
September 18, 2017
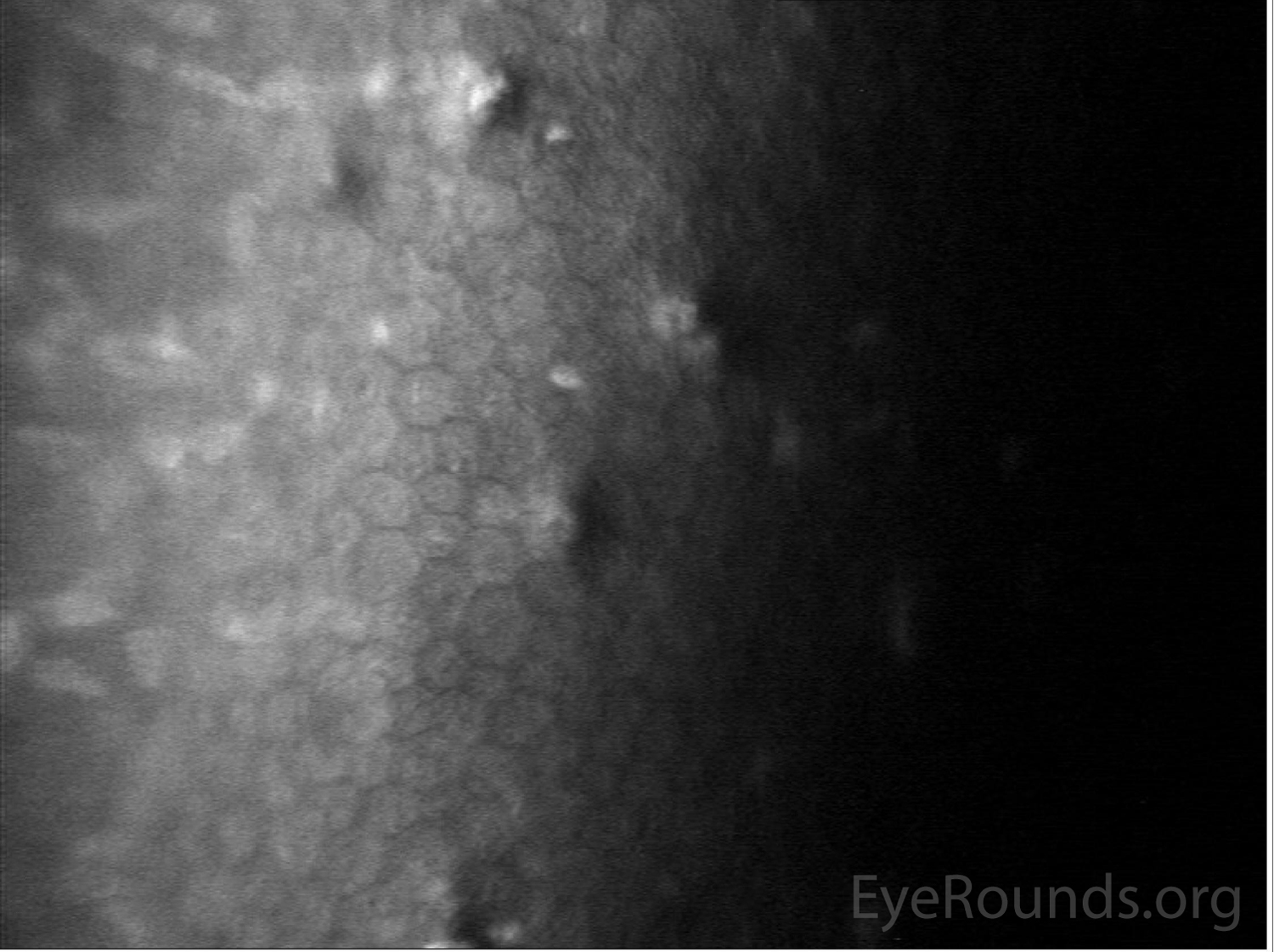
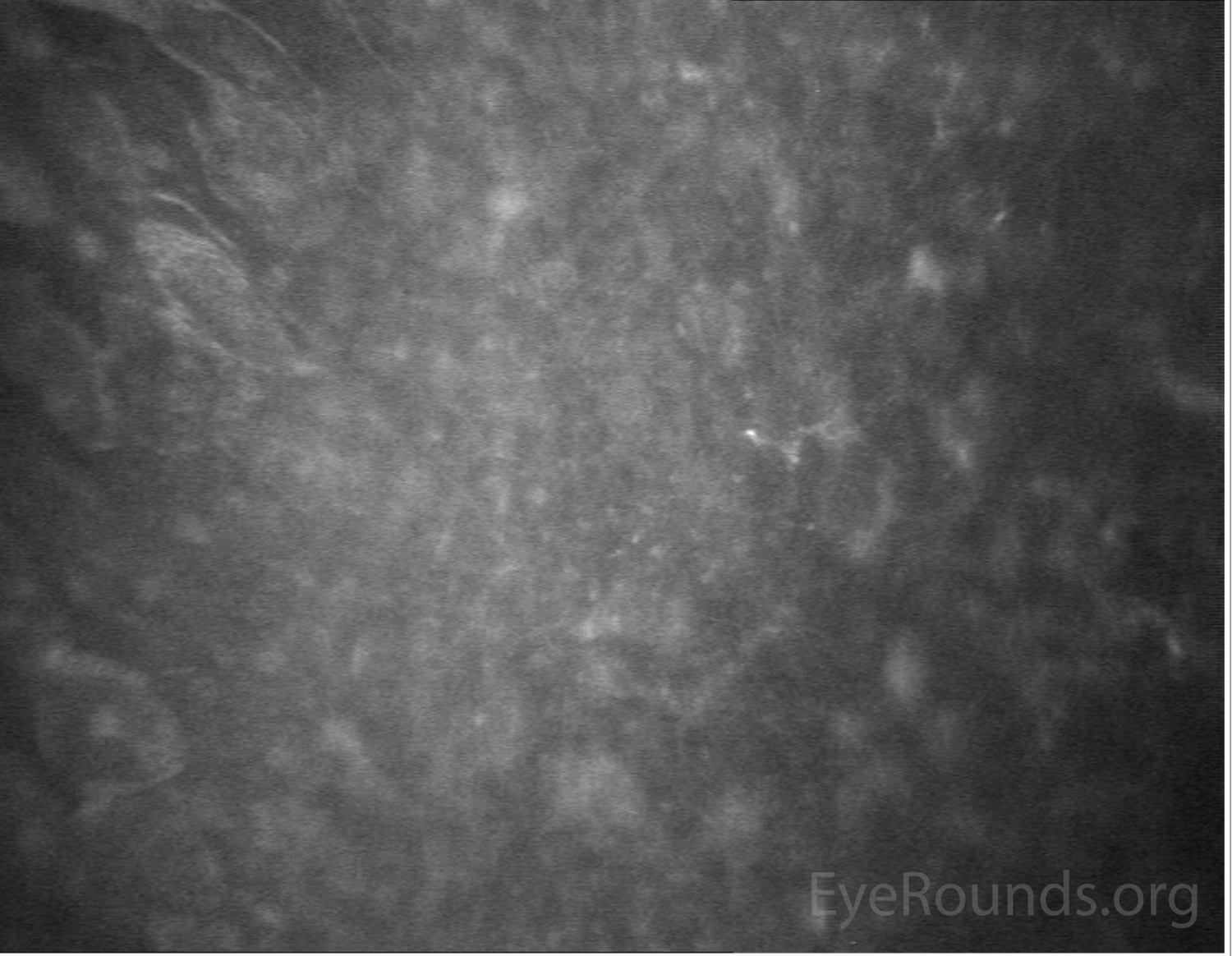
A 43-year-old woman with poor contact lens hygiene presented with two weeks of redness, pain, photophobia, and decreased vision of the right eye (OD). Visual acuity was 20/60 OD, and her anterior segment examination is documented in Figures 1-3. She was started on two fortified topical antibiotics, topical amphotericin, oral valacyclovir, and a topical cycloplegic, and corneal cultures were collected. Confocal microscopy showed numerous activated keratocytes without definitive hyphae or amoebic cysts (Fig 4). Corneal cultures were positive for >100 colonies of Nocardia farcinica. Topical amikacin 10 mg/mL and oral trimethoprim-sulfamethoxazole were added to her regimen. Within two weeks, her symptoms resolved and vision improved to 20/15 OD. Her drops were slowly tapered over three months.
