A 62-year-old woman presents with a 3-year history of painless, progressive loss of vision in both eyes.
Over the last 3 years, there has been gradual, painless loss of vision in both eyes (right greater than left) at both distance and near. She has had 3 updates of her spectacle prescription that have not provided satisfactory vision. There is no diurnal variation in vision.
Visual acuity (VA) with correction:
Manifest Refraction
Intraocular pressure (applanation): OD 16 mmHg, OS 18 mmHg
Pupils: Equal, round, 4 mm in dark, 2 mm in light, no relative afferent pupillary defect
Visual fields: Full to confrontation both eyes (OU)
Motility: Full OU
Disc: Normal, cup-to-disc ratio 0.3 OU
 |
 |
Topography was ordered to characterize the corneal nodules seen on slit lamp exam in the setting of significant astigmatism. Figure 2 shows the crab-claw like pattern of irregular astigmatism superiorly on each eye due to the superior Salzmann’s nodules. Placido images show irregular mires most noticeable superiorly on each eye corresponding to the Salzmann’s nodules.
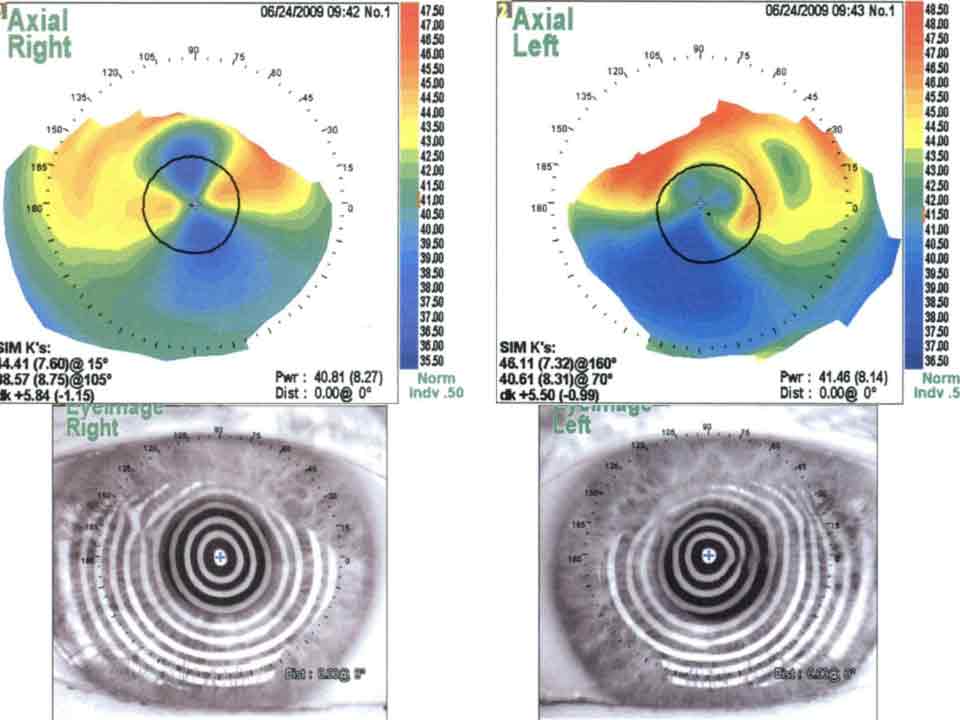
Figure 2: Topography before treatment.
