
This is a 46-year-old monocular man who presented with floaters, peripheral vision loss, and decreased central acuity in his left eye. Nine months prior to presentation, the right eye had suffered a penetrating globe injury with retinal detachment and was enucleated within four weeks of the injury.
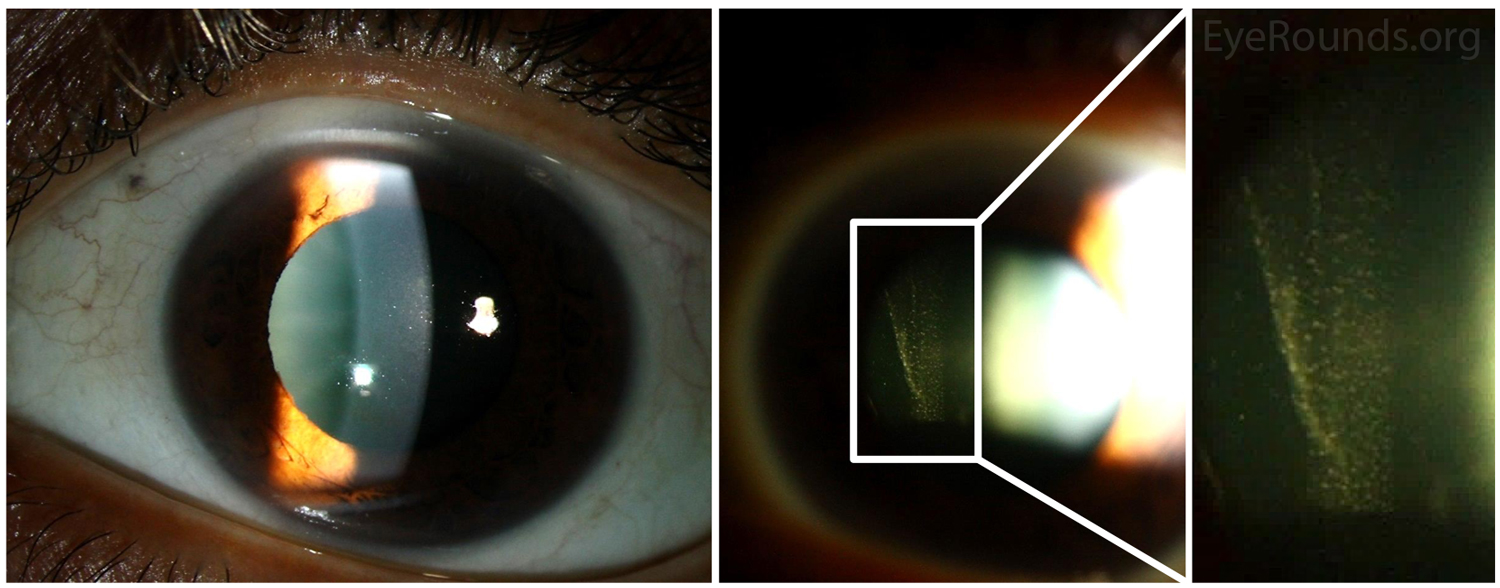
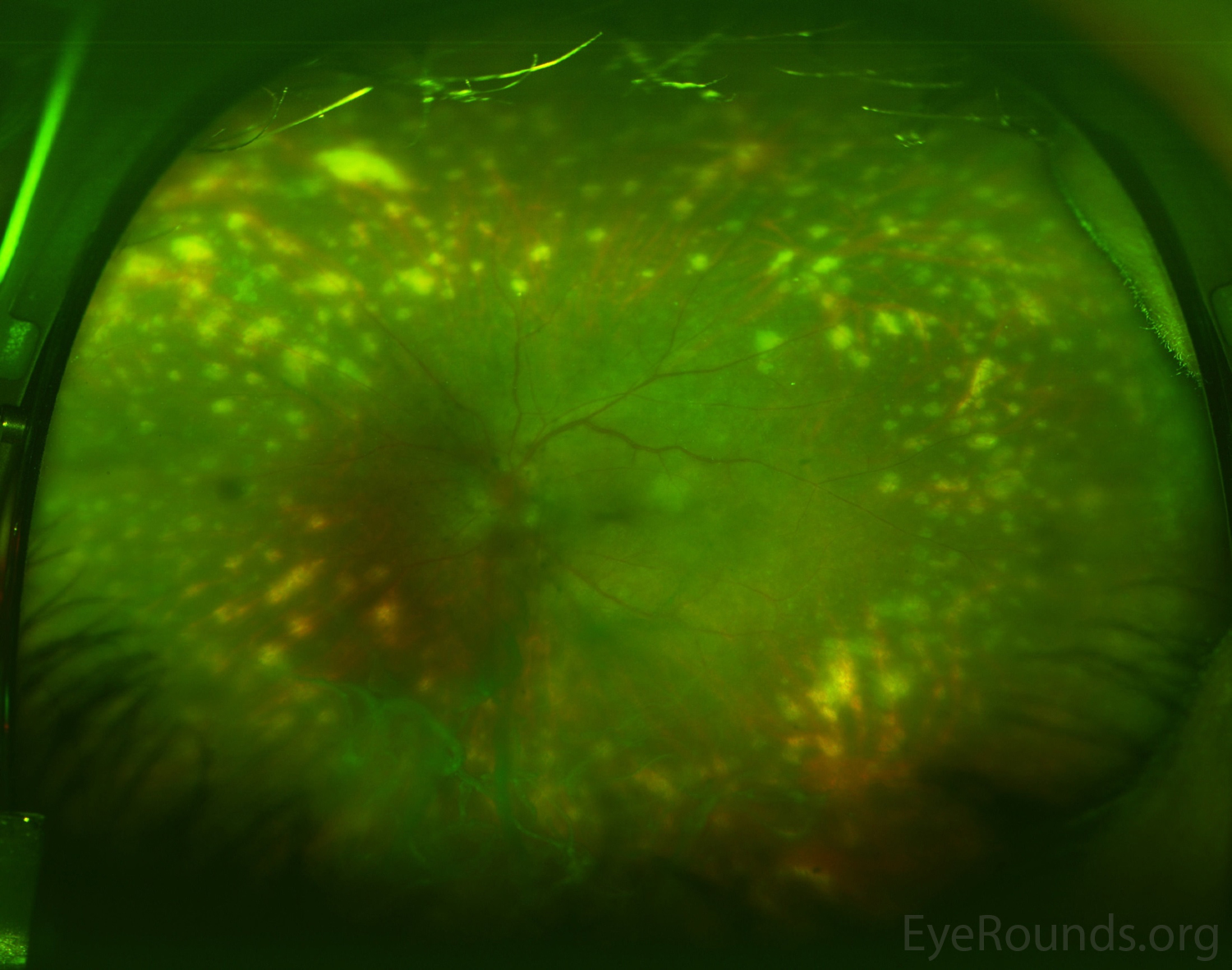
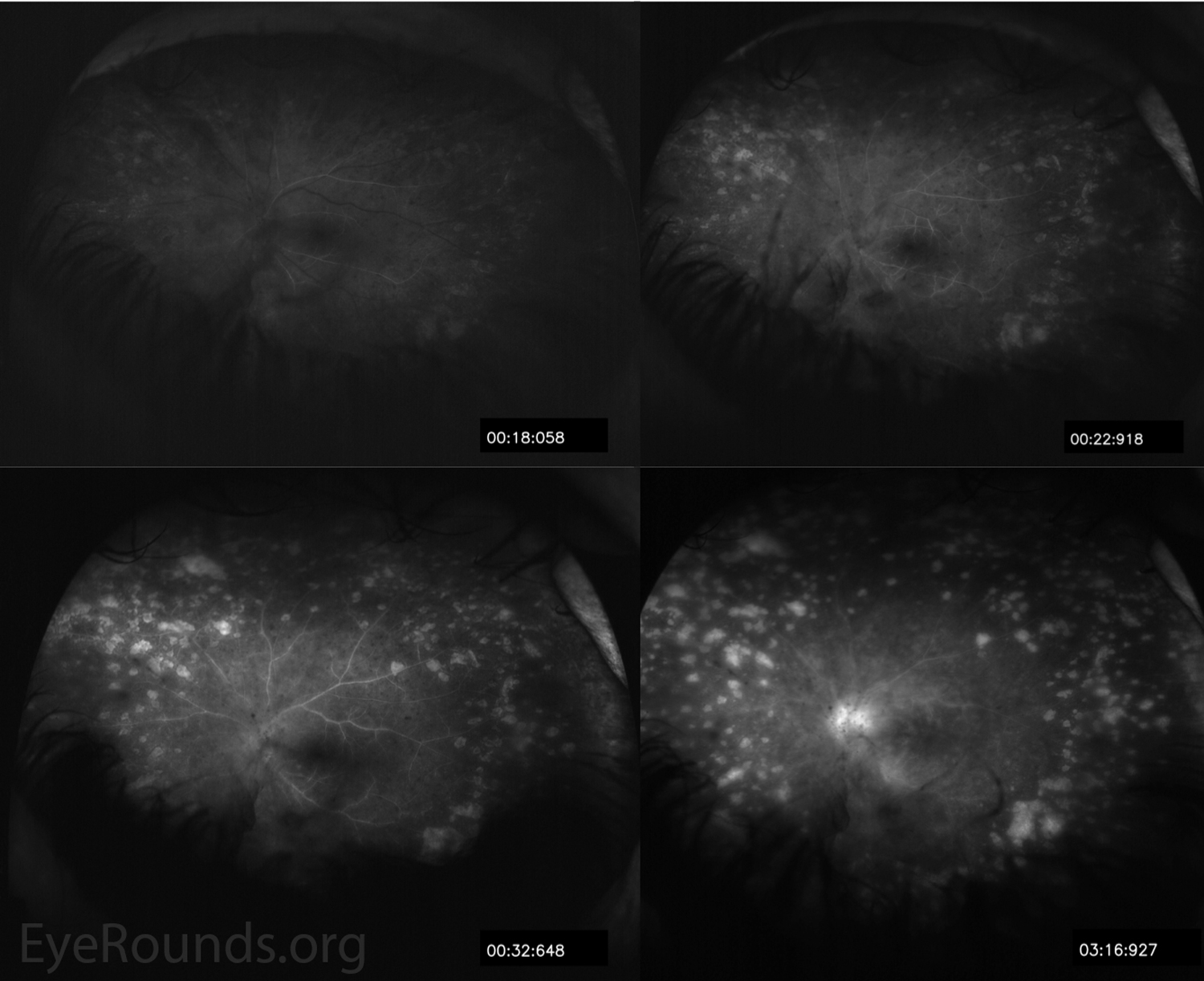
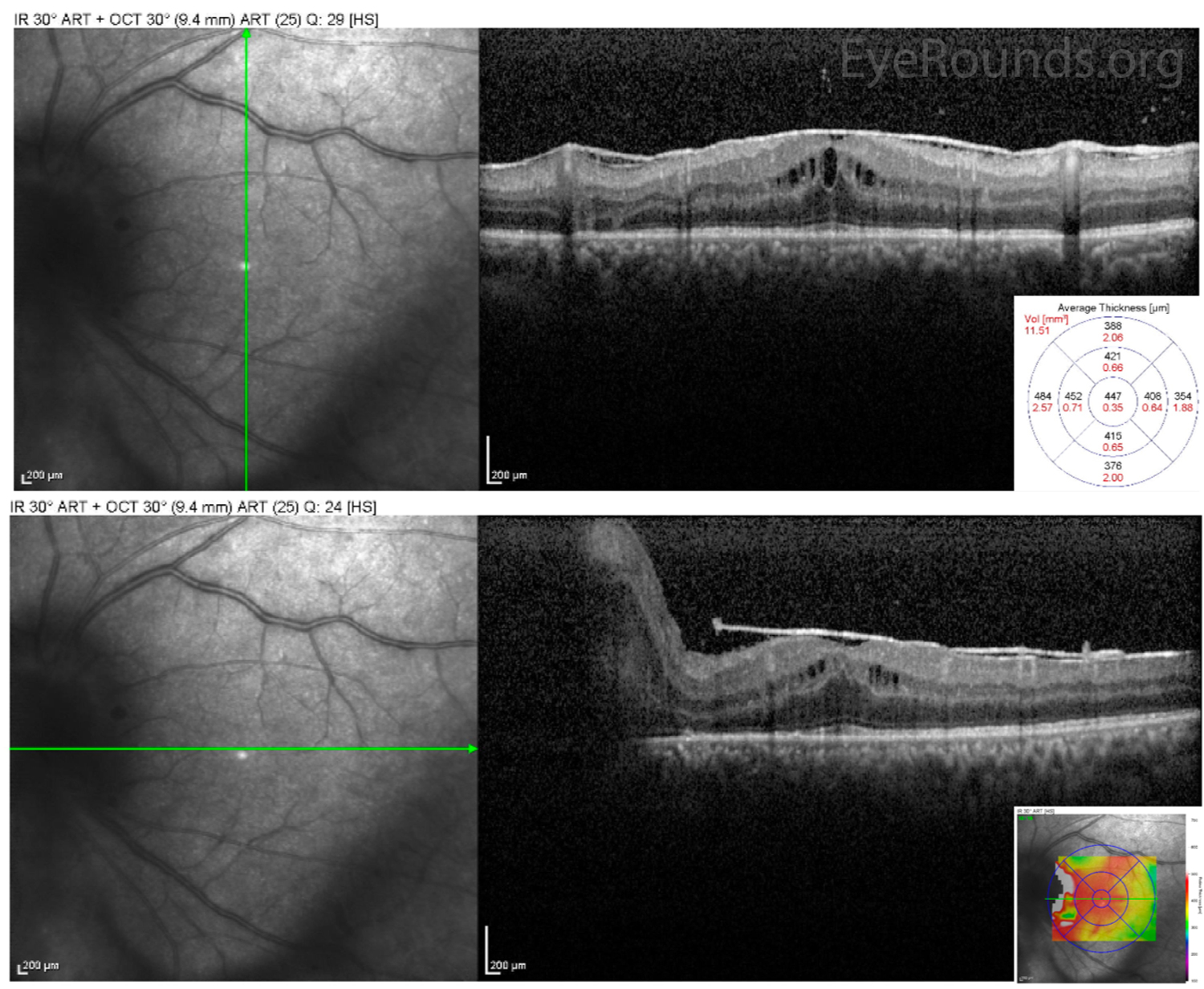
