Chief Complaint: Double vision and a droopy eyelid
History of Present Illness: A 63-year-old female presented to the ophthalmology clinic at the University of Iowa Hospitals & Clinics after three months of gradually progressive double vision and a droopy right eyelid. She had binocular oblique diplopia, worse when looking to the right. Her symptoms were constant and did not fluctuate with activity or the time of day.
She denied any difficulty swallowing, weakness, shortness of breath, or trauma.
Past Ocular History: Wears spectacles. No ocular surgery or trauma.
Medical History: Negative
Medications: None
Family History: Father died of esophageal cancer.
Social History: 60 pack-year history, quit at age 44. Used to work in a factory.
 |
 |
This patient’s presentation of enophthalmos in the setting of three months of slowly progressive ptosis and diplopia was concerning for an orbital mass. Computed tomography (CT) with intravenous contrast was performed and revealed right enophthalmos and an ill-defined intraconal lesion in the right orbit, inseparable from the medical rectus and abutting the optic nerve.
 |
 |
The patient underwent right anterior orbitotomy and biopsy of the intraconal mass. Pathologic examination revealed a dense infiltrate of spindle shaped to round cells with scant cytoplasm and hyperchromatic nuclei. The cells demonstrated an infiltrative growth pattern. Immunohistochemistry testing was positive for estrogen and progesterone receptors. Carcinoembryonic antigen (CEA) demonstrated focal positivity. Pancytokeratin, AE1/3, and Cytokeratin 7 were also positive. CD45 and S100 were negative. These findings were consistent with a poorly differentiated carcinoma with a growth pattern and immunophenotype most consistent with metastatic neoplasm, likely breast or ovary.
The patient was referred to the oncology service for a systemic workup. On further history, her last mammogram was 10 years ago and reportedly normal except for some calcification in the left breast. She had not noticed a breast mass but reported having an inverted right nipple for the past year. She had not sought any medical attention for it. She denied any skin change or nipple discharge. She had menarche at the age of 12 and menopause at the age of 50. She had never been pregnant. Physical examination of the right breast revealed an inverted nipple without discharge and a 10 cm x10 cm mass underneath the nipple which was hard and immobile.
Mammogram revealed suspicious clusters of microcalcifications in both breasts.
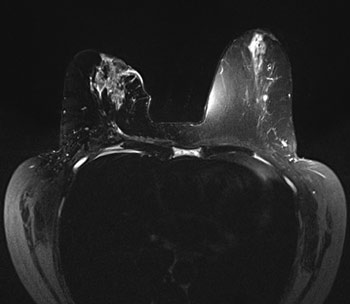
Magnetic resonance imaging (MRI) of the breast revealed a large right retroareolar mass with skin and nipple retraction and right axillary lymphadenopathy highly suspicious for metastatic breast cancer.
 |
MRI of the brain revealed diffiuse metastatic disease to the calvaria and upper cervical spine. Positron emission tomography (PET) revealed radiotracer activity in the right axilla, the right breast, the omentum, axial skeleton, and moderate ascites.
To confirm the diagnois, a core needle biopsy was performed which was consistent with invasive lobular carcinoma. The tumor was estrogen and progesterone receptor positive and Her2/neu negative.
The patient was started on the aromatase-inhibitor anastrozole (Arimidex) and the bisphosphonate zoledronic acid (Zometa). She was referred to radiation oncology who decided to treat the right orbital lesion with 30 Gy in 10 fractions in an effort to preserve the eye.
After a few doses of radiation, the patient’s diplopia had midly improved. Her ptosis and enophthalmos were stable. She had new complaints of dry eye and was treated with aggressive lubrication and lower punctal occlusion.