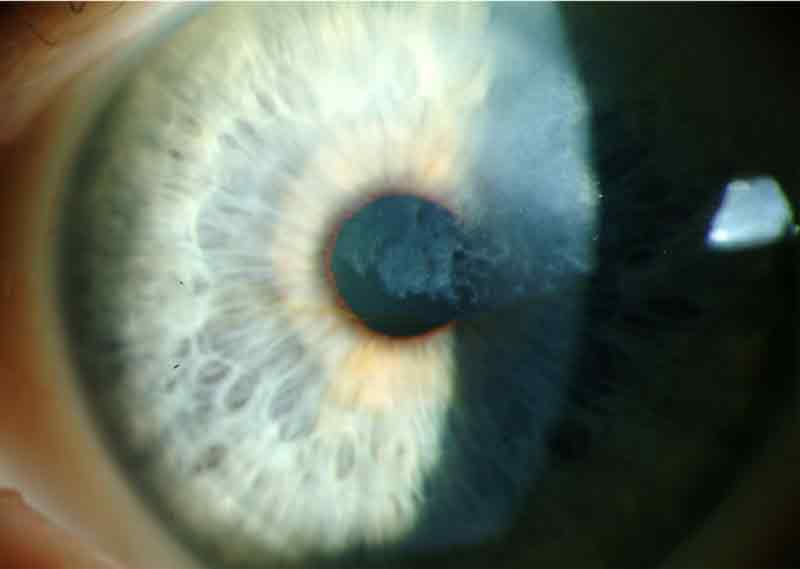
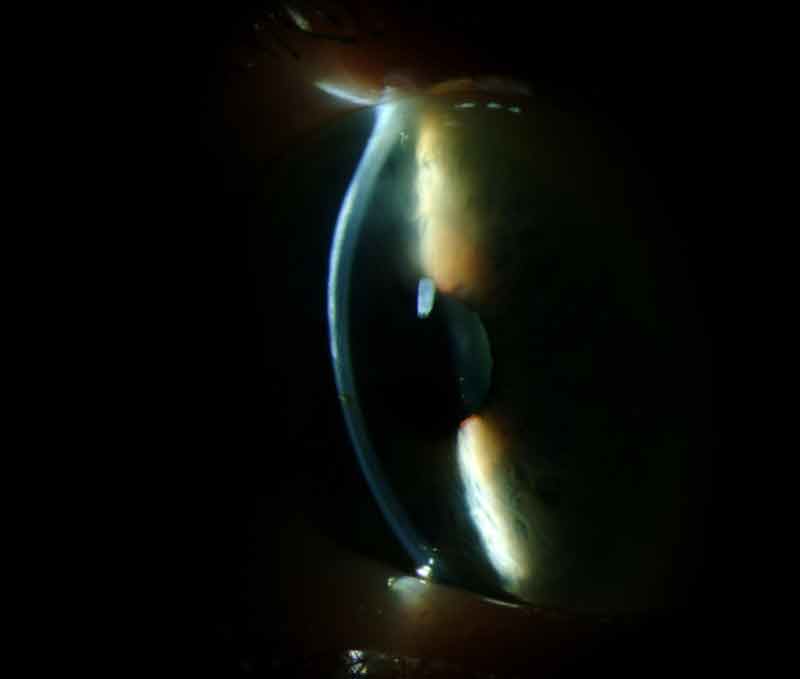
A diagnosis of Salzmann’s nodular degeneration was made on the basis of the characteristic clinical appearance and the clinical history of progressive increasing irregular astigmatism associated with worsening of best corrected visual acuity. She was also diagnosed with nuclear sclerotic cataracts on the right greater than left eye.
To improve visual acuity and to decrease the irregular astigmatism a superficial keratectomy was recommended to remove the Salzmann’s nodules.
The patient underwent superficial keratectomy on her right eye. Postoperatively, there was complete clearing of the subepithelial opacities with excellent clarity of the underlying stroma. One month later, reliable keratometry and intraocular lens (IOL) calculations were obtained and an uneventful phacoemulsification and implantation of a posterior chamber IOL was performed (see Figure 3). Several months later, she underwent superficial keratectomy on her left eye with similar results, followed by cataract surgery on her left eye one month later. Postoperatively both eyes achieved best corrected visual acuity of 20/20, with substantial reduction in the astigmatic error (Table 1; Figure 4). At the time of this writing, the vision and examination remains stable for 47 months with no recurrence of Salzmann’s nodular corneal degeneration. The mild dry eye continues to be well controlled with artificial tears.

