Chief Complaint: 72-year-old white female returns to the cornea service with a known history of Fuchs' corneal dystrophy and decreasing vision.
History of Present Illness: This patient first presented as a referral from an outside doctor. For several years, the patient has had corneal guttae and increasing edema. During that time, the patient had experienced slow, progressive decrease in vision in both eyes. Her vision seemed worse in the morning and improved slightly as the day progresses. Options for management were discussed with the patient. For two years following presentation at the University of Iowa in 2002, the patient was managed conservatively and did fairly well.
However, a very gradual decrease in vision persisted during this time. The patient returned to the Cornea service in 2004 to further discuss treatment options for her decreased vision (OS>OD).
Past Ocular History: No ocular surgery, no contact lens use, and obscure history of minor needle trauma to OD at age 4. Patient has used glasses since age 7. Early cataracts have been noted in both eyes.
PMH: Migraine headaches, HTN, and mild asthma.
Family History: Diabetes, HTN, and glaucoma of unknown type.
Social History: Noncontributory
OCULAR EXAM
Both corneas had 4+ guttae. There were no bullae in either eye. There was measurable corneal edema. (Corneal pachymetry, OD was 585 microns and 607 microns in 2002 and 2004, respectively. Pachymetry, OS, was 591 microns and 620 microns in 2002 and 2004, respectively)
The risks and benefits of various treatment options were discussed with the patient. She decided to proceed with deep lamellar endothelial keratoplasty (DLEK) in her left eye.
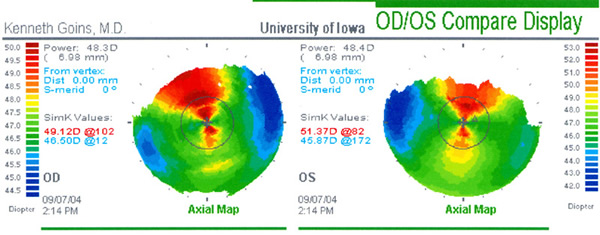
Corneal topographical maps were obtained preoperatively and are shown in Figure 1. (Pre-operative wavefront analysis was also performed and is shown in comparison to post-operative analysis in later figures).
 |
VIDEO: A deep lamellar keratoplasty (DLEK) was performed on her left eye. (if video fails to load, try this link)
Note: The evening after the surgery, the DLEK lenticule was noted to have subluxed inferiorly out of position. As can be seen in the video, this complication was treated by refloating the button into position and injecting an air bubble into the anterior chamber. This was complicated by a closed angle glaucoma attack that was relieved with dilation of the pupil.
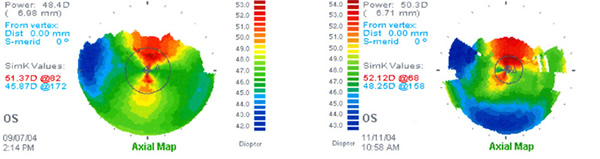
Post-operative corneal topography reveals relatively little change from her preoperative state, minimizing image distortion (Figure 2).
 |
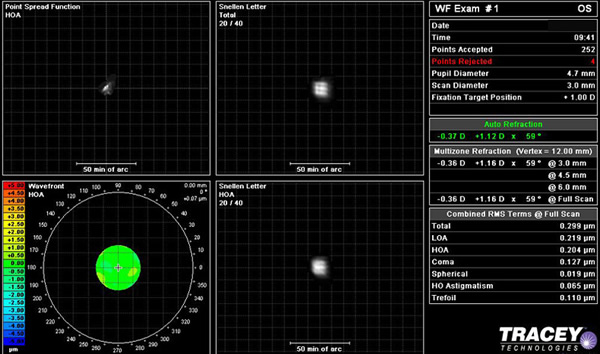
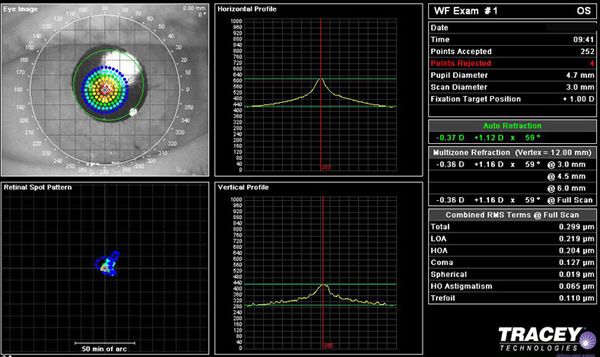
As noted, pre- and post-operative wavefront analysis was performed (Tracey technologies). One potential benefit of the DLEK procedure is the minimization of post-operative astigmatism. Indeed, in this patient, her post-operative auto-refraction is -0.37 +1.12 x059. Post-operative wavefront examination reveals relatively little change from her preoperative state, displaying no increase in higher order aberrations. This can be readily appreciated in comparing the two wavefront images. This can be readily appreciated in comparing the two wavefront images below. Pre and post-operative wavefront is shown here in sequence (Figure 3A and 3B).
