Slow decline in vision over 2 years
57-year-old Caucasian female with known history of heterozygous Fabry disease diagnosed in 2005, initially presented asymptomatically at the age of 46 with bilateral corneal verticillata, early cataracts, and vascular tortuosity. Her primary care provider noted that she had a history of numbness and tingling of her hands and feet that resolved in early adulthood, proteinuria, hypertension, and asymptomatic left ventricular hypertrophy. She subsequently was lost to follow up with ophthalmology until 2017 when she presented with increasing blurry vision with reading and distance over the past 2 years. The patient reports that her last eye exam was 7 years ago and has been wearing the same prescription since.
No other ocular history
None
Father passed away from renal failure secondary to Fabry disease
Non-contributory
Normal and full
Full
Normal
The increase in blurry vision that was attributed to progression of her cataracts. The patient's BCVA was 20/20 OU with manifest refraction and the decision was made to observe her cataracts. She was provided a prescription for new glasses and recommended follow up in 1 year with continued follow up with her primary care provider, nephrology, and cardiology as scheduled.
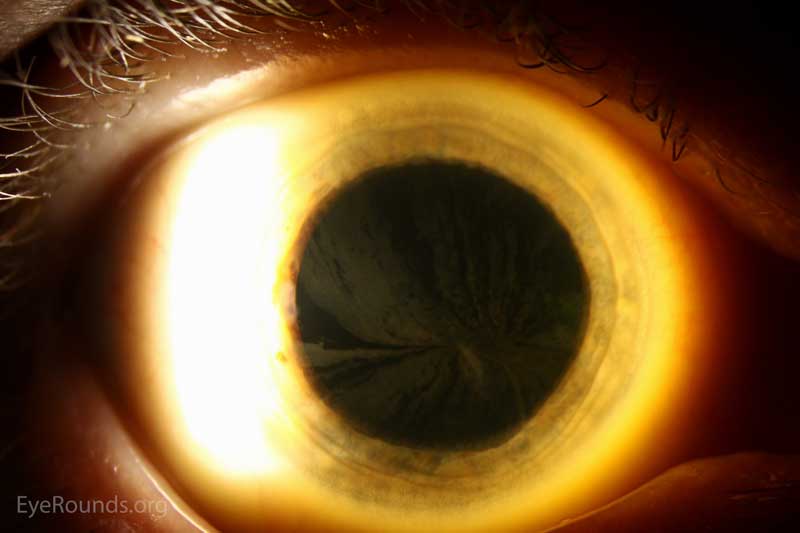 |
Figure 1: Slit lamp photos of the right eye exhibiting the whorled pattern of corneal verticillata
 |
Figure 2: Slit lamp photos of the left eye exhibiting the whorled pattern of corneal verticillata
Fabry disease is an X-linked dominant condition that affects 1 in 40,000 to 60,000 males. The prevalence in females is unknown. [1] Fabry disease results from mutations in the GLA gene encoding alpha-galactosidase A. The inability to metabolize glycosphingolipids causes a buildup in globotriaosylceramide in the cells found in nerves, vasculature, and other tissues including the cornea. This is a systemic disease that commonly presents as numbness and tingling of the hands and feet (acroparesthesias), skin lesions (angiokeratomas), decreased sweating (hypohidrosis), gastrointestinal dysfunction, kidney dysfunction, heart disease, vascular disease, and the following ophthalmic findings: corneal verticillata and vascular tortuosity. [2]
Corneal verticillata was first reported by Gruber in 1946 but it was not until 1969 when verticillata was attributed to Fabry disease by Franceschetti et al. [3,4] Corneal verticillata are also associated with many medications that cause subepithelial deposits and rarely cause visual disturbances. The following medications have been associated with corneal verticillata: amiodarone, chloroquine, hydrochloroquine, indomethacin, and phenothiazines. These often present bilaterally and will typically resolve following cessation of these medications.[5]
Diagnosis in males in the setting of positive signs, symptoms, and family history can be completed by measuring the level of alpha-Gal A activity in leukocytes or plasma. Affected males will often have little to no detectable levels of alpha-Gal A. However, atypical presentations or marginal levels of alpha-Gal A in both males and females may require genetic testing to confirm the diagnosis. Genetic testing is not necessary in females with a positive history of Fabry disease in her father, thus making females obligate heterozygotes (as is the case with our patient).[6] Treatment of Fabry disease with enzyme replacement therapy (agalsidase beta) should be started as soon as low levels of alpha-Gal A are detected, even in the absence of systemic symptoms. These patients should be followed by ophthalmology, nephrology, cardiology, neurology, and dermatology due to systemic manifestations of the disease.[7]
EPIDEMIOLOGY / ETIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT/MANAGEMENT
|
Chung AT, Oetting TA. Fabry disease. EyeRounds.org. June 15, 2017. Available from https://eyerounds.org/cases/253-Fabry-Disease.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.