Chief Complaint: Double vision and a droopy left upper eyelid
History of Present Illness: A 49-year-old man with a history of multiple myeloma in remission, status post autologous stem cell transplant, presented to the Neuro-Ophthalmology clinic at the University of Iowa Hospitals & Clinics with a 1-2 month history of progressively-increasing diplopia and ptosis of the left upper eyelid. The diplopia was oblique and constant, and resolved upon closing either eye. He had not noticed any fluctuation of the diplopia or ptosis. However, he also complained of right arm coordination difficulties. At the time of presentation, the patient was receiving multiple myeloma remission maintenance therapy with low-dose prednisone.
He denied headaches, vision loss, fevers, sweats, and rigors.
Confrontation visual fields: Full OU
External exam: Normal
The optic nerves appeared healthy with a 0.3 cup-to-disc ratio. The macula was normal OU. The vessels and peripheral exam were normal OU.
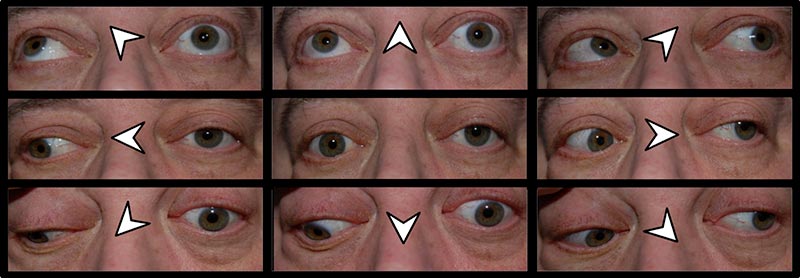 |
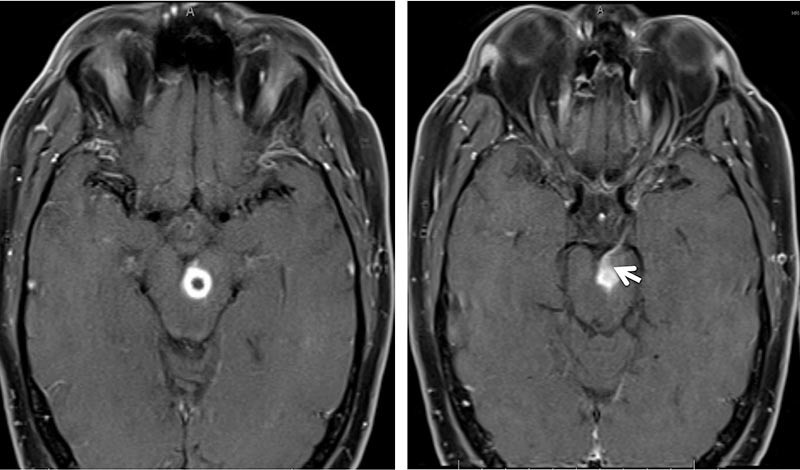
This patient's presentation with a partial progressive pupil-involving third nerve palsy with contralateral hemiplegia was concerning for a midbrain lesion. MRI brain with contrast was performed and revealed a ring-enhancing lesion with associated vasogenic edema in the left side of the midbrain, involving the left third nerve fascicle and medial left cerebral peduncle (Figures 2 and 3). No other intra-axial lesions were identified. MRA head with contrast was unremarkable.
