Chief complaint: Decreased vision and a central scotoma in both eyes (OU)
History of Present Illness: The patient is a 43-year-old male who presented with decreased vision and a central scotoma OU for the past 10 years, which has been getting progressively worse. He describes the vision as having a blurred spot in central of his vision bilaterally. The patient saw an optometrist two years ago and could not be refracted better than 20/40 in either eye. The patient has had intermittent photopsias in both eyes over the past two years. He denies floaters.
Past Ocular History: None
Past Medical History: Depression
Medications: sertraline, fish oil
Allergies: None
Family History: Non-contributory
Social History: The patient works as a chef. He does not smoke or drink alcohol.
Review of systems: All negative except for HPI
Pupils: 5→3, no RAPD OU
Extraocular movements: Full OU
Confrontation visual fields: Full OU
Intra-ocular pressure:
Slit Lamp Exam
The optic nerves have a cup-to-disc ratio of 0.2 OU. The macula of both eyes have a greyish sheen with superficial crystals, right angle venules, and telangiectatic vessels that are more prominent temporally. The vessels and peripheral retina are normal OU. There is no posterior vitreous detachment (Figure 1).
Fundus photos demonstrate a greyish sheen with superficial crystals, right angle venules, and telangiectatic vessels that are more prominent temporally in the macula of both the right (A) and left (B) eyes (Figure 1).
Fluorescein angiography (FA) demonstrates telangiectatic vessels surrounding the fovea more prominent temporally with leakage OU (Figure 2).
Spectral domain optical coherence tomography (OCT) demonstrates small foveal cystoid cavities in both the right (A) and left (B) eyes. The central macular thickness is 331 microns OD and 320 microns OS (Figure 3).
Autofluorescence imaging shows a mild increase in autofluorescence in the foveal region of both the right (A) and left (B) eyes (Figure 4).
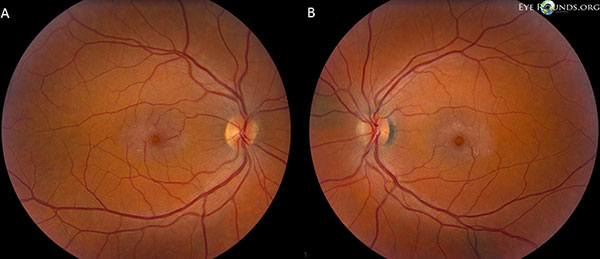
Figure 1. Fundus photos demonstrate a greyish sheen with superficial crystals, right angle venules, and telangiectatic vessels that are more prominent temporally in the macula of both the right (A) and left (B) eyes.
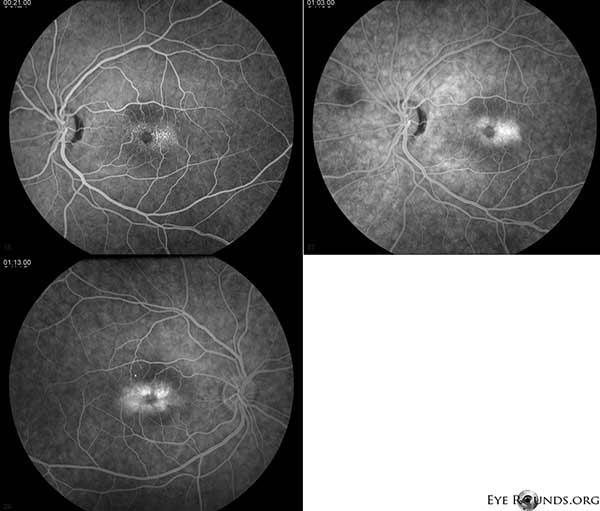
Figure 2. Fluorescein angiography demonstrates telangiectatic vessels surrounding the fovea more prominent temporally with leakage OU.
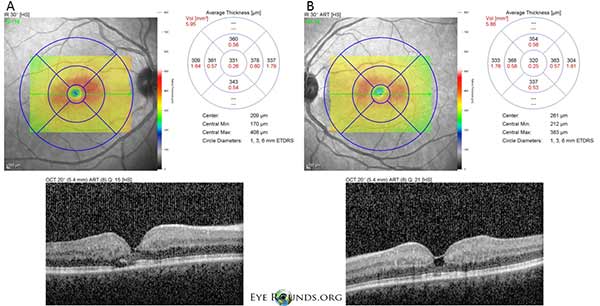
Figure 3: Spectral domain optical coherence tomography (OCT) demonstrates small foveal cystoid cavities in both the right (A) and left (B) eyes. The central macular thickness is 331 μm OD and 320 μm OS.
