Chief Complaint: "My right pupil is higher than my left pupil"
History of Present Illness: A 62-year-old female with a one-year history of breast carcinoma status post lumpectomy, chemotherapy and radiation presents to the general ophthalmology clinic for routine follow-up of a symptomatic posterior vitreous detachment in her left eye. She states that over the last year she has noticed that her right pupil is higher than her left. Additionally, she wonders why more sclera is showing under her right iris than under her left. She denies pain or double vision.
Medical History: Infiltrating ductal carcinoma of the breast (Elston-Ellis grade III, ER/PR +, HER-2/neu +) status post right breast lumpectomy with lymph node dissection, chemotherapy and radiation
Medications: Tetracycline, vitamins
Allergies: Morphine, Keflex (cephalexin), codeine, Talwin (pentazocine lactate), Taxol (paclitaxel), mold, milk
Family History: Thyroid disease (mother and sister), post-menopausal breast cancer (mother and maternal aunt), lung cancer (father), prostate cancer (brother), ovarian cancer (sister)
Social History: Works as a nursing coordinator at a local college
 |
The patient was referred to the oculoplastics service and found to have 2 mm of right eye proptosis as well as right hyperglobus with inferior scleral show. Given her history of cancer, there was concern for a possible metastatic orbital mass. Contrast-enhanced CT of the orbits was performed and showed a well-demarcated 1.6 cm soft tissue density in the inferior lateral aspect of the right orbit. There was some minimal scalloping of adjacent lateral orbital wall. Although the mass had a benign appearance, the patient requested removal after reviewing the risks and benefits.
A right lateral orbitotomy was performed with excisional biopsy of the mass. Pathologic examination showed an encapsulated mass consisting of irregular, thin-walled vascular spaces. The spaces were filled with red blood cells. Radiographic and pathologic findings were consistent with cavernous hemangioma of the orbit.
Cavernous hemangioma is the most common primary orbital tumor in adults (Cohen 2009). It is classically a well-circumscribed unilateral intraconal mass seen in middle-aged women. It is not uncommon for these to be found incidentally after imaging is performed for another condition (e.g. headaches, seizures, etc.). The clinical hallmark is a slowly progressive, painless proptosis, but patients may also present with vision loss either due to optic nerve compression or hyperopic shift when the mass compresses the posterior pole. In the latter case, choroidal folds may be seen on fundus exam. As with any space occupying lesion in the orbit, patients may also note diplopia. Given the slow progression of cavernous hemangiomas, patients, as ours did, may be able to fuse deviations that would have produced diplopia if onset were acute.
Histopathologically, these tumors are thought to be congenital vascular hamartomas, though there is some speculation regarding an acquired etiology. They account for approximately 80% of orbital vascular tumors and invariably take a benign course in contrast to hemangiopericytomas, which can mimic cavernous hemangioma both in presentation and on imaging (Kikuchi et al 1994).
CT, MRI and echography have all been studied for the evaluation of cavernous hemangioma (Thorn-Kany et al 1999, Dallaudiere et al 2009). Choice of imaging depends on clinical suspicion, but the authors feel that CT with contrast is a good first choice as this will yield information about the shape, vascularity, consistency, and margins of the lesion as well as adjacent bony changes. Some studies report that MRI can be helpful in differentiating between schwanomma, hemangiopericytoma, and cavernous hemangioma (Xian et al 2010, Kikuchi 1994). Coronal images are useful to assess position of the lesion relative to the optic nerve (see Figure 9). Some general imaging characteristics are highlighted below.
CT appearance: Well-defined oval or round mass roughly isodense to muscle. Hyperdense areas within the lesion may correspond to areas of thrombosis termed "phleboliths." Contrast enhancement is homogenous but fills slowly.
MRI appearance: T1-weighted imaging: Homogeneous signal isointense to muscle.
T2 weighted imaging: Homogeneous signal hyperintense to muscle best seen with fat suppression.
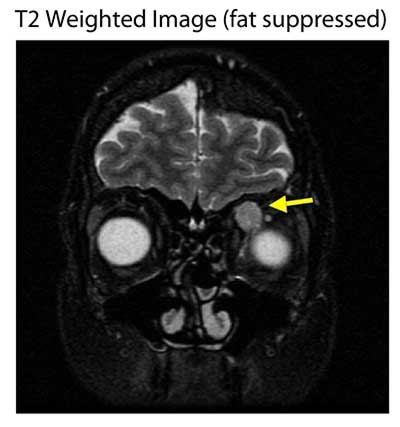 |
In summary, lesions are easiest to see either on non-contrast-enhanced T1 images without fat suppression, fat-suppressed T2 images, or T1 fat-suppressed contrast-enhanced images (Ruchman and Flanagan 1983, Thorn-Kany et al 1999).
If history, exam and imaging studies are consistent with cavernous hemangioma it is reasonable to observe without obtaining a tissue diagnosis. In the majority of cases there is little change in the appearance of the lesion as demonstrated by the CT scan below. However, patients should be monitored with imaging every 1-2 years for the first five years after diagnosis to confirm stability. If the lesion is stable after five years, then there is no need to reimage unless there are any new clinical findings.
However, in the setting of known malignancy (such as in this case) or rapid progression in size, biopsy is reasonable to rule out other etiologies for the mass. In addition, diplopia, optic nerve compression and choroidal folds are indications for removal. Excision is usually not necessary depending on the size and location of the lesion and in the absence of vision loss. Complete excision can usually be achieved with relative ease due to the encapsulated nature of these lesions.
Diagnosis: Cavernous hemangioma
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Ward MS, Allen R. Painless Proptosis in a 62-year-old female. EyeRounds.org. July 7, 2010; Available from: http://www.EyeRounds.org/cases/112-painless-proptosis.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.