History of Present Illness: The patient is a 4-year-old girl who presented to her local eye doctor for routine preschool screening and was found to have central posterior synechiae in both eyes (OU), for which she was started on Atropine 1% OU for 6 weeks. On follow-up, she was found to have macular edema and was referred to pediatric rheumatology for further systemic evaluation with suspicion of inflammatory etiology, and subsequently to pediatric ophthalmology.
Past Ocular History: None
Past Medical History:
Medications: amoxicillin 400 mg orally, twice daily (BID) for an upper respiratory infection
Allergies: None
Family History: Positive for maternal aunt with psoriasis, otherwise non-contributory.
Social History: Patient lives with her parents. There are no pets in the household.
Review of Systems: Positive for a small, round, recurrent rash on the left forearm. Otherwise, negative in detail, including no joint pain.
Visual Acuity: 20/20 right eye (OD) and 20/25 left eye (OS)
Current refraction: +2.00 sphere OD and OS
Pupils: 5 mm in dark, 3 mm in light OU without relative afferent pupillary defect
Extraocular movements: Full OU
External: Normal
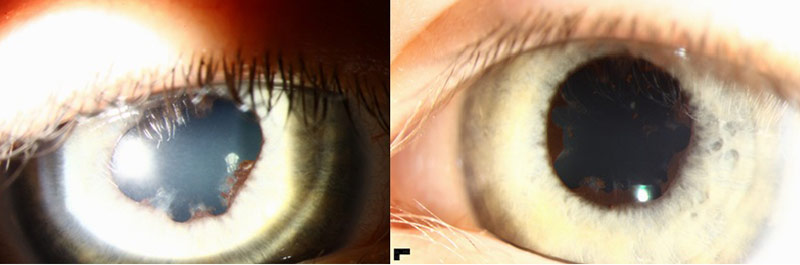
Slit Lamp Exam: Normal lids and lashes OU, trace injection OU, corneas clear, anterior chambers with 1+ flare and no cell OU, central posterior synechiae OU (Figure 1), lenses show pigment deposits on anterior lens capsule OU
 |
Dilated Fundus Exam: Bilaterally normal discs, macula, vessels and periphery. No cystoid macular edema (CME) seen.
Musculoskeletal exam: Notable for thickening and fullness of the left ankle, incomplete extension with flexion contraction of right elbow to 70 degrees with thickening felt at medial epicondyle. No pain or warmth noted. Otherwise unremarkable.
ANA |
Positive at 1:160, diffuse pattern |
|---|---|
Angiotensin-1 converting enzyme |
60 U/L (normal 8-52 U/L) |
Lyme disease antibody (IgG/IgM) |
Negative |
Erythrocyte sedimentation rate |
14 mm/hr (normal 0-20 mm/hr) |
HLA-B27 typing |
Negative |
Serum IgA |
59 mg/dL (normal 27-195 mg/dL) |
Serum IgG |
667 mg/dL (normal 504-1464 mg/dL) |
Urinalysis |
Unremarkable |
Based on the patient’s lack of cells in the anterior chamber, CME on exam and poor cooperation with OCT testing, it was decided to defer topical steroids in lieu of a repeat exam in one month.
Visual Acuity: 20/25 right eye (OD) and 20/20 left eye (OS)
Intraocular pressure: 8 mmHg OD, 13 mmHg OS by iCare
Current prescription: +2.50 sphere OD, +2.00 +0.50 x 015 OS
Pupils: 5 mm in dark, 3 mm in light OU without relative afferent pupillary defect
Extraocular movements: Full OU
External: Normal
Slit Lamp Exam: Normal lids and lashes OU, conjunctive clear and quiet OU, corneas show band keratopathy temporally with fine keratic precipitates OU, anterior chambers with 2+ flare and 2+ cell OU, normal iris architecture OU, lenses show pigment deposits on anterior lens capsule OU
Dilated Fundus Exam: Blunted foveal light reflex OD, normal macula OS. Bilaterally normal discs, vessels and periphery.