 |
 |
The patient was admitted to the Neurology service. With guidance from the Infectious Disease team, the patient had a full work-up for infectious, inflammatory, and neoplastic sources which included:
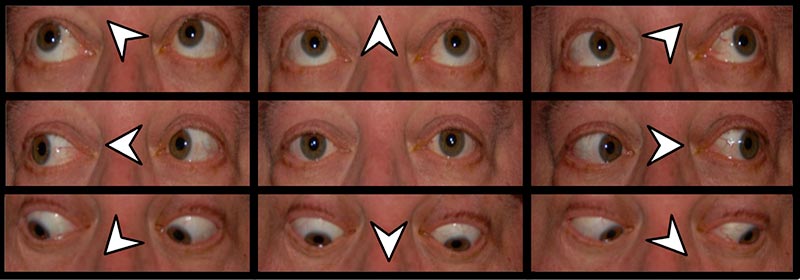
The workup was unrevealing, except for a weakly-positive Beta-D-Glucan Assay, which suggested a fungal etiology. Although a biopsy would have provided significant information regarding the etiology of the lesion, it was considered too risky given the difficult to access location and high likelihood of causing a greater and irreversible neurologic deficit. Therefore, empiric treatment with voriconazole and caspofungin was initiated. The treatment was subsequently changed to posaconazole, as the patient developed severe photosensitivity with the voriconazole (1). Serial Beta-D-Glucan measurements demonstrated a two-fold decease over a two week period. The patient was re-evaluated in the Neuro-Ophthalmology clinic 2 months after the initiation of anti-fungal therapy. During that visit, he showed a dramatic improvement in motility, with full adduction and marginally limited supraduction and infraduction of the left eye (Figure 4). Pupils were equal and briskly reactive to light. Almost complete resolution of his ptosis was also noted.
 |
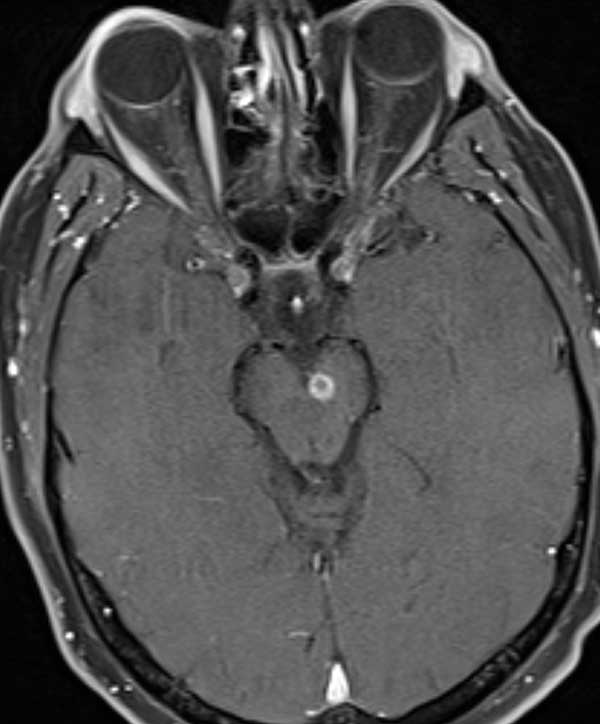 |
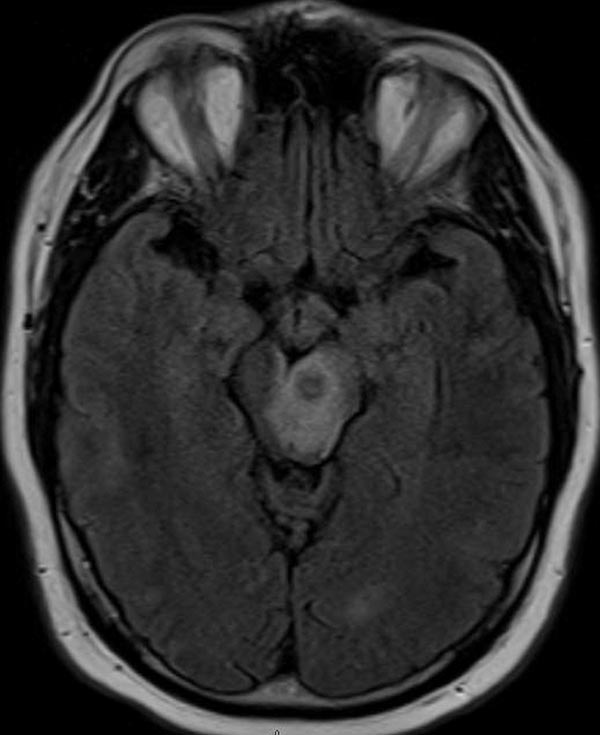
The patient was continued on posaconazole and scheduled for brain MRI with contrast and Neuro-Ophthalmology follow-up in 3 months. MRI demonstrated a drastic reduction in the size of the ring-enhancing lesion and associated vasogenic edema (Figure 5). The radiographic improvement correlated with clinical improvement as well. Motility was noted to be full, except for minimal residual limitation of supraduction. Pupils were equal and briskly reactive to light.
