caused by compression or disruption by coiling of the posterior thalamo-subthalamic branch of the paramedian artery.
 |
 |
| Figure 3A. MRI with DWI (diffusion weighted imaging) showing hyperintense signal in rostral midbrain. | Figure 3B. MRI with ADC (apparent diffusion coefficient) showing corresponding area of hypointensity. This signifies infarction. |
 |
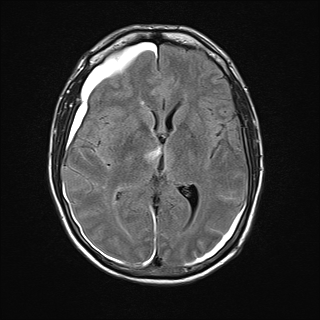 |
| Figure 3C. MRI Flair image showing hyperintensity in the Rostral midbrain | Figure 3D. MRI Flair image showing hyperintensity in the right thalamus. Also note hyperintense signal from subarachnoid hemorrhage |
Diagnosis: Infarction of the rostral midbrain and thalamus causing pseudoabducens palsy and vertical gaze palsy.
Birkholz ES, Wall M: Pseudoabducens palsy: When a VI nerve palsy is not a VI nerve palsy. Eyerounds.org. Posted December 22, 2009; Available from: http://www.EyeRounds.org/cases/93-PseudoAbducensPalsy.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.