His slit lamp exam demonstrated anterior and posterior chamber cell (Figure 1). Dilated fundus exam revealed vitreous strands, grade III disc edema, and multiple, discrete, peripheral hypopigmented lesions consistent with Dalen-Fuchs nodules (i.e., lymphocytes and epithelioid histiocytes present between the RPE and Bruch membrane) (Figure 2). Fluorescein angiography demonstrated staining of the multiple peripheral lesions and leakage from the optic nerve and vessels in the posterior pole (Figure 3).
Despite initial treatment with mycophenolate mofetil (CellCept) for several months, the patient experienced worsening peripheral vision and persistent vitreous inflammation. He underwent surgical placement of a fluocinolone acetonide intravitreal implant (Retisert) for local, long-term inflammation control.
Sympathetic ophthalmia (SO) is a rare, granulomatous panuveitis that usually occurs within one year of penetrating trauma to the fellow eye, likely as a result of uveoretinal antigens entering the conjunctival lymphatics [1, 2]. In addition to trauma, pars plana vitrectomy and other intraocular procedures are associated with increased SO risk [2]. Other characteristic findings of SO that were not present in this case include serous retinal detachments and mutton-fat keratic precipitates.
Please refer to the Eye Rounds case on sympathetic ophthalmia for further information regarding work-up, differential diagnosis, pathophysiology, and management.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.