Nocardia keratitis (NK) is a rare cause of bacterial keratitis that mimics fungal infections and, as a result, is often diagnostically challenging. Nocardia are gram-positive, aerobic bacteria of the actinomycetes order that are found in microflora of soil, dust, decaying vegetation, etc (1). NK classically leads to a wreath-like arrangement of patchy, anterior stromal infiltrates in the setting of trauma, contact lens use, or LASIK (1, 2). The course of NK is usually slowly progressive; however, these infections are commonly recalcitrant unless Nocardia-specific treatment (e.g., amikacin and sulphonamides) is initiated early (1, 2). Topical corticosteroids should be avoided prior to adequate treatment of Nocardia (1).
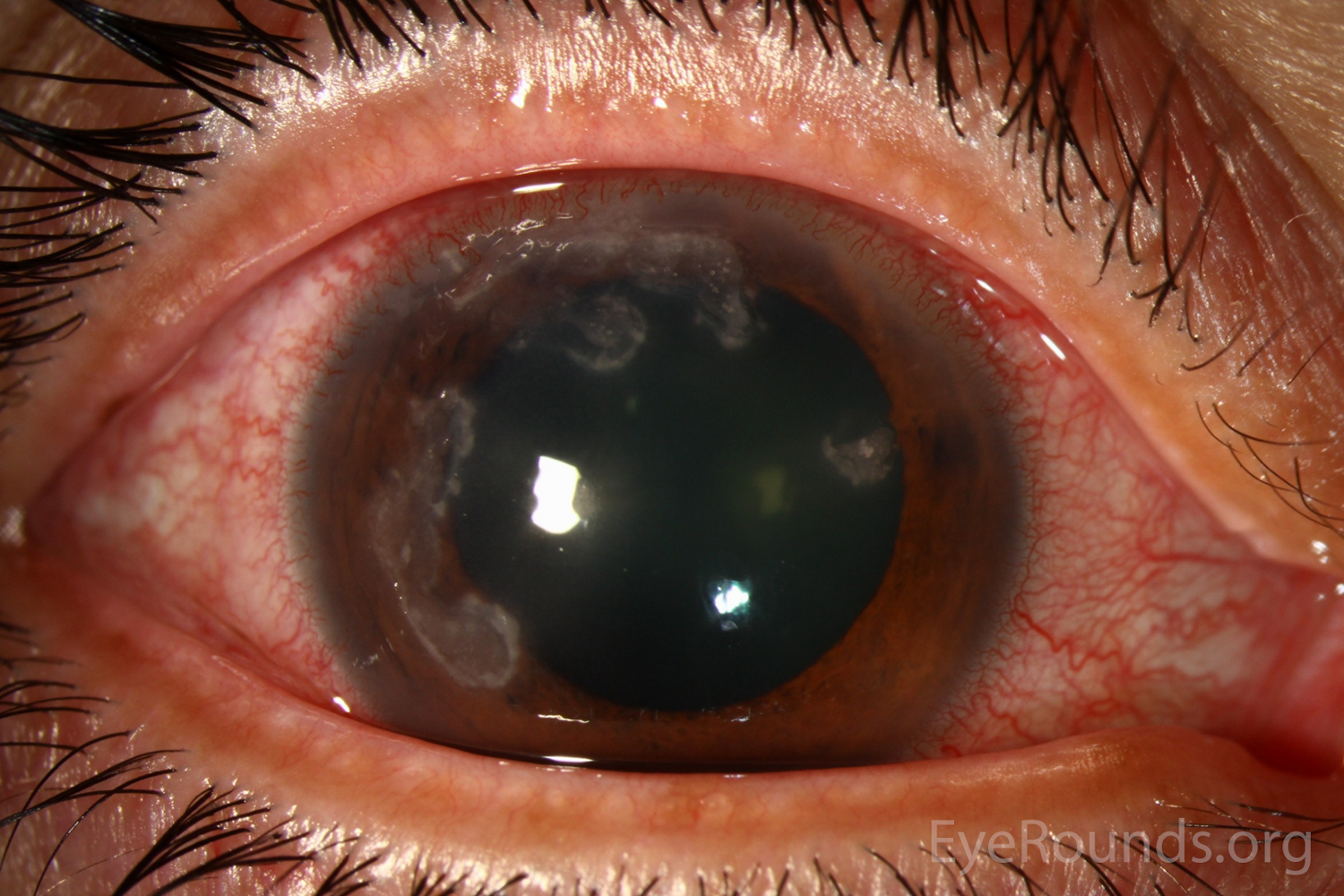
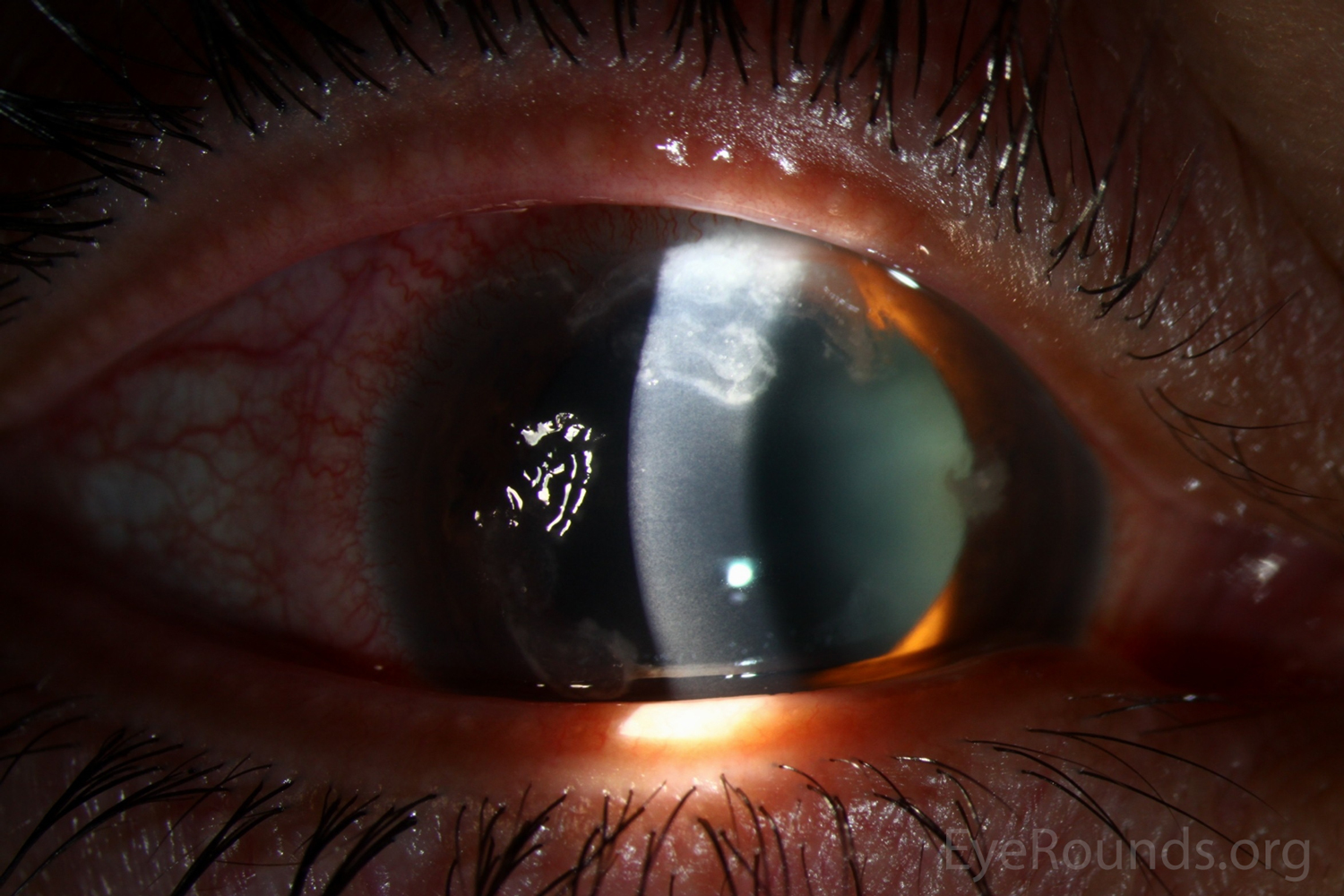

A 52-year-old male with a 35+ year history of hard and soft contact lens wear, poor lens hygiene, including overnight wear and recent hot tub exposure, presented with decreased vision in the left eye and eye pain. On presentation, his visual acuity was 20/20 OD and 20/60 OS, with intraocular pressures of 15 and 13 mmHg, respectively. Slit-lamp examination revealed multifocal, wreath-like infiltrates consistent with microbial keratitis. Corneal cultures grew >100 colonies of Nocardia species. The patient was started on polyhexamethylene biguanide, erythromycin, and amikacin 2.5% for treatment of Nocardia keratitis.