Elevated intraocular pressure (IOP) left eye
A 20-year-old female was referred for management of secondary open-angle glaucoma. She was initially seen three years prior by the retina service and was found to have an unusual vasoproliferative tumor in her left eye (OS). She subsequently developed posterior uveitis, which was thought to be related to leakage from this tumor. This was initially successfully treated with topical prednisolone and oral prednisone, but recurred and was subsequently treated with photodynamic therapy to the lesion as well as intravitreal Triesence® (triamcinolone acetonide). Shortly thereafter, her IOP spiked to 59 mm Hg. She was started on topical dorzolamide-timolol, brimonidine, latanoprost and oral acetazolamide and referred to the glaucoma service. At that time, she reported ocular irritation with drop therapy, along with systemic malaise and stomach upset from oral acetazolamide.
Past Medical History: None
Past Surgical History: None
Allergies: None
Family History: No family history of glaucoma
Social History: Non-contributory
Review of Systems: Negative except as listed in HPI
Ocular Motility: Full both eyes (OU)
Confrontation visual fields: Full to counting fingers OU
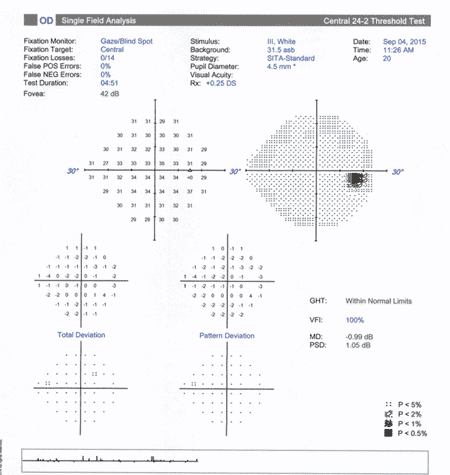
OD
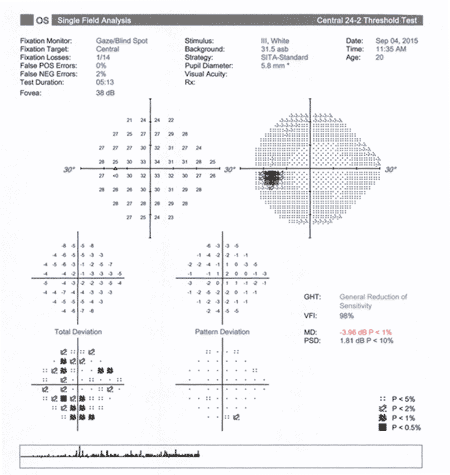
OS
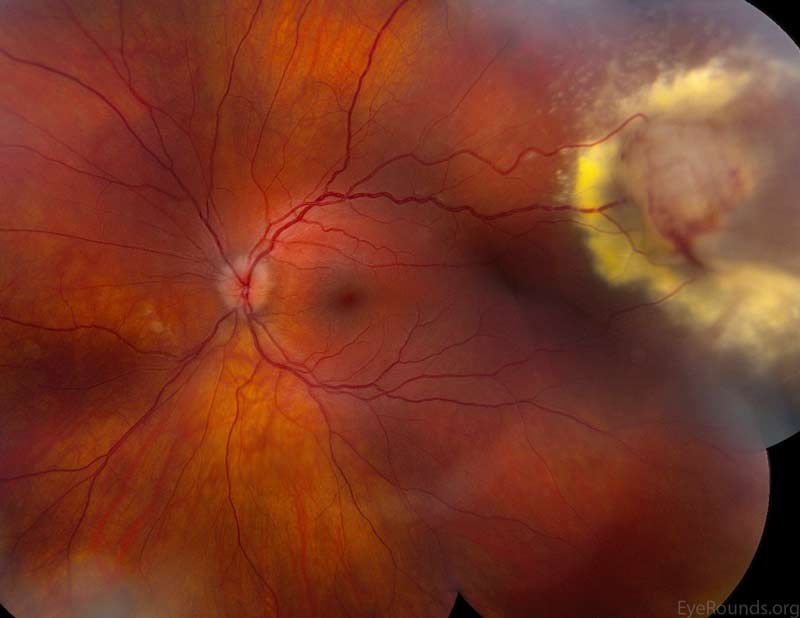
Figure 1. Left eye: Normal macula and vessels. Yellow-white vascular mass in the superotemporal periphery with surface telangiectasia and a feeding arteriole.
 |
 |
| Right Eye | Left Eye |
|---|
Given the relatively healthy appearance of the optic nerve and normal visual fields, along with the temporal association of the IOP spike with the steroid injection, the initial decision was to temporize the IOP medically until 6-8 weeks following the injection before undertaking glaucoma surgery. Even so, the pressure remained elevated and the patient became increasingly intolerant of both topical and oral anti-glaucoma medications. As such, the patient elected to proceed with surgery. With the relatively recent inflammation, the patient was deemed high-risk for trabeculectomy failure and offered tube shunt implantation or gonioscopy-assisted transluminal trabeculotomy (GATT). Given her age and the potential need for future intervention, the patient opted for GATT as a minimally-invasive glaucoma surgery (MIGS) for first-line treatment. The narrated recording of this surgery can be seen in Video 1.
