Chief Complaint: Spot on the iris of the right eye.
History of Present Illness: A 57-year-old female noted a new tan-colored spot on the lower portion of her right iris while looking in the mirror. Her optometrist was concerned about this lesion, as it was easily visible and had not been noted on examinations over the prior three years. The patient denied any change in vision or other ocular symptoms.
Past Ocular History: Myopia and presbyopia
Medical History: Hypertension and depression
Ocular Exam:
.jpg) |
.jpg) |
|
alternative video link: http://www.youtube.com/watch?v=AcYQZ-vW-jc |
Based on the clinical appearance, it was thought that the patient's iris lesion was a melanoma.
The patient underwent a metastatic work-up for tumor staging. Liver function tests were at the upper limit of normal and a chest X-ray showed a nodule measuring less than 1cm in the lower lobe of the left lung. The patient subsequently underwent a chest CT to further evaluate the lung nodule, which was thought to be a granuloma. Given that she did not have any distant metastases, the decision was made to proceed with an iridocyclectomy.
alternative video link: http://www.youtube.com/watch?v=UTtGUKLNI6M Also see Dr. Alward's Iridocyclectomy video at http://www.youtube.com/watch?v=QeG_mqfqKMA |
.jpg) |
 click on image for more detailed, unlabelled view |
Based on the pathology, the lesion was an amelanotic melanoma involving the iris and ciliary body. It was not possible to determine if the tumor cells were ciliary body or iris in origin and it was concerning that the tumor margins were positive after what appeared grossly to be a complete resection. Given the rapid growth of the lesion and the involvement of the ciliary body (which carries a worse prognosis) it was thought to be in the best interest of the patient to treat the lesion aggressively. After discussion with the patient, the patient elected to have an enucleation of the affected eye. The patient underwent uncomplicated enucleation of the right eye in the following weeks.
She was evaluated by radiation oncology who determined that she did not have detectable distant metastases. They have recommended adjuvant radiation therapy to right eye socket, with repeat chest CT and liver function testing in 3-6 months. She has been tolerating radiation treatment well.
.jpg) |
Uveal melanomas are the most common primary intraocular tumor in adults, most commonly occurring in the choroid. Iris melanomas represent 3-10% of uveal melanomas.(1) Clinically, small malignant melanomas of the iris can be very difficult to differentiate from benign iris nevi. They can range in appearance from off-white to dark brown. Usually iris melanomas are asymptomatic and are noticed by eye care specialists on routine examination. Of the uveal melanomas, the prognosis is best for iris melanomas as they have the lowest rates of metastasis and mortality.
There are several key clinical elements that may suggest malignancy on exam:
With respect to ancillary testing, echography is perhaps the most useful adjunct to the clinical exam. The A-scan technique allows the clinician to assess the lesion's internal reflectivity, vascularity and size. Melanomas typically have low internal reflectivity, a solid tumor pattern and can often have spontaneous vascular pulsations. The B-scan ultrasound can determine the size, position and thickness of the lesion in question.(2)
Given the relatively low rate of metastasis of an iris melanoma, management may involve close observation for signs of growth. Careful documentation and monitoring via photography and echography or ultrasound biomicroscopy is necessary.(3) Fine needle aspiration is sometimes used to obtain biopsy samples to make a tissue diagnosis. This method can yield both false positive and false negative results and does carry with it a small risk of tumor seeding. If it is decided that the lesion is quickly growing and suspicious, surgical resection is often accomplished by sector iridectomy or iridocyclectomy. Occasionally patients are treated with plaque radiotherapy although this method is usually reserved for patients who decline alternative interventions. The prognosis for iris melanoma is excellent as they usually do not metastasize. Lesions less than three clock hours in size have reported rates of extraocular spread of 3% at 5 years, 5% at 10 years, and 10% at 20 years with mortality rates estimated at 1-4%.(4,5)
Ciliary body melanomas grow behind the iris and thus may attain a large size before they are detected. Clinically they are visible only if the pupil is widely dilated or if they grow into the anterior segment. These lesions can remain asymptomatic until they grow enough to affect neighboring ocular structures; if extensive growth occurs patients may present with visual loss, photopsias, or visual field alterations.(6)
Ciliary body melanomas are associated with a worse prognosis than iris melanomas. These lesions have higher rates of metastasis with estimates of 25% at 5 years and 34% at 10 years.(7) The most common sites of metastases for both iris and ciliary body melanomas are the liver and lung. The initial metastatic workup involves checking liver function tests and obtaining a chest X ray. If any of these are abnormal, more extensive tests are undertaken, including liver ultrasound, CT-PET scan or MRI of the abdomen and chest. It has also been hypothesized that many have undetectable micrometastatic disease at the time of their primary diagnosis. For those with metastatic uveal melanoma, survival rates are poor, with a median survival of less than 6 months.(8) Because of the high rates metastases and poorer prognosis, ciliary body melanomas are treated more aggressively and patients often have to undergo enucleation for definitive therapy.
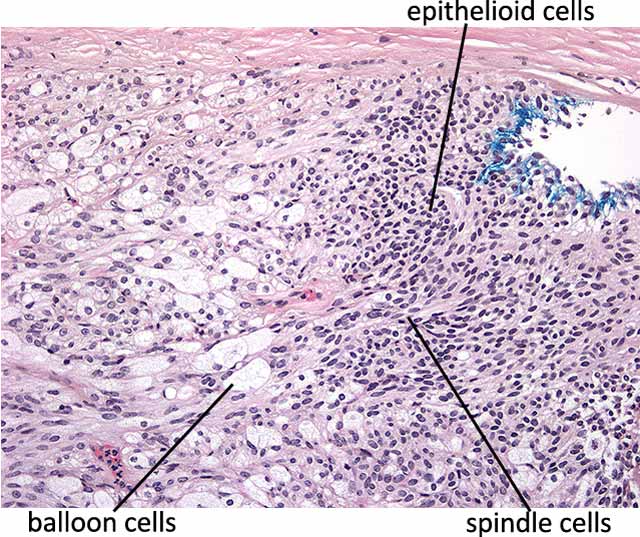
The most important microscopic feature of uveal malignant melanomas that correlates with prognosis is the cell type. As per the Modified Callender Classification, lesions can contain predominantly spindle cells, epithelioid cells, or both.
Several pathologic features correlate with prognosis: Spindle cell melanomas have the best prognosis, followed by mixed cell lesions. Epithelioid cell lesions generally have the worst prognosis. Size smaller than 10 mm in greatest dimension and the absence of extrascleral extension confer a better prognosis than larger lesions. Finally, the intrinsic microvascular pattern has implications for prognosis: A complex pattern associated with microvascular closed loops or networks (3 vascular loops located back-to-back) are associated with increased incidence of subsequent metastasis.(9, 10)
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Rogers GM, Syed NA, Alward WLM, Fernandez de Castro J, Jensen L. Iris-Ciliary Body Melanoma: 57-year-old female with iris lesion. EyeRounds.org. January 15, 2010; Available from: http://www.EyeRounds.org/cases/104-Iris-Ciliary-Body-Melanoma.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.