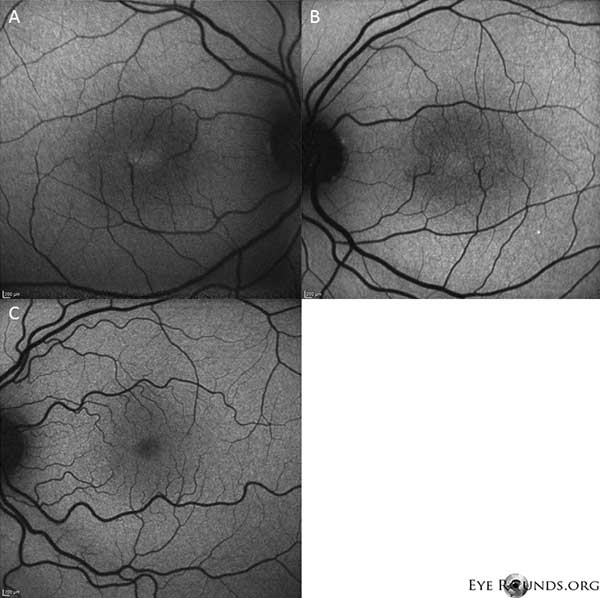
Figure 4: Autofluorescence imaging shows an increase in autofluorescence in the foveal region of both the right (A) and left (B) eyes. An eye with normal autofluorescence is shown forcomparison (C).
Idiopathic Juxtafoveal telangiectasia, type II (Macular Telangiectasia type 2 or Mac Tel 2)
Idiopathic juxtafoveal telangiectasia (IJFT), also known as idiopathic macular telangiectasia[1], is an uncommon disorder characterized by telangiectatic vessels in the juxtafoveolar region of one or both eyes. According to Gass, IJFT can be divided into three groups based upon phenotype:[2] type I is typically a unilateral disease characterized by parafoveal dilation of capillaries, microaneurysms, leakage, and lipid deposition; type II is the most common form of IJFT and typically presents with bilateral juxtafoveal telangiectasias with minimal exudate; type III is extremely rare and is characterized by occlusive telangiectasia. This review will focus on IJFT type II (macular telangiectasia type 2 or Mac Tel 2).
The prevalence of IJFT type II is not entirely known, but one large study estimated a prevalence of 1-5 in 22,062 while another study estimated it may be has high as 0.1% in some populations.[3 ,4] Although IJFT can occur at any age, the mean age of onset is 55 years old. There is no predilection for gender and no known racial predilection. Although there are a few case reports of monozygotic twins with IJFT type II raising the possibility of genetic component, there is currently insufficient evidence from population studies to support genetic association. Several studies suggest that smoking may worsen disease.
IJFT type II is a bilateral disease, but can be asymmetric and may appear as a unilateral process early in the disease. Patients often present with complaints of blurred vision, metamorphopsia, or paracentral scotomas.
Early changes seen with IJFT type II include parafoveal graying of the retina, superficial crystalline deposits, subfoveal cystoid cavities, parafoveal telangiectasias, and right-angle vessels. Visual acuity decreases slowly and is often associated with hyperplasia of the retinal pigment epithelium (RPE). In approximately one-third of patients, deep retinal neovascularization with retinal feeders, subretinal neovascularization (SRNV), may occur as an acute complication and is then called the proliferative form.[1 ,5] The natural progression of the disease results in significant visual loss in the majority of patients with IJFT type II.[5] In a paper by Watzke et al., 15 or 20 eyes developed either central RPE hyperplasia or SRNV with decreased vision of 20/70 or worse over 15 years.[5]
Fundus findings of IJFT type II on biomicroscopy can be subtle, especially early in the disease process, and therefore imaging with FA, OCT, and fundus autofluorescence are important in making the diagnosis. FA highlights the parafoveal telangiectatic vessels, which demonstrate early hyperfluorescence with leakage. These are often more prominent temporal to the fovea. OCT demonstrates subfoveal cystoid spaces, usually without cystoid macular edema.[6 ,7] In more advanced disease, photoreceptor disruption and outer retinal atrophy are present on OCT.[7] Fundus autofluorescence findings are pathognenmonic for MacTel II, showing a loss of the physiologic hypoautofluorescence—i.e. increased autofluorescence—in the fovea.[8 ,9]
The pathogenesis of IJFT type II is unclear, but may involve abnormalities in the parafoveolar Muller cells rather than a primary abnormality of retinal capillaries.[10] Muller cells are important for the health of the retinal capillary endothelium and the surrounding retina.[11 ,12] It has been postulated that Muller cell dysfunction in IJFT type II results in endothelial degeneration, which may lead to retinal capillary proliferation and telangiectasia.[6 ,7] In support of this, perifoveal depletion of Muller cells has been seen on histopathology of patients with IJFT type II.[13] The superficial crystals seen in patients with IJFT type II are thought to represent to footplates of degenerated Muller cells.[7 ,14] In addition, it has been speculated that the spaces seen on OCT in IJFT type II represent tissue loss from retinal degeneration, specifically due to the dysfunction or loss of Muller cells, rather than fluid filled cystic spaces.[1,12,13]
A better understanding of the disease mechanism in IJFT type II is important because there remains no definitive treatment for the visual loss seen in the nonproliferative form of IJFT II. Bevacizumab has been shown to be effective in the treatment of the SRNV associated with IJFT type II, but does not appear to consistently affect the course or cystic changes in nonproliferative IJFT.[15-19] Similarly, ranibizumab failed to show a functional benefit in a prospective interventional trial of patients with nonproliferative IJFT type II, although was shown to cause a significant reduction in retinal thickness and a decrease in leakage on FA.[20] Oral carbonic anhydrase inhibitors were also shown to cause a significant reduction in retinal thickness, but did not significantly improve visual acuity.[21] Multiple other interventions have been tried, including focal grid laser,[22] photodynamic therapy,[23] and intravitreal triamcinolone,[24] with no clear improvement in either the cystoid cavities or the visual acuity in patients with IJFT type II. Finding an effective treatment is important because the majority of patients with IJFT type II develop a significant decline in vision over time.