Figure 3: Right eye slit lamp photography, after superficial keratectomy, cataract extraction and intraocular lens placement.
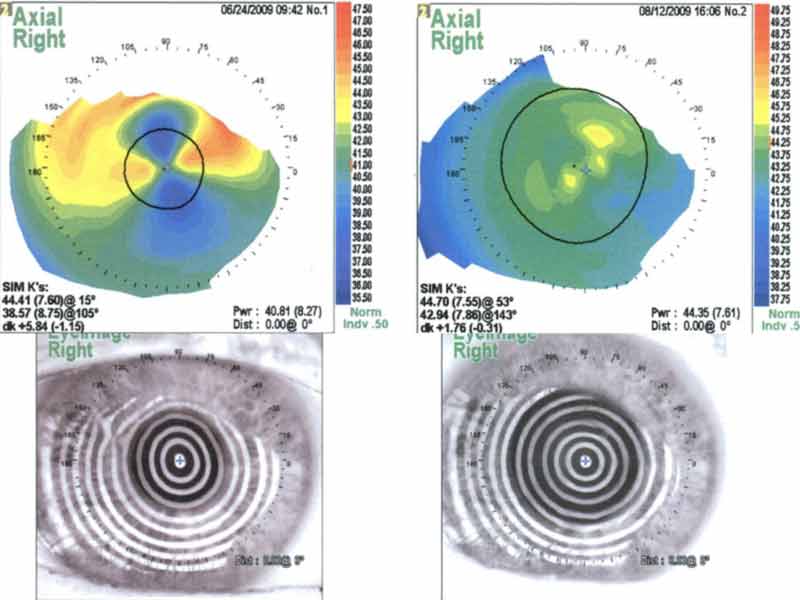
Figure 4: Right eye topography after superficial keratectomy. The overall corneal curvature is reduced with substantial reduction of both regular and irregular astigmatism.
Table 1
| Pre-operative Manifest Refraction |
-2.00 + 5.00 x 20 VA 20/60 OD -0.75 + 7.50 x 165 VA 20/25 OS |
Post-operative Manifest Refraction |
-0.25 + 0.75 x 045 VA 20/20 OD -1.00 + 1.00 x 150 VA 20/20 OS |
Salzmann’s nodules are characterized by hyaline deposited anterior to a disrupted or even displaced Bowman’s layer, posterior to an atrophic corneal epithelium. Figure 5 for is an example of the typical histopathology of Salzmann’s nodules.
Salzmann’s nodular corneal degeneration was described by Katz in 1930 following a 1925 case series on the condition published by Maximilian Salzmann, although Salzmann concedes that a case published by Ernst Fuchs in 1901 appears to be the first published case of this corneal degeneration [1].
Salzmann’s nodular corneal degeneration is characterized by bilateral gray-white elevated nodules anterior to Bowman’s layer, which may be visually significant, cause foreign body sensation, or be asymptomatic. It is most common in middle-aged women. The cause of this degeneration is unknown; however, it has been associated with chronic ocular surface inflammation [1-6]. A case series of 152 eyes concluded that the most common associations were, in descending order, meibomian gland dysfunction (MGD), contact lens wear (especially hard contact lenses), peripheral vascularization, pterygium, keratoconjunctivitis sicca, and exposure keratitis [1]. Another case series of 180 eyes also identified MGD as the most common comorbidity [2].
Conservative treatment consists of management of the underlying etiology, such as MGD. Eyelid hygiene and doxycycline may be considered to treat the MGD prior to surgical treatment. Contact lens cessation or re-fitting may also be beneficial. Medical management is successful in preventing the need for surgery in most cases; the indications for surgery are (1) discomfort; (2) reduced vision due to progressive increase in astigmatic error. Surgery is uniformly successful in removal of the nodule and almost invariably successful in reducing the astigmatic error in allowing for improvement in best corrected visual acuity, usually with a much weaker spectacle prescription. Stabilization of the refractive error usually takes 3 to 6 weeks. In rare cases of neglected nodules within the visual axis, anterior stromal haze may compromise the final visual results.