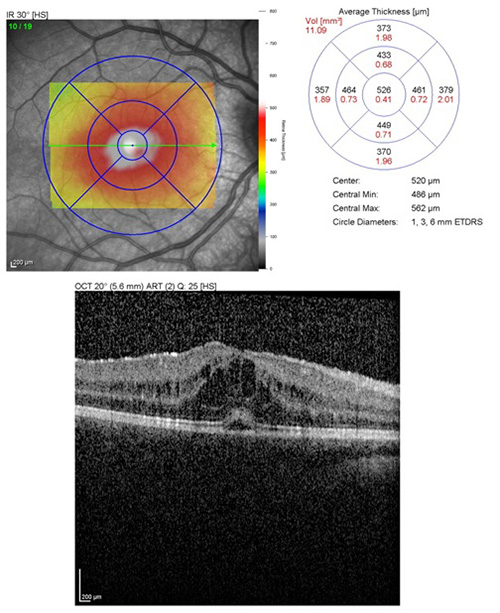
Optical coherence tomography: Florid CME OD with central macular thickness of 634 microns (Figure 2); central macular thickness OS 330 microns, no intraretinal or subretinal fluid.
 |
The patient was begun on Pred Forte® (prednisolone acetate ophthalmic suspension, USP, 1%) OU every 2 hours while awake, ketorolac OU four times daily and atropine OU at bedtime. Patient was seen by the pediatric rheumatology service later that day, and after a long discussion with the patient’s parents, it was decided to begin methotrexate 25 mg subcutaneously weekly with 1 mg of folic acid daily.
Visual Acuity: 20/25 right eye (OD) and 20/30 left eye (OS)
Intraocular pressure: 33 mmHg OD, 27 mmHg OS by iCare
Current prescription: +2.50 sphere OD, +1.75 +0.75 x 018 OS
Pupils: 7mm in dark and light OU due to pharmacologic dilation
Extraocular movements: Full OU
External: Normal
Slit Lamp Exam: Normal lids and lashes OU, conjunctiva clear and quiet OU, corneas show early band keratopathy temporally with fine keratic precipitates OU, anterior chamber showed 1+ flare and no cell OD and trace flare with no cell OS, iris showed multiple posterior synechiae OU, lenses show pigment deposits on anterior lens capsule OU
Dilated Fundus Exam: 1+ vitreous flare without cell OU, bilaterally normal discs, macula, vessels and periphery. No macular edema.
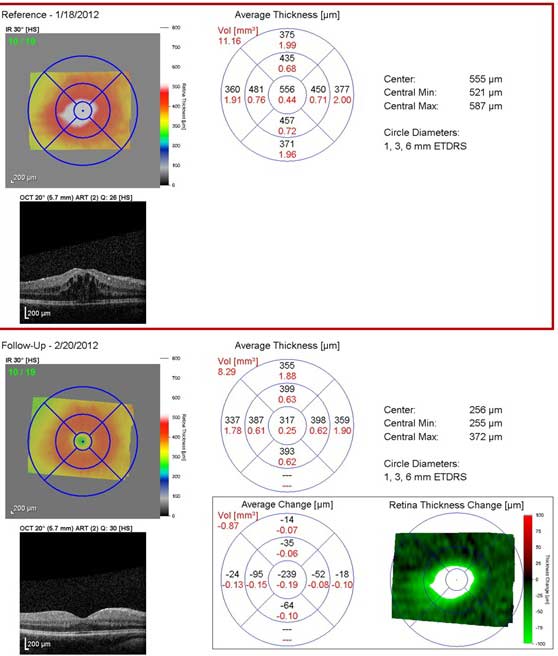
Optical coherence tomography: OD: Central macular thickness 317 microns (was 634 microns) with total resolution of CME (Figure 3); OS: central macular thickness 302 microns (was 330 microns), no CME.
 |
The patient was started on Cosopt® (Dorzolamide and Timolol Ophthalmic) OU twice daily for steroid-induced ocular hypertension, Pred Forte was decreased to every 3 hours OU while awake, ketorolac was continued four times daily in the right eye only, and atropine was stopped.
Visual Acuity: 20/30 right eye (OD) and 20/30 left eye (OS)
Intraocular pressure: 13 mmHg OD, 13 mmHg OS by iCare
Current prescription: +2.50 sphere OD, +1.75 +0.75 x 018 OS
Pupils: 5 mm in dark, 3 mm in light OU without relative afferent pupillary defect
Extraocular movements: Full OU
External: Normal
Slit Lamp Exam: Normal lids and lashes OU, conjunctiva clear and quiet OU, cornea clear OD and early band keratopathy OS with interval resolution of fine keratic precipitates OU, anterior chamber showed trace to 1+ flare and no cell OD and trace flare with trace to 1+ cell OS, iris showed multiple posterior synechiae OU, lenses show pigment deposits on anterior lens capsule OU
Dilated Fundus Exam: 1+ vitreous flare without cell OU, bilaterally normal discs, macula, vessels and periphery. No macular edema.
Optical coherence tomography: OD: Central macular thickness 301 microns (was 317 microns) with total resolution of CME; OS: central macular thickness 295 microns (was 302 microns), no CME.
The patient’s Pred Forte® was increased back to every 2 hours OU while awake due to recurrence of anterior inflammation in the left eye, and ketorolac and Cosopt® were continued.