Video 1: Gonioscopy-assisted transluminal trabeculotomy (to read the transcript of this video, please see the video atlas page)
|
Visual Acuity |
Visual Acuity Pin hole |
IOP |
Anti-Glaucoma Medications |
|---|---|---|---|---|
Pre Operative |
20/25 |
20/20 |
32 |
Dorzolamide-timolol Brimonidine Travoprost Oral acetazolamide |
Day 1 |
20/30-2 |
20/25-1 |
10 |
None |
Week 1 |
20/25+1 |
20/25 +2 |
15 |
Pilocarpine |
Week 2 |
20/30+2 |
20/25+2 |
13 |
Pilocarpine |
Week 6 |
20/30 |
20/25+1 |
14 |
None |
Table 1: This table outlines the visual acuity and IOP of the post-operative visits. On post-operative day 1, there was 3+ RBCs and a small (<1mm) hyphema which resolved by post-operative week 1.
Increasing attention has been given to the surgical treatment of glaucoma given the morbidity associated with traditional glaucoma surgery. In the trabeculectomy versus tube study (TVT), there was found to be early post-operative complications in 37% of trabeculectomy patients and 21% of tube shunt patients, along with late complications in 36% and 34%, respectively (1). These observations have led to an increasing focus on angle surgery and other minimally-invasive glaucoma surgeries, including trabectome, iStent, canaloplasty, and the recently-described ab interno trabeculotomy (2, 3). All of these approaches share the common goal of increasing the natural flow of aqueous into Schlemm's canal. GATT is a minimally-invasive form of ab interno trabeculotomy first described by Grover et al. (4). It can be performed using a small suture or illuminated microcatheter after a small, 1-2 clock-hour goniotomy incision is made using a direct gonioprism. After Schlemm's canal is cannulated, a 360 degree trabeculotomy is performed (Video 1). One major advantage of this approach is that it spares the conjunctiva, which could later be used for trabeculectomy or tube shunt surgery if needed. Amongst MIGS in the US, another advantage of this technique is that it does not need to be combined with cataract surgery and can be performed as a standalone procedure. In some countries, 360 degree trabeculotomy has become a first-line option for the treatment of glaucoma (5).
|
POAG (n=57) |
Other Glaucoma (n=28) |
|||
|---|---|---|---|---|---|
|
GATT only (n=25) |
GATT + CE/IOL (n=16) |
GATT + prior CE/IOL (n=16) |
GATT only (n=17) |
GATT + CE/IOL (n=11) |
Pre-op IOP (mmHg) |
25.6 |
23.9 |
23.8 |
31.8 |
27.6 |
1 yr IOP (mmHg) |
15.7 |
15.5 |
16.2 |
12.4 |
13.8 |
# of medications pre-op |
3.2 |
2.9 |
2.2 |
3.5 |
2.9 |
# of medications at one year |
1.5 |
1.0 |
2.6 |
1.8 |
1.2 |
Table 2: This table summarizes the findings described in detail below. [adapted from Grover et al. (4)]. POAG = primary open-angle glaucoma, CE/IOL = cataract extraction with intraocular lens placement.
This retrospective chart review examined 85 patients who underwent GATT surgery. Fifty-seven patients with POAG had an average decrease of 11.1 mmHg (39.8%) with 1.1 fewer glaucoma medications used at one year. In the secondary glaucoma group of 28 patients, intraocular pressure decreased by an average of 19.9 mmHg (56.8%) with 1.9 fewer medications being used at one year. Eight patients (9.4%) required further IOP-lowering surgery within 1 year to achieve adequate IOP control. Serious complications were rare, but transient hyphema was seen in 30% of patients. Other rare complications included cystoid macular edema, choroidal folds and steroid-induced elevation of IOP. Concurrent cataract surgery was not deemed to have any statistically significant impact on the data analysis. These results are similar to other reports of ab externo trabeculotomy (5, 6, 7). More recently, this technique has also been reported in primary congenital glaucoma and juvenile open-angle glaucoma with an average decrease from 27.3 to 14.8 mmHg, as well as a significant reduction in medication use (8).
Absolute contraindications proposed by Grover et al. are the inability to stop anticoagulants, bleeding diatheses, an unstable intraocular lens, inability to identify angle structures, a closed angle, or severe corneal endothelial compromise. Relative contraindications are prior corneal transplantation or inability to elevate the head 30 degrees for the first 1-2 weeks after surgery.
As seen in our video (Video 1), the procedure is made easier by the use of a flexible illuminated microcatheter, although one may also use a small nylon or prolene suture to cannulate Schlemm's canal. One feature to look for during the operation is episcleral venous blanching during the irrigation and aspiration portion of the procedure, which indicates an open collector channel system (9). Although taken from a different patient, this is demonstrated well in (Video 2). Another feature of a successful surgery is creation of a "trabecular shelf," in which the reflected trabecular meshwork is adherent to the peripheral iris (4). This can usually be seen gonioscopically after the surgery has healed.
Video 2. Episcleral Blanching
This case represents the use of an angle-based glaucoma surgery for the treatment of a 20-year-old patient with secondary open-angle glaucoma. Her results support the effectiveness and relative safety of this therapy. GATT provides the advantage of sparing the conjunctiva for potential future interventions while opening access to Schlemm's canal for 360 degrees.
Secondary open-angle glaucoma successfully treated with GATT
Indications
|
Contraindications
|
Complications
|
Efficacy [4]
|
Lenci LT, Bettis DI. Secondary Open-Angle Glaucoma Treated with Gonioscopy-Assisted Transluminal Trabeculotomy (GATT). EyeRounds.org. January 24, 2016; Available from: https://eyerounds.org/cases/231-GATT.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.