INITIAL PRESENTATION
Chief Complaint: Left upper eyelid pain
History of Present Illness: A 28-year-old woman presented with a 1-month history of progressive left upper eyelid pain.
She initially presented to her primary care physician who diagnosed her with a stye of the left upper eyelid. She completed a 10-day course of cephalexin without improvement. Her symptoms progressively worsened until she went to her local emergency department, where she received intravenous steroids and a local ketorolac injection for presumed orbital myositis. She again experienced minimal improvement in her symptoms following treatment.
Due to ongoing pain, she later presented to the University of Iowa emergency department endorsing persistent left upper eyelid pain worsened with eye movement, particularly in upgaze. She denied any visual changes, flashes of light, floaters, visual curtaining, diplopia, pulsatile tinnitus, transient visual obscuration, fevers, chills, or unintentional weight loss.
Past Ocular History:
Past Medical History:
Medications: None
Allergies: No known drug allergies
Family History: Non-contributory
Social History: Non-contributory. No history of alcohol, tobacco, or drug use.
Review of Systems: Negative except for what is detailed in the history of present illness.
OCULAR EXAMINATION
OD:
OS:
Both eyes (OU)
MRI Brain with and without contrast
Echography
Labs:
|
Complete Blood Count (CBC) |
Within Normal Limits |
|
Complete Metabolic Panel (CMP) |
Within Normal Limits |
|
Thyroid Stimulating Hormone (TSH) |
Within Normal Limits |
|
Free T4 |
Within Normal Limits |
|
Rheumatoid Factor (RF) |
Within Normal Limits |
|
Anti-Neutrophil Antibody (ANA) |
Within Normal Limits |
|
Erythrocyte Sedimentation Rate (ESR) |
Within Normal Limits |
|
C-Reactive Protein |
Within Normal Limits |
Differential diagnosis:
CLINICAL COURSE
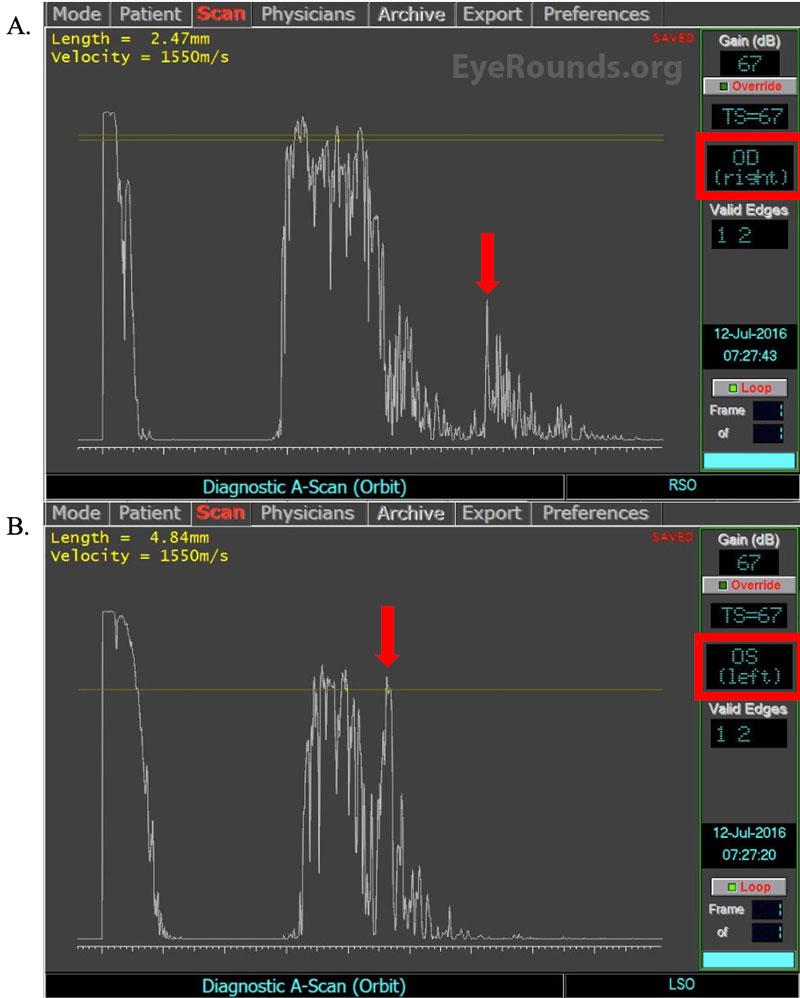
After being evaluated in the ED, the patient was started on high dose oral prednisone and was instructed to follow up outpatient with oculoplastics. Additional testing showed normal laboratory workup (Table 1), moderate thickening and mild enhancement of the left superior oblique muscle on MRI (Figure 1), and marked left superior oblique and trochlear enlargement on A-scan (Figure 2). At that time, she reported side effects from taking the prednisone and was instructed to see rheumatology for management with steroid-sparing agents. She was then switched from prednisone to methotrexate. However, despite 3 months of treatment with methotrexate, she continued to have left upper eyelid pain.
Upon her next follow up visit with oculoplastics (total of 4 months since initial presentation to UIHC ED), she received her first trochlear injection of 0.3 mL of dexamethasone at a concentration of 10 mg/mL mixed with 0.25 mL of 2% lidocaine without complication. She returned to clinic 1 month later stating her left upper eyelid pain had resolved. She would go on to receive dexamethasone with lidocaine injections monthly, with eventual extension of injections to every 3 months. As the dexamethasone and lidocaine combination injections were relieving her pain, the methotrexate was ultimately discontinued. Of note, her symptoms did not worsen following cessation of methotrexate. As the patient continued with her injections, both echography and CT of the orbits revealed reduced swelling of the left superior oblique muscle. The patient continues to receive injections on a 2- to 3-month basis with satisfactory symptom management.
DIAGNOSIS: Trochleitis/Superior Oblique Myositis
DISCUSSION
Etiology/Epidemiology
Trochleitis falls within the realm of orbital myositis and is defined as a local inflammation of the superior oblique muscle, traditionally characterized by periorbital pain in the region of the trochlea [1]. The etiology of trochleitis is often idiopathic, though it has been associated with inflammatory autoimmune conditions such as rheumatoid arthritis, systemic lupus erythematosus, psoriasis, and enteropathic arthropathy [2-6], as well as more rarely sinusitis, trauma, and cancer metastases [6]. The estimated prevalence of trochleitis in the general population is 12 per 100,000 [7], with females being affected twice as frequently as males [8-9].
Pathophysiology
The pathophysiology of trochleitis is not completely understood but is hypothesized to involve inflammatory, neuropathic, and neuromuscular etiologies.
The most widely accepted etiology of trochlear pain is inflammatory. First documented in 1984, biopsy of the superior oblique muscle in a patient with trochlear pain showed perivascular lymphocytic invasion of the myofibrils [15]. Notably, unilateral inflammation is generally considered idiopathic, while bilateral inflammation is highly correlated with systemic autoimmune conditions that, in addition to those listed previously, include Behçet's syndrome, granulomatosis with polyangiitis (GPA), and adult-onset Still's disease (AOSD) [16-19].
Another hypothesized cause of trochlear pain is neuropathic pain. Yanguela et al. postulated that