On subsequent follow-up exams, the patient had stable inflammation with trace to 1+ flare and no cell OD and 1+ flare and trace cell OS without recurrence of macular edema. The patient’s Pred Forte® was decreased to OU four times daily. Four weeks later, patient had stable mild anterior chamber inflammation, and Pred Forte was tapered to OU twice daily, and ketorolac and Cosopt® were continued.
Diagnosis: Juvenile idiopathic arthritis with associated bilateral anterior uveitis
Uveitis is commonly associated with juvenile idiopathic arthritis, most commonly in the oligoarticular category, in which 2-4 joints are involved, within the first 6 months of diagnosis. Additional risk factors include female sex, positive ANA, and negative rheumatoid factor. Unlike uveitis in adults, which often presents with pain, photophobia and redness of the eye, JIA-associated uveitis in children can present with a quiet-appearing eye. Due to the asymptomatic nature, it is important to follow recommended uveitis screening guidelines for children with JIA. After initial ophthalmologic examination at the time of JIA diagnosis, the frequency of follow-up eye exams in patients with JIA is determined by their risk category (Cassidy et al., 2006). High-risk patients, who have positive ANA, are 6 years old or less at onset of joint disease and have had JIA for 4 years or less should be examined every 3 months. Moderate and low risk patients are determined based on a combination of ANA status, age at onset, and duration of disease (Cassidy et al., 2006). Patients with moderate risk should be examined every 6 months, and low risk patients should be examined every 12 months, as shown in Table 1.
| Type | ANA |
Age at Onset (years) |
Duration of Disease (years) |
Risk Category |
Frequency of Eye Exams |
Oligoarthritis or polyarthritis |
+ |
≤ 6 |
≤ 4 |
High |
3 months |
+ |
≤ 6 |
> 4 |
Moderate |
6 months |
|
+ |
≤ 6 |
> 7 |
Low |
12 months |
|
+ |
> 6 |
≤ 4 |
Moderate |
6 months |
|
+ |
> 6 |
> 4 |
Low |
12 months |
|
- |
≤ 6 |
≤ 4 |
Moderate |
6 months |
|
- |
≤ 6 |
> 4 |
Low |
12 months |
|
- |
> 6 |
N/A |
Low |
12 months |
|
Systemic disease |
N/A |
N/A |
N/A |
Low |
12 months |
Approximately 10% of patients with oligoarticular JIA have uveitis (Kotaniemi et al., 1999), with 37.3% of JIA-associated uveitis patients experiencing complications from the disease or associated steroid-treatment, such as cataract, posterior synechiae, band keratopathy, glaucoma, or macular edema (listed in decreasing order of incidence) (Sabri et al., 2008). Macular edema was found to occur in 5.6% of 147 children with JIA-associated uveitis, or 3.9% of eyes, as the majority of patients had bilateral uveitis, but less commonly bilateral macular edema (Sabri et al., 2008).
The treatment of JIA-associated chronic uveitis is largely based on clinical course, but basic recommendations exist to guide therapy (Heiligenhaus et al., 2012). Patients presenting with uveitis in the setting of JIA are initially started on topical corticosteroid. If there are prognostic factors of impending vision loss such as poor initial vision, hypotony, glaucoma, cataract, macular edema, or dense vitreous opacities, it is also recommended that systemic corticosteroids are begun, at a dosage of 1-2 mg/kg, and tapering to <0.15 mg/kg within 4 weeks. Oral corticosteroids should be limited to 3 months use secondary to systemic complications, and similarly, topical corticosteroid should be limited to no more than 3 drops per day for chronic use due to risk of cataract and glaucoma. If the uveitis remains active or reactivates within these guidelines, steroid sparing agents should be begun.
Methotrexate, a folate analogue which inhibits a key step in DNA synthesis, is currently the preferred steroid sparing agent in JIA-associated uveitis (Heiligenhaus et al., 2012). Several studies have shown its effectiveness in treating chronic uveitis. Malik et al, 2005, examined the use of low-dose methotrexate in ten children with bilateral chronic anterior and intermediate uveitis. This study found significantly better visual acuity, decrease in anterior chamber inflammation, topical corticosteroid frequency, and oral steroid use than prior to using methotrexate. This study, however, did not include any patients with JIA-associated uveitis. Weiss et al., 1998, reported on seven children with JIA-associated chronic uveitis treated with methotrexate, and 6/7 were found to have a significant reduction in the severity of uveitis, based on the number of cells seen in the anterior chamber. Foeldvari and Wierk, 2005, performed a retrospective chart view of 25 patients with chronic JIA-associated uveitis who were treated with methotrexate. Twenty-one of the 25 patients responded to methotrexate therapy, and in 6 of these patients, methotrexate was discontinued due to continuous remission. There was one case of cystoid macular edema in a 13-year-old patient in Malik et al.'s study, which resolved with methotrexate treatment, although this patient's uveitis was not associated with JIA. There were no cases of macular edema among the JIA-associated uveitis cases treated with methotrexate in the above studies.