Whereas subtle recurrences are common in most cases over a 5 to 15 year period, visually significant recurrences are uncommon (5 to 20%) and can be minimized with meticulous control of the etiology responsible for the condition [1, 2]. Those cases can be treated with repeat superficial keratectomy. If anterior stromal haze persists in the visual axis after treatment of primary or recurrent nodules, phototherapeutic keratectomy can be offered [1].
Superficial keratectomy of astigmatism-inducing Salzmann’s nodules should always be performed prior to cataract surgery. Stable keratometry readings and IOL calculations cannot be reliably obtained until 3 to 6 weeks after surgery. Toric IOLs should be avoided because of the risk of recurrent nodules and induction of post-operative astigmatism.
Since the diagnosis of Salzmann’s nodular corneal degeneration is clinical, several more examples appear in figures 6-10.

Figure 9: Slit lamp photo of the right eye of another patient with Salzmann’s Nodular Corneal Degeneration. Nodules are nasal and inferonasal.
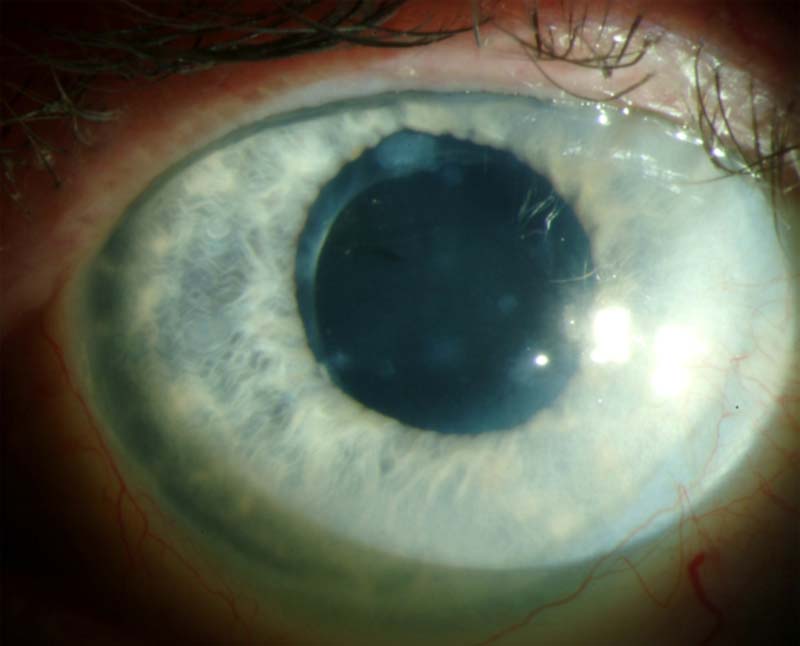
Figure 10: Slit lamp photo of another patient with Salzmann’s Nodular Corneal Degeneration. Several small nodules, superior and inferior approach the visual axis.
For a summary of the key facts regarding Salzmann’s nodular corneal degeneration, see Table 2.
Table 2
Epidemiology
|
Signs
Symptoms
|
Diagnosis
|
Treatment
|
Salzmann’s nodular corneal degeneration is a non-inflammatory, slowly progressive nodular corneal degeneration that may induce ocular surface discomfort and progressive astigmatism with decreased best corrected visual acuity. The diagnosis is based on clinical examination. Topography is helpful in evaluating the contribution of the nodule to visual impairment. Superficial keratectomy is a successful treatment option, and visually significant recurrence afterward is relatively rare.
Carroll JN, Maltry AC, Kitzmann AS. Salzmann’s Nodular Corneal Degeneration: 62-year-old woman presents with 3 years of progressive decrease in vision. EyeRounds.org. September 9, 2013; available from https://eyerounds.org/cases/180-salzmann-nodular-corneal-degeneration.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.