Decreased vision after cataract surgery
65-year-old female who presented to the contact lens clinic because she was unhappy with her vision after cataract surgery. She was a contact lens wearer prior to her cataract surgery and had tried 14 different pairs of contact lenses since surgery with no improvement in her vision. She was uncomfortable in glasses because images appeared trapezoidal.
She had cataract extraction with lens implantation right eye (OD) and left eye (OS) about 18 months prior in summer of 2010. Prior to surgery, she was in monovision contact lenses with the right eye set for distance and the left eye for near. She had worn rigid gas permeable (RGP) contact lenses since age 16. She had always been happy with her RGP contact lenses, and she never liked wearing glasses. She wanted to continue to wear RGP contact lenses after the cataract surgery.
Visual acuity (VA) at distance with contact lens correction
Manifest refraction
Manual keratometry
She was fit with a bitoric RGP lens in each eye, but even after ordering several lenses, the best visual acuity that could be obtained was 20/40. (See table 1 and discussion of RGP lenses for astigmatism below.) It was felt that optimal vision could not be obtained using the bitoric RGP lenses. She was referred to the comprehensive ophthalmology clinic for evaluation of an intraocular lens (IOL) exchange.
| Follow-up | Visual acuity (with contact lens) |
Plan |
|---|---|---|
Initial visit |
OD 20/40 OS 20/100 |
Fit with bitoric RGP lens |
6 week return |
OD 20/70 OS 20/60 |
Good lens fit, adjusted lens power |
8 week return |
OD 20/50 OS 20/50 |
Adjusted lens power, ordered monovision |
10 week return |
OD 20/40 OS J5 |
Referral to comprehensive ophthalmology clinic |
OD
OS
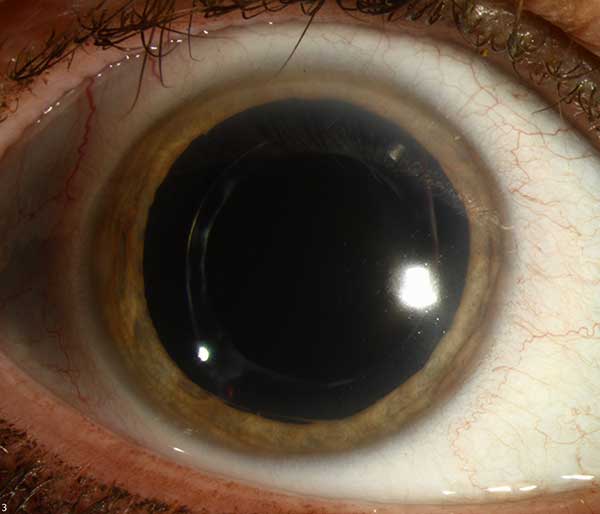
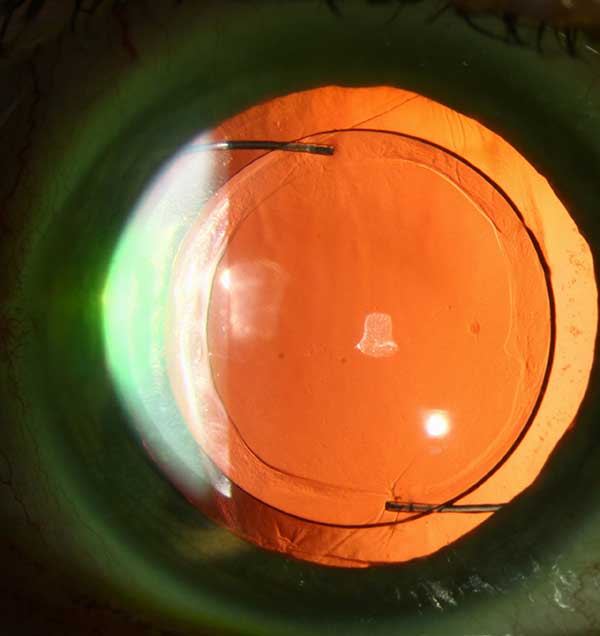
| right eye(click on either image for higher resolution image) | left eye |
 |
 |
 |
 |
OD
OS
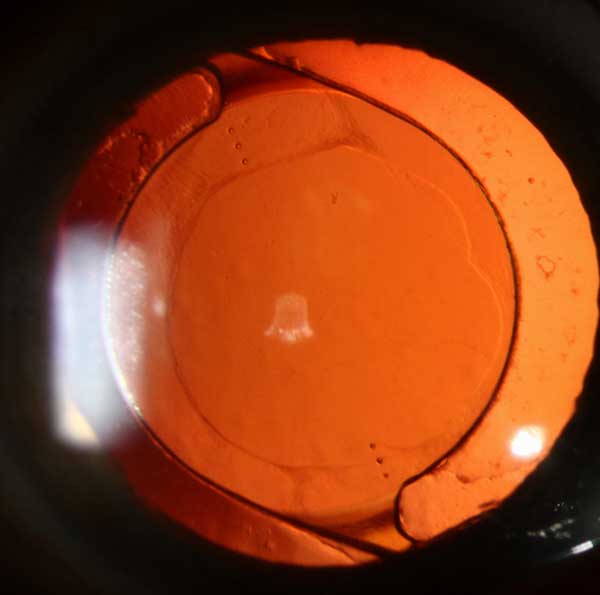
IOL calculations showed over 4 diopters of corneal astigmatism in both eyes. (See figure 2)
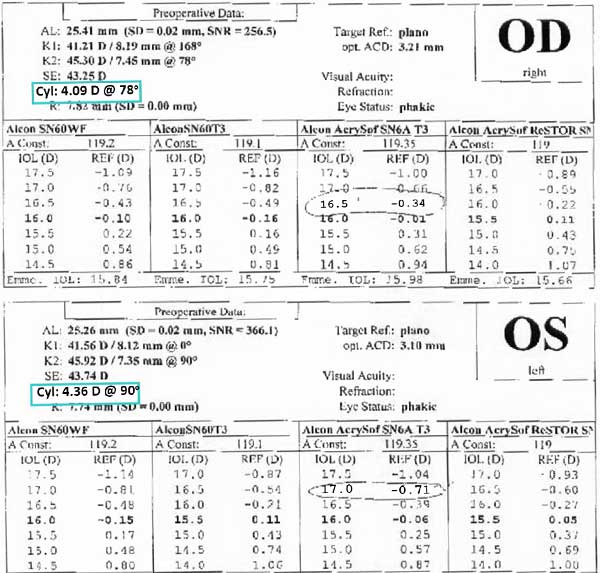 |
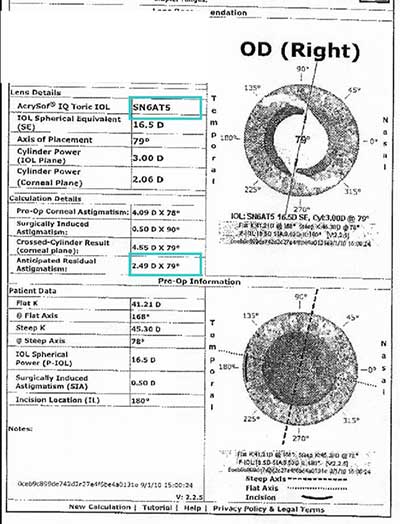
Toric lens calculations predicted that even using the highest toric power available at the time of her surgery (Alcon Acrysof SN6AT5 which corrects about 2 diopters of astigmatism at the corneal plane), there would be approximately 2.50 diopters of residual astigmatism OD and 4 diopters of residual astigmatism OS. (fig. 3) (See discussion of toric IOLs below)
| Right Eye | Left Eye |