| 3A: Pre-operative wavefront analysis and autorefraction, OS. A sample of the patient's view of the 20/40 Snellen "E" is seen in the middle frames and autorefraction is highlighted to the right of the image. |
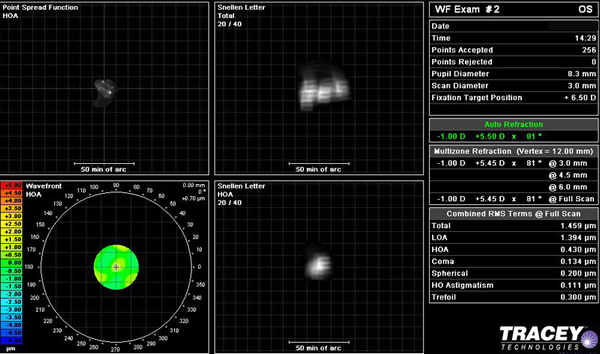 |
| 3B: Post-operative wavefront analysis and autorefraction, OS. |
 |
The retinal spot pattern, and vertical and horizontal profile of light refraction was also obtained. The post-operative analysis is shown in Figure 4. Light rays in both meridians came to focus nicely on the fovea.
 |
Though different types of lamellar keratoplasty have been described for over a century, deep lamellar endothelial keratoplasty (DLEK) first started to gain favor as an alternative to penetrating keratoplasty (PKP) just at the turn of this century. With DLEK, only the posterior portion of the cornea is replaced by donar tissue, as opposed to a full-thickness graft of transplanted tissue with the traditional corneal transplant (PKP).
Through a corneal or sclerocorneal incision (alternative entrance wounds are utilized), the host anterior chamber is accessed. A button of the dysfunctional host endothelium and deep stroma may be demarcated using an intracorneal trephine. The host button is then excised using microscissors and curved corneal dissecting blades (ie. Cindy I and II scissors). An open bed is thus created on the inner surface of the host cornea.
The donor tissue is then prepared for implantation as a similar button of tissue is excised. While this may be done from an intact donor globe, in the United States most donor buttons are typically dissected using only donated corneal rims and an artificial anterior chamber. After securing the donor cornea within the artificial anterior chamber, a microkeratome can remove a flap of epithelium and deep stroma, approximately 350 microns in depth. Similarly, the dissection of the donor may be done using manual techniques. Standard trephination techniques familiar to all transplant surgeons are then used to excise a donor button.
The donor button is then introduced into the host anterior chamber with a spatula or spoon-like instrument on a bed of viscoelastic material for large incision DLEK. Alternatively, the donor disc may be folded or—in cases of thin donor tissue—rolled and injected into the anterior chamber in small incision DLEK. The donor tissue is then carefully positioned within the defect in the host cornea and held up against the recipient bed by an injected air bubble.
The technique employed in this patient is the transplantation of a posterior donor disc through a corneal incision. The epithelium is minimally disturbed and no sutures are needed to secure the disc of donor tissue. By minimizing compromise of the anterior corneal surface, post-operative astigmatism is dramatically reduced. The absence of sutures further decreases astigmatic effect of the procedure and nearly eliminates the many suture-related post-operative complications of traditional transplantation procedures.
With the development and refinement of DLEK, surgeons and patients alike are discovering considerable advantages over traditional penetrating keratoplasty in the treatment of endothelial dysfunction.
Graff JM, Goins KM. Deep Lamellar Endothelial Keratoplasty (DLEK) for Fuchs: 72-year-old female with Fuchs. EyeRounds.org. February 25, 2005; Available from: http://www.EyeRounds.org/cases/33-DLEK-deeplamellarendothelialkeratoplasty.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.