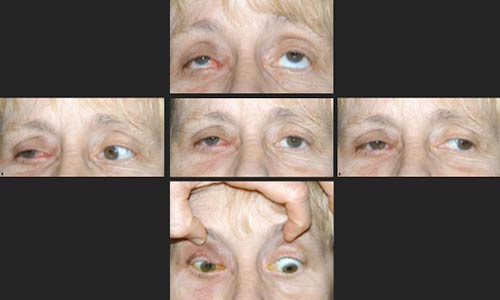 |
Enophthalmos is retrodisplacement of the eye within the orbit. It is a subtle ophthalmological sign and less common than proptosis. Enophthalmos can be subjectively appreciated by visualizing the anterior-posterior position of the globes from an inferior perspective while the patient looks superiorly. Objectively, it is quantified by exophthalmometry, which measures the anterior-posterior distance from the lateral orbital rim to the corneal apex. A difference of more than 2 mm between the orbits is abnormal.
Enophthalmos can be caused by two mechanisms: an increase in the size of the orbit or a decrease in the volume of the orbital contents. The size of the orbit may be increased by trauma (a large floor fracture), congenital abnormalities, chronic sinusitis with orbital wall destruction, silent sinus syndrome, silent brain syndrome, and congenital absence of the sphenoid wing as in neurofibromatosis (1, 2, 3). The volume of the orbital contents may be decreased by microphthalmos, orbital fat atrophy (post-radiation, post-hemorrhage, self-inflicted orbital trauma), scirrhous tumors (breast cancer), post-inflammatory changes, and post-surgical (extraocular muscle resection) changes. Of these causes, congenital orbital asymmetry and trauma are the most common (4).
Scirrhous metastatic breast cancer is the most common malignant condition that should be ruled-out in a female who presents with enophthalmos. In a review of 25 cases of orbital metastasis presenting with enophthalmos, 76% were caused by breast carcinoma. The other 24% originated from stomach, colon, or pancreatic cancers (5). In another series of 70 patients with orbital metastasis, 8 presented with enophthalmos and all of them had scirrhous breast carcinoma (6).
The level of suspicion for malignancy is greater if there are accompanying symptoms such as diplopia and ptosis. The classic triad of enophthalmos, ptosis, and restricted ocular motility is present in 32% of patients with metastatic breast carcinoma to the orbit (6). Patients may also have downgaze "hang-up," whereby the lid is retracted in downgaze, and reduced levator function, due to malignant infiltration of superior orbital tissues (7).
Ophthalmologists can be the first to diagnose some of these life-threatening illnesses. In a review of 28 cases of orbital metastases, 61% of patients had symptoms of orbital metastasis before the primary tumor was detected. Breast cancer was the most frequent primary tumor identified (8).
‘Scirrhous’ means hard or indurated. In the context of metastatic breast cancer, it describes the the contraction of fibroblasts and subsequent posterior retraction and tethering of the globe that causes enophthalmos. It is a paradoxical phenomenon. Henderson writes in his 1980 textbook Orbital Tumors: "...as the disease progresses, rather than proptosis, chemosis, and tissue reaction characteristic of other adenocarcinomas, the picture is one of the muscles, nerves, and surrounding soft tissues becoming so entwined and infiltrated by the scirrhous tumor that the helpless eye soon is immobilized and pulled posteriorly."
The workup of suspected metastatic scirrhous breast cancer to the orbit includes a complete history and physical, imaging of the orbit (CT or MRI), mammogram, orbital mass biopsy and body imaging for metastatic disease. These patients require a multi-disciplinary approach with general practitioners, medical oncologists, radiation oncologists and surgeons.
The prognosis for patients with orbital metastasis is usually poor due to the advanced nature of the cancer. The median survival time ranges from 5 to 17 months (9, 10). However, there have been some reports of long survival with no detectable disease in other organs for years (11).
Treatment of the orbital metastasis usually consists of external beam radiation, which may palliate symptoms and preserve vision. Enucleation does not affect prognosis, and is reserved for patients with intractable pain or hygiene issues. Exenteration is also not curative so it is rarely performed due to cosmesis issues. The systemic disease is often treated with chemotherapy, estrogen antagonists (based on receptor status), and bisphosphonates when bony metastasis is present.
Epidemiology
|
Signs
|
Symptoms
|
Treatment
|
Risma JM, Sobel RK, Allen RC. Enophthalmos Secondary to Metastatic Breast Cancer. EyeRounds.org. December 23, 2011; Available from: https://eyerounds.org/cases/144-breast-cancer.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.