Chief Complaint: 9-year-old girl presents to an outside hospital with fatigue, poor appetite, and decreased activity for 3 weeks.
History of Present Illness: Patient initially had noted mild to moderate, diffuse, intermittent headache. She developed a brief, diffuse rash that resolved spontaneously. Incidentally, the parents noted recent mosquito bites. Vitals and physical exam were unremarkable. By the time of ER presentation locally, the rash had completely resolved. ER work-up revealed CBC: 18.5 WBC; 76 % PMN, West Nile, Lyme, Monospot, and LFT’s all normal.
One week later the patient noted decreased vision in OD and for about 2 days she noticed pain in and behind the right eye. As this persisted, the patient was brought again to a local hospital. Headaches remained unchanged, though the patient did vomit once before presentation to the local hospital. The fundus was examined and an MRI of the head and orbits was obtained. Findings were concerning and the patient was transferred to the University of Iowa.
Past Medical History/Past Ocular History: None
Social History: Patient lives in an Iowa Amish community
Family History: Some history of cardiac disease; 10 healthy siblings
Medications/Allergies: none
ROS: Negative, except as noted above
Ocular Exam:
 |
 |
| 1A: Optic nerve photo, OD. Note grade 2 papilledema, characterized by 360 degree nerve elevation without obscuration of the vessels. | 1B: Optic nerve photo, OS. Note grade 1 papilledema, characterized by optic nerve elevation with temporal sparing. |
Remainder of Physical Exam: Normal vitals, skin, and HENT exam. Normal CV, lungs, GI, and GU exam.
Neuro Exam: +RAPD, OD, as noted. Remainder of CN2-12 intact. Strength, sensation, reflexes and gait all normal.
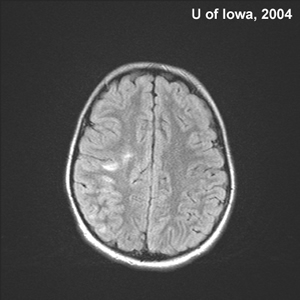
Imaging: Outside MRI revealed several non-specific white matter lesions, and possible optic nerve enhancement (lack of fat suppression in this MRI made orbital evaluation difficult).
Lumbar Puncture: Normal opening pressure, Protein = 21, Glucose = 28, WBC = 53 (15 PMN's, 31 Lymph)
Course of Management: The patient appeared to have optic neuritis (OD>OS), possibly secondary to Acute Demyelinating Encephalomyelitis (ADEM). She was admitted for a three day course of IV methylprednisolone sodium succinate (Solu-Medrol), then converting to oral Prednisone to complete a total of 14 days of steroid therapy. Within a week, her vision had returned to 20/20, OD and OS.
Four days after the completing his 14 day steroid course, however, the patient returned. She reported reduced vision OD, "worse than before". Again, there was pain behind the right eye, mild periorbital edema on that side, and right-sided jaw pain and very mild swelling. Parents noted she had "felt warm" x1day.
Repeat Lumbar Puncture: Normal opening pressure, Protein = 29, Glucose = 127, WBC = 22 (4 PMN's, 14Lymph), no oligoclonal bands seen.
Repeat MRI was performed (to confirm probable ADEM, r/o orbital or preorbital cellulitis in light of fever and recent suspected sinus infection, evaluate sinuses):
| Figure 3: MRI brain, axial FLAIR image. Note the increased signal in the white matter, evident especially at the gray/white junction. Deep white matter, including the periventricular areas, were free of signal. | Figure 4: MRI brain, sagital FLAIR image. Again, note the increased signal in the superficial white matter. |
 |
 |
| Figure 5: MRI brain, coronal T1 post-gadolinium. Increased signal is evident in the right optic nerve. | Figure 6: MRI brain, axial T1 post-gadolinium. Again, the enhancing right optic nerve is evident. |
 |
 |
The patient was felt to have a relapse of her optic neuritis secondary to ADEM. This did not seem to be a true recurrent demyelinating event, but rather a relapse of ADEM following a moderate course of steroids. The MRI did not reveal orbital or periorbital cellulitis. Neither was there any evidence of sinus disease.
Course of Management: Patient was admitted for IV Solumedrol, Acyclovir was given to cover potential HSV/VZV. The patient's vision improved to count fingers at 4 feet within 24 hours of initiating IV steroid therapy. The patient was later discharged to home on a 4 week course of oral steroid therapy.
55% of cases are bilateral. In adults, only 30% are bilateral. 87% of cases show optic disc swelling. In adults, the optic disc usually appears normal. Optic neuritis in children often follows a viral prodrome.
Optic neuritis in children is typically treated with steroids. However, controlled data supporting this is lacking. There is no pediatric equivalent to the Optic Neuritis Treatment Trial (ONTT). Prognosis is favorable, with 75% of children achieving
20/40 or better vision by 1 year. When children are taken as a whole, this is similar to data in adults. However, children under 7 years of age have better outcome than older children or adults. There are numerous causes of optic neuritis. However, most cases are idiopathic. 20% of pediatric cases are associated with ADEM. Pediatric optic neuritis is usually not associated with multiple sclerosis (MS), with only 25% of children diagnosed with MS by age 40. In adults, 55% of optic neuritis patients subsequently develop MS.
ADEM is a monophasic, multifocal demyelinating disorder of the central nervous system. It primarily affects children. Mean onset in children is 8 years of age. The disorder often follows viral infection or vaccination. Most common presenting symptoms in one series included ataxia, head ache, and weakness. Other signs and symptoms include fever, nausea/vomiting, and nonspecific rash. A variety of focal neurologic deficits may be present, as with MS. Examination of CSF is typically normal. However, CSF can also show nonspecific findings which could suggest aseptic/viral meningitis, encephalitis, or MS. This was seen in our patient. Head CT scan is typically normal.
ADEM and MS have several features which can help to distinguish these seemingly similar disorders.
MS exhibits recurrent episodes of demyelination, while demyelination in ADEM is monophasic. Thus, MS typically shows demyelinating lesions of varying ages on MRI. MRI in ADEM typically exhibits lesions of the same age.
MS typically exhibits demyelination of the deep or periventricular white matter. ADEM usually involves the superficial white matter, often at the junction of gray matter and white matter.
CSF examination in MS is usually positive for oligoclonal bands, while CSF in ADEM is usually negative for this. Uncommonly, ADEM may exhibit oligoclonal bands. However, they usually resolve when ADEM resolves. Oligoclonal bands in MS usually remain positive indefinitely.
Despite these differences, up to one-third of ADEM patients are later diagnosed with MS. Furthermore, ADEM with recurrences has been described.
Treatment of ADEM is based on case series and case reports. Typically, steroids are administered IV, then PO. Unlike idiopathic optic neuritis, ADEM is treated for 4 to 6 weeks, followed by a taper. As with our patient, relapses can occur, especially with short courses of steroids. IVIG and plasmapheresis have also been reported in the treatment of ADEM.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS are variable, but can include:
|
TREATMENT
|
Tantri AP, Lee AG. Acute Demyelinating Encephalomyelitis (ADEM) with associated optic neuritis: 9-year-old girl presents to an outside hospital with fatigue, poor appetite, and decreased activity for 3 weeks. EyeRounds.org. February 21, 2005; Available from: http://www.EyeRounds.org/cases/30-AcuteDemyelinatingEncephalomyelitis.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.