Pato et al., 2011, have studied the effect of immunosuppressants and biological therapies in treating posterior autoimmune uveitis and its complications. In this systematic review, they found several studies which have effectively treated macular edema. The agents that were found to be effective include cyclosporine, infliximab, daclizumab, INF-alpha-2a, acetazolamide and methylprednisolone. There was no report of which medications were found to be ineffective in treating macular edema. There were no studies found in which the effect of methotrexate on macular edema associated with posterior uveitis was evaluated.
We present a case in which a 4-year-old girl with oligoarticular JIA and associated chronic uveitis developed a vision threating complication of macular edema and was successfully treated with methotrexate for her arthritis, and macular edema. The patient was treated with topical corticosteroids and ketorolac for her ocular inflammation, and in conjunction with the methotrexate, she did not need any other therapies for macular edema, such as intravitreal or periocular steroid, which would be difficult to administer in a 4-year-old child without general anesthesia. Interestingly, she was not begun on oral steroids prior to starting methotrexate, based on the established aggressive course of her disease.
Differential Diagnosis: HLA-B27 associated uveitis, HSV uveitis, Lyme disease uveitis, syphilitic uveitis, tuberculosis uveitis, tubulointerstitial nephritis and uveitis (TINU), idiopathic uveitis.
Signs
|
Risk Factors for Uveitis
|
Symptoms
|
Treatment
|
Recommended screening: At first diagnosis of JIA, then every 3-12 months, based on risk category, which is determined by ANA, age at onset of disease, and duration of disease, as shown in Table 1, above.
Cassidy J, Kivlin J, Lindsley C, Nocton J, Section on Rheumatology and Section on Ophthalmology.
Ophthalmologic examinations in children with juvenile rheumatoid arthritis. Pediatrics. 2006 May;117(5):1843-5.
Foeldvari I, Wierk A. Methotrexate is an effective treatment for chronic uveitis associated with juvenile idiopathic arthritis. J Rheumatol. 2005; 32:362-365.
Heiligenhaus A, Michels H, Schumacher C, Kopp I, Neudorf U, Niehues T, Baus H, Becker M, Bertram B, Dannecker G, Deuter C, Foeldvari I, Frosch M, Ganser G, Gaubitz M, Gerdes G, Horneff G, Illhardt A, Mackensen F, Minden K, Pleyer U, Schneider M, Wagner N, Zierhut M. Evidence-based, interdisciplinary guidelines for anti-inflammatory treatment of uveitis associated with juvenile idiopathic arthritis. Rheumatol Int. 2012 May; 32(5):1121-33.
Heiligenhaus A, Mingels A, Heinz C, Ganser G. Methotrexate for uveitis associated with juvenile idiopathic arthritis: value and requirement for additional anti-inflammatory medication. Eur J Ophthalmol. 2007; 17:743-748.
Kotaniemi K, Kaipiainen-Sepp-nen O, Savolainen A, Karma A. A population-based study on uveitis in juvenile rheumatoid arthritis. Clin Exp Rheumatol. 1999 Jan-Feb; 17(1):119-22.
Malik AR, Pavesio C. The use of low dose methotrexate in children with chronic anterior and intermediate uveitis. Br J Ophthalmol. 2005; 89:806-808.
Pato E, Munoz-Fernandez S, Francisco F, Abad MA, Maese J, Ortiz A, Carmona L; Uveitis Working Group from Spanish Society of Rheumatology. Systematic review on the effectiveness of immunosuppressants and biological therapies in the treatment of autoimmune posterior uveitis. Semin Arthritis Rheum. 2011 Feb; 40(4):314-23.
Sabri K, Saurenmann RK, Silverman ED, Levin AV. Course, complications, and outcome of juvenile arthritis-related uveitis. J AAPOS. 2008 Dec; 12(6):539-45.
Weiss AH, Wallace CA, Sherry DD. Methotrexate for resistant chronic uveitis in children with juvenile rheumatoid arthritis. J Pediatr. 1998; 133:266-268.
Kemp PS, Longmuir SQ. Juvenile idiopathic arthritis with associated bilateral anterior uveitis in a four-year old girl. EyeRounds.org. Posted August 14, 2012. Available from http://www.EyeRounds.org/cases/154-JIA-associated-uveitis-macular-edema.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.