|---|---|
 |
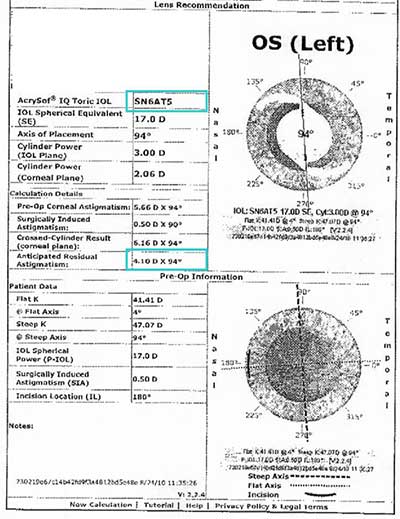 |
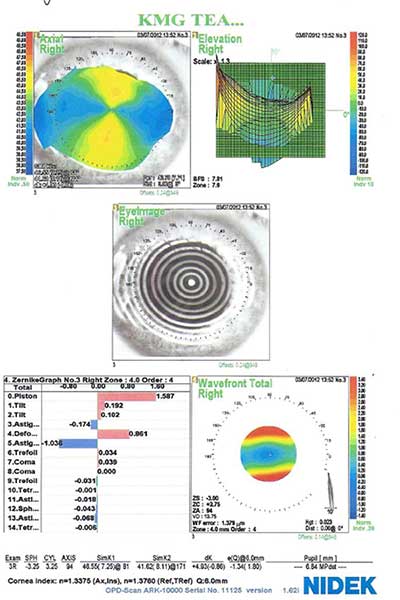
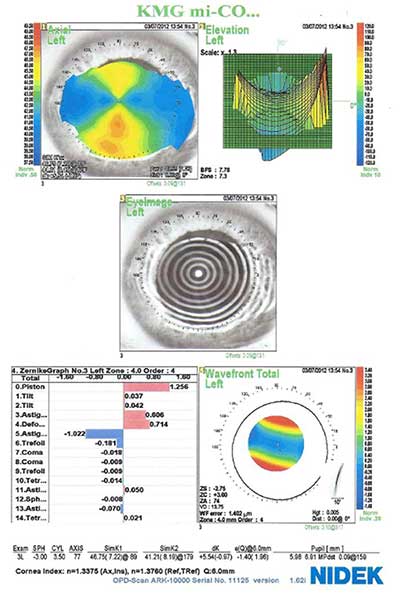
Corneal topography confirmed with-the-rule corneal astigmatism of 4.93 diopters OD and 5.54 diopters OS. (fig. 4)
| Right eye | Left Eye |
 |
 |
63 year old female with about 5 diopters of corneal astigmatism in both eyes, 2 diopters of iatrogenic lenticular astigmatism in the toric IOL, and 4 diopters of astigmatism in her manifest refraction.
Manifest refraction gave 20/20 acuity, but she could not tolerate spectacles because of image distortion from the high astigmatic correction.
She was unable to obtain optimal vision even with RGP lenses. With an RGP lens, the lens tear film corrects the corneal astigmatism, but this uncovers lenticular astigmatism. A bitoric lens can correct corneal astigmatism and some lenticular astigmatism. The toric base straddles the cornea and maintains fit while residual astigmatic correction can be placed on the front surface of the lens. Because of this patient's combination of lenticular and residual corneal astigmatism, a front surface could not be created to perfectly correct the complex refractive error. Even with a multitude of bitoric lens fittings, her best acuity was only 20/40.
