Chief Complaint: Patient on Amiodarone therapy. No visual complaints.
History of Present Illness: 54-year-old white male with a known history of atrial fibrillation and hypertension. The patient had been on Amiodarone therapy for several years. Two months prior to this routine follow up, the patient's primary care doctor made a change in the patient's cardiac medications which included the removal of amiodarone from his medication regimen. The patient has no vision complaints.
PMH/POH: Atrial fibrillation and hypertension. No other ocular or health problems.
 |
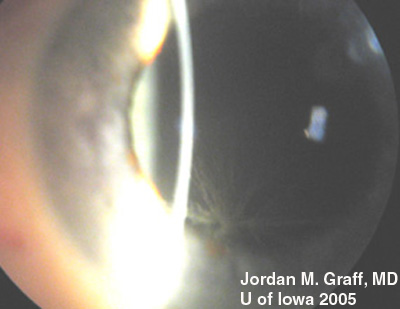 |
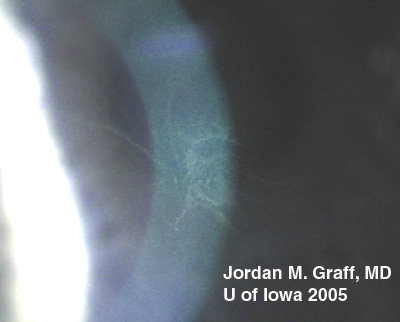
There are dozens of medications, materials, and disease biproducts that can result in deposits in the cornea. These deposits occur in various levels of the cornea. Corneal verticillata, also called vortex keratopathy, are one type of corneal deposits. Verticillata are readily recognizable by their distinct appearance as fine, golden-brown or gray opacities that are almost always bilateral. The opacities branch out from a central whorl, usually across the inferior cornea. The most common causes of verticillata include:
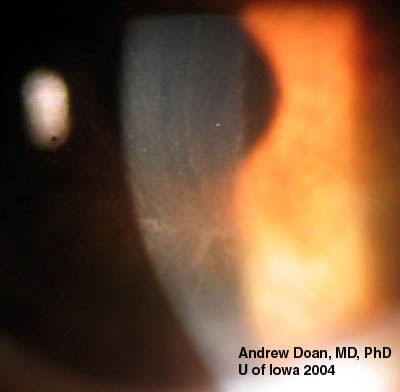 |
In the case of our patient, he had developed classic corneal verticillata from amiodarone use. As can be seen, the verticillata are somewhat less distinct than some published examples. Having been off the medication for 2 months, it is expected that the deposition pattern will diminish, as is the case for the vast majority of patients. Verticillata almost never cause vision complaints. Rarely, patients may notice haloes. The deposits occur within the subepithelium, do not stain, and are non-irritating. It has been hypothesized that the amphiphilic drugs that deposit verticillata may form complexes with phospholipids in the cells. These complexes cannot be metabolized by lysosomal phospholipases. Tissues where phospholipids content or turnover is high, lamellar or crystalloid deposits may occur. Verticillata from indomethacin, amiodarone, chloroquines, and phenothiazines are similar in this respect.
Verticillata from Fabry disease are similar in appearance to those caused by medication related deposits. Fabry disease is a glycolipidosis caused by deficiency of the alpha-galactosidase A (alpha-Gal A) enzyme. In addition to the verticillata and corneal spoke-like deposits, patients often have severe pain in the extremities, and characteristic skin lesions (angiokeratomas). In the third or fourth decade of life, more severe effects of the disease are manifest including progressive cardiovascular, renal, and cerebrovascular disease (seizures and strokes). Some heterozygote female carriers of the alpha-Gal A defect may express varying degrees of the disease as carriers, including corneal verticillata.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Suggested citation format: Graff JM. Verticillata: 54-year-old white male with a known history of atrial fibrillation and hypertension on amiodarone. EyeRounds.org, February 21, 2005; Available from http://www.EyeRounds.org/cases/case29.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.