Based on his examination findings of a partial, pupil-involving third nerve palsy with contralateral hemiplegia, the lesion could be localized to the midbrain prior to imaging. Once focused to the midbrain, additional signs/symptoms allowed for more specific localization within the midbrain. The presence of a left-sided third nerve palsy and right sided pyramidal signs suggested a left midbrain lesion. Weakness of the right upper extremity with a negative Babinski sign of the right lower extremity indicated involvement of the upper extremity, but sparing the lower extremity. This allowed localization of the lesion to the medial cerebral peduncle, due to its topographical arrangement (upper extremity-medial, lower extremity-lateral). Finally, the posterior boundary of the lesion could be determined by observing whether the medial lemniscus (contralateral loss of two-point discrimination, vibration, and proprioception) or the superior cerebellar peduncle (contralateral ataxia) was involved (2,3). Because the patient did not demonstrate any of these findings, the lesion was localized anterior to the medial lemniscus and the superior cerebellar peduncle. Therefore, the clinical symptoms and signs allowed for localization of the lesion to the left side of the midbrain, involving the medial cerebral peduncle and third nerve fascicle. Note that this patient could also be described as having Weber Syndrome, a third nerve fascicular syndrome occurring due to involvement of the cerebral peduncle and the adjacent third nerve fasciculus (4). Other third nerve fascicular syndromes are listed in the table below.
The differential diagnosis for a ring enhancing lesion in an immunocompromised individual can be separated into three major categories: infectious, neoplastic, or inflammatory (5). During the work-up of this patient, investigations for bacterial, viral, parasitic, inflammatory, and neoplastic etiologies all came back negative. Only the Beta-D-Glucan assay was positive. This assay measures 1,3-Beta-D-Glucan, which is a component of the cell wall of most fungi, excluding Cryptococcus, Zygomycetes, and the yeast form of Blastomyces (sensitivity 50%, specificity 99%) (6,7). Serial measurements of Beta-D-Glucan levels were utilized in order to monitor response to therapy. In this case, a decrease in Beta-D-Glucan levels seemed to correlate with both radiologic and clinical improvement, although there is no current literature addressing the utility of following Beta-D-Glucan levels to monitor patient response to therapy.
Because the Beta-D-Glucan Assay suggested that the lesion was a fungal abscess, empiric treatment with voriconazole and caspofungin was initiated. Voriconazole was chosen due to its efficacy against invasive aspergillus and broad-spectrum of anti-fungal coverage. In 2008, the Infectious Disease Society of America advised that voriconazole was superior to amphotericin B for treatment of invasive aspergillus (8). Although there is limited evidence to support the use of voriconazole over amphotericin B for invasive fungal infections other than aspergillus, it was felt to be adequate because of its broad-spectrum of action and less severe side-effects compared with amphotericin B. Combination therapy with caspofungin was also utilized in this case during the first four weeks, even though there are limited studies to suggest that combination therapy is superior to monotherapy (9). During treatment, the patient experienced photosensitivity, a well-characterized side-effect of voriconazole treatment and, thus, was switched to posaconazole. When compared with voriconazole, posaconazole has a similar broad-spectrum of activity, but lacks efficacy against invasive aspergillus. Since CNS fungal infections can be difficult to cure, this patient will remain on posaconazole treatment long-term until radiologic signs of the lesion are no longer evident.
Diagnosis: Third Nerve Palsy with Contralateral Hemiplegia Secondary to Midbrain Fungal Abscess
Epidemiology of a midbrain fungal abscessImmunocompromised Individuals
|
Signs of a 3rd nerve palsy from a fascicular midbrain lesion
|
Symptoms of a 3rd nerve palsy from a fascicular midbrain lesion (10)
|
Treatment of a midbrain fungal abscessOptions Include one of the following:
|
Baldwin A, Thurtell MJ. Third Nerve Palsy with Contralateral Hemiplegia Secondary to Midbrain Fungal Abscess. EyeRounds.org. September 5, 2012. Available from: https://eyerounds.org/cases/156-Fungal-abscess-causing-3rd-nerve-palsy.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.