Our patient highlights all of the early findings of non-proliferative IJFT type II, including parafoveal graying of the retina, superficial crystalline retinal deposits, right angle vessels, and parafoveal telangiectasias (Figure 1). FA further highlighted the parafoveal telangiectasias, which demonstrated prominent leakage and staining of the retina (Figure 2). OCT demonstrated characteristic subfoveal cystoid spaces (Figure 3). Finally, fundus autofluorescence showed a mild increase in foveal autofluorescence consistent with IJFT type II (Figure 4). Fortunately, our patient did not show signs of more advanced disease, including no evidence of retinal pigment epithelium hyperplasia or SRNV. The patient was initially started on PO methazolamide 50mg bid and demonstrated a decrease in macular thickness within 1.5 months of treatment (Figure 5). He was then changed to PO acetazolamide secondary to insurance and had a continued decrease in macular thickness and subfoveal cysts over the next year despite only tolerating 125mg bid (Figure 5). There was also a mild non-significant improvement in visual acuity to 20/50 OD and 20/40 OS at the most recent follow-up.
Figure 5: Spectral domain optical coherence tomography (OCT) demonstrates subfoveal cyst-like spaces OU at baseline. The retinal thickness map is shown to the right (CMT = 331 μm OD, CMT = 320 μm OS). After 1.5 months of methazolamide, there was a reduction in the macular thickness (CMT = 312 μm OD, CMT = 296 μm OS). After one year of treatment with acetazolamide, there was a further decrease in the cystic spaces and macular thickness (CMT = 303 μm OD, CMT = 278 μm OS). Images were obtained in the same meridian and registered to the original visit.
Table: Characteristics of the three types of idiopathic juxtafoveolar telangiectasia
| Types of IJFT* | Epidemiology |
Signs and symptoms |
Treatment |
Prognosis |
IJFT type I |
Predominantly male. Mean age 40yo. |
Unilateral prominent visible telangiectatic retinal capillaries with macular edema and lipid deposition/exudate. |
Laser photocoagulation may reduce exudation and stabilize vision. |
Variable, majority progress to 20/70 or worse if untreated |
IJFT type II |
Equal gender predilection. Mean age 55yo. |
Bilateral parafoveal graying of the retina, superficial crystalline deposits, subfoveal cystoid cavities, parafoveal telangiectasias (more evident on FA), right-angle vessels, hyperplasia of the RPE. SRNV develops in approximately 1/3 of patients. |
No known treatment for non-proliferative IJFT type II. Intravitreal anti-VEGF for SRNV. |
Variable, 2/3 of eyes will progress to 20/70 or worse associated with RPE hyperplasia or SRNV. |
IJFT type III |
Very rare |
Bilateral perifoveal capillary obliteration, capillary telangiectasia, and minimal exudation, associated with systemic or cerebral disease. |
Unknown due to its rarity |
Variable, mostly unknown due to its rarity |
| *Idiopathic juxtafoveal telangiectasia (IJFT) is also known as idiopathic macular telangiectasia. According to the idiopathic macular telangiectasia classification, IJFT type I is named aneurysmal telangiectasia and IJFT type II is named perifoveal telangiectasia. Because of its rarity, IJFT type III has been omitted from the idiopathic macular telangiectasia classification.[1] | ||||
Epidemiology (IJFT type II)
|
Symptoms
|
Signs
|
Treatment
|
Chen JJ, Sohn EH, Folk JC, Mahajan VB, Kay CN, Boldt HC, Russell SR. Decreased Macular Thickness in Nonproliferative Macular Telangiectasia Type 2 with Oral Carbonic Anhydrase Inhibitors. Retina 2014;34(7):1400-6.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.