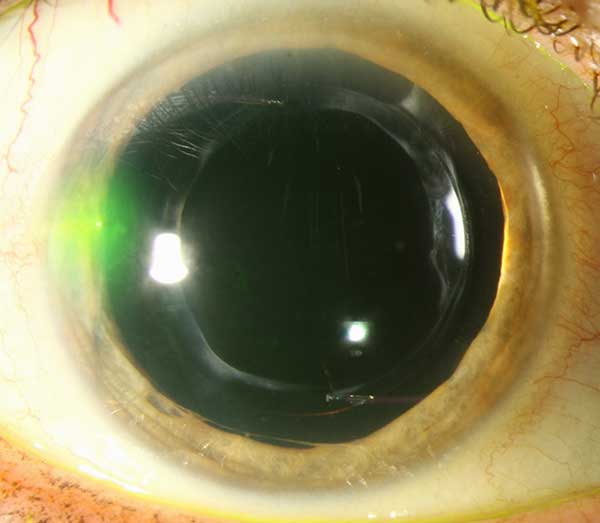
We opted to proceed with IOL exchange to remove the toric lens and place a spherical lens to remove the lenticular astigmatism and allow for correction of the corneal astigmatism with RGP lenses. (See Video 1 and 2 and post-operative photos in figure 5)
 |
 |
 |
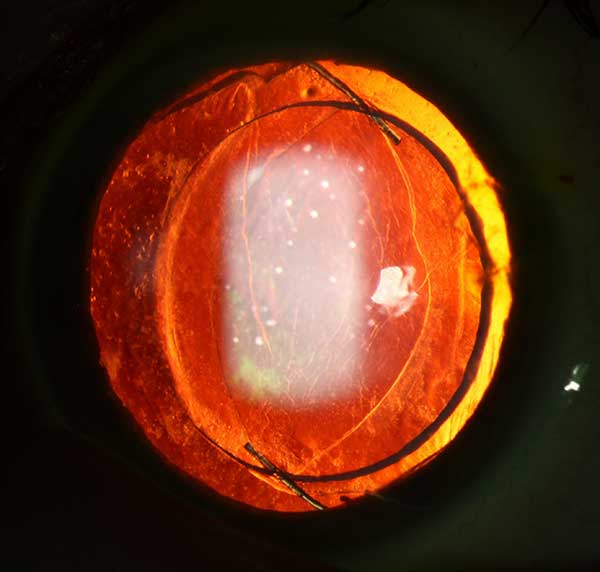 |
Video 1: Right Eye IOL exchange (if video 1 fails to load, view in external viewer)
Video 2: Left Eye IOL exchange (if video 2 fails to load, view in external viewer)
She was then re-fit with a rigid gas permeable lens in each eye with final visual acuity of 20/20 OD and 20/20 OS.
There are multiple refractive options for the treatment of high astigmatism including spectacle correction, contact lenses, laser refractive surgery, corneal or limbal relaxing incisions, astigmatic keratotomy, or toric intraocular lens implantation. This discussion will be limited to the interventions tried by our patient, spectacle correction, rigid gas permeable contact lenses, and toric lens implantation.
The least invasive treatment of astigmatism is spectacle correction. Patients have a more difficult time adapting to spectacles with high astigmatic correction, especially if the astigmatism is oblique. If patients have not been prescribed glasses with high cylinder in the past, they may experience image warping or tilting when wearing the new glasses.
Rigid gas permeable contact lenses are a second option for the correction of high astigmatism. There are multiple types of rigid gas permeable lenses available. The choice of lens type depends on the total amount of cylinder induced by the cornea and the lens (See table 2) (Cutler 2006).
Spherical surface with spherical base curve
|
Toric surface lens with spherical base curve
|
Spherical surface with toric base curve
|
Toric surface with toric base curve (bitoric)
|
Two types of bitoric lenses 1. Spherical power equivalent (SPE) bitoric
2. Cylindrical power equivalent (CPE) bitoric
|
If a patient is considered a candidate for cataract extraction, corneal astigmatism can be corrected using a toric intraocular lens. The primary purpose of a toric intraocular lens is similar to a spherical intraocular lens, to restore vision decreased by a significant cataract. The secondary purpose is to correct corneal astigmatism with the goal of maximizing uncorrected distance visual acuity. A recent systematic review supports that toric IOLs are successful in improving uncorrected acuity in patients with corneal astigmatism (Agresta et al 2012).
Our institution uses Alcon Acrysof IQ Toric lenses which are currently available in T3 through T9 powers (See table 3). The lower T3 through T5 powers were approved by the FDA in September 2005 (Acrysof 2009). The higher T6 through T9 powers were approved by the FDA later in May of 2011 (Acrysof 2011). The Acrysof toric lens calculator (http://www.acrysoftoriccalculator.com/) is helpful in determining which power lens and axis of placement to optimize post-surgical visual acuity.
