Chief Complaint: 60-year-old male with 15 year history of serpiginous choroiditis reports a 2 day history of a new scotoma noticed on Amsler Grid testing of his right eye. His left eye is unchanged and has been about 20/125 for the last 13 years.
Medical History: Coronary artery disease. History of MI with stent placement.
Current Meds: Prednisone, 5 mg PO daily.
Ocular Exam:
 |
A fluorescein angiogram was performed to further characterize the lesion OD (see Figure 2).
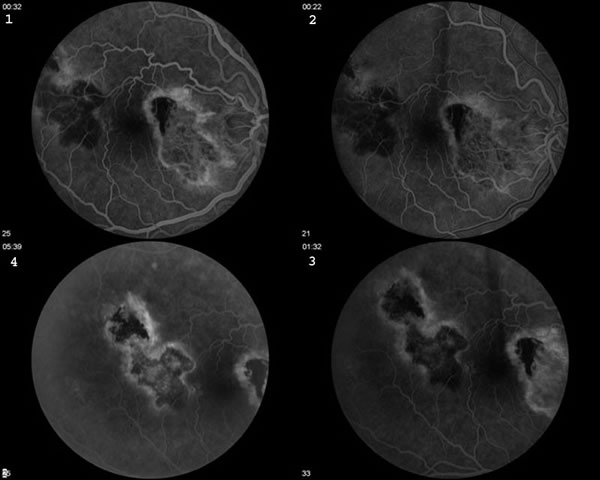 |
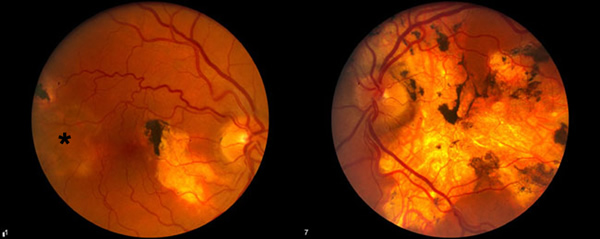
Serpiginous choroiditis is a bilateral idiopathic disorder characterized by geographic, helicoid destruction of the choroid and RPE. Subsequent destruction of the retina leads to a permanent visual disability, especially when the disease involves the central macula. This case demonstrates a variety of findings unique to this entity. In the right eye, one notices the old peripapillar scar. This disease frequently begins in the peripapillar region and spreads centripetally through the posterior pole. The left eye in this example shows the results of this progressive serpentine spread. Also, the right eye shows a scar along the superotemporal arcade with a characteristic area of active disease adjoining the old scar. Most of the time, areas of activation occur at the margins of old lesions. Occasionally, one will notice "skip" lesions that have areas of normal RPE between old scars and the new areas of activation. One will occasionally notice posterior vitreous cell and rarely, anterior uveitis.
The etiology of this disease is unknown. Immune mediated vasculitis with subsequent occlusion of the choroidal vessels is one proposed mechanism. An associated elevation of von Willebrand factor has been reported, but its significance is unclear. The fact that these patients have multiple recurrent inflammatory episodes has led some to speculate that infection (possibly herpesvirus) may be the cause.
Besides progressive foveal scarring, these patients also lose vision as a result of choroidal neovascularization. Retinal vasculitis and retinal vein occlusions may also occur.
Many combinations of anti-inflammatory regimens have been prescribed for serpiginous choroiditis. Azathioprine and cyclosporine have both been used as long term steroid sparing agents. Acute disease is regularly treated with corticosteroids. Intravenous, oral, periocular, and intraocular steroids have all been tried. There are some that recommend acyclovir based on the belief that herpes-virus may be the etiologic entity. Considerations when deciding upon a course of treatment for active lesions include proximity to the fovea, status of the other eye, presence or absence of a CNVM, systemic disease in the patient that may be exacerbated by treatment, previous experience of the treating physician and the patient's wishes. The efficacy of long term immunosuppression in preventing and/or minimizing recurrences has yet to be determined.
Plan: For this patient, we initiated pulse intravenous methylprednisolone at a dose of 1 gram/day for 3 days. Subsequently, we recommended an oral prednisone taper.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Zumbro D, Folk JC. Serpiginous Choroiditis: 60-year-old male with 15 year history of serpiginous choroiditis reports a 2 day history of a new scotoma noticed on Amsler Grid testing of his right eye. EyeRounds.org. February 21, 2005; Available from: http://www.EyeRounds.org/cases/32-SerpiginousChoroiditis.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.