Lens model |
SN6AT3 |
SN6AT4 |
SN6AT5 |
SN6AT6 |
SN6AT7 |
SN6AT8 |
SN6AT9 |
|
|---|---|---|---|---|---|---|---|---|
Cylinder power |
IOL plane |
1.50 D |
2.25 D |
3.00 D |
3.75 D |
4.50 D |
5.25 D |
6.00 D |
Corneal plane* |
1.03 D |
1.55 D |
2.06 D |
2.57 D |
3.08 D |
3.60 D |
4.11 D |
|
Recommended Corneal astigmatism correction range |
0.75 D to 1.54 D |
1.55 D to 2.05 D |
2.06 to 2.56 D |
2.57 D to 3.07 D |
3.08 D to 3.59 D |
3.60 D to 4.10 D |
4.11 D and up |
|
| * Based on the average pseudophakic human eye | ||||||||
| Table adapted from Acrysof IQ Toric (SN6ATT) Surgeon Keys for Success and Acknowledgement (2011), used with permission from Alcon Surgical, Inc., all rights reserved. | ||||||||
Careful patient selection is crucial to achieve optimal visual outcomes after toric IOL implantation. Many factors come into play when considering if a patient is a candidate for toric IOL.
If a co-existing ocular condition is likely to limit the patient's visual acuity after surgery, a toric lens may not offer additional benefit over a spherical lens.
The estimated correction of corneal astigmatism is based on placement of the lens in the capsular bag. Therefore, ideal patients are those anticipated to have a high success of continuous curvilinear capsulorhexis.
Ocular surface disease or epithelial basement membrane dystrophy can cause variable irregular astigmatism and spuriously high cylinder on IOL calculation results. A toric lens based on inaccurate calculations may result in a post-operative refractive surprise. A careful corneal exam in conjunction with corneal topography can help identify errors from irregular astigmatism.
A patient with less than 0.75 diopters of astigmatism is unlikely to have significant benefit compared with a spherical IOL. A patient with astigmatism greater than the recommended range may have their astigmatism reduced, but not fully corrected by the implant lens.
A patient that has a strong desire to be glasses-free for distance vision is a good candidate for a toric IOL. If the patient wishes to continue wearing glasses or contact lenses after surgery, a spherical lens may be a better option.
Placement of a toric lens requires additional discussion with the patient, pre-surgical planning, and physician skill in intraoperative lens positioning. Toric lens choice and placement is more complicated than that of a spherical IOL and, in many practices, is an additional charge.
Our patient is an example of the importance of careful patient selection prior to toric lens implantation. Two important factors made her a less than ideal candidate for toric lens placement.
First, she had a large amount of corneal astigmatism, larger than what could be fully corrected by the highest toric IOL power available. At the time of her cataract surgery in 2010, lens powers up to only T5 were FDA-approved. After placement of the SN6AT5 lens, she had significant residual astigmatism of 4 diopters in her postoperative manifest refraction.
Second, she stated that she was a long-term rigid gas permeable contact lens wearer and desired to continue wearing monovision RGP lenses after cataract surgery. She was not interested in wearing glasses. Pure corneal astigmatism is relatively easily corrected using RGP lenses. The placement of a toric IOL added lenticular astigmatism making her RGP lens fit much more difficult, even by an eye care provider experienced at fitting these lenses. The lenticular astigmatism showed through, no matter which contact lens was tried. The best corrected visual acuity we could obtain with contact lens correction was 20/40. With the combination of corneal and iatrogenic lenticular astigmatism, she was unable to obtain acceptable visual acuity using her preferred method of vision correction.
Thoughtful discussion with the patient and thorough preoperative planning may have identified these issues prior to surgery. Primary placement of a spherical IOL would have allowed for easy fitting of monovision RGP lenses, saving the patient the time and expense of multiple contact lens fittings and additional IOL exchange surgery.
Toric lenses are a good option for patients with corneal astigmatism who undergo cataract surgery. With the advent of higher power toric lenses, they are being used in a wider range of patients. However, not every patient with astigmatism is a candidate. Careful preoperative planning can help identify appropriate patients and increase surgical success and patient satisfaction.
Maltry A, Kitzmann AS, Sindt C. To toric or not to toric? A cautionary tale. EyeRounds.org. February 27, 2013; Available from: https://eyerounds.org/cases/164-Toric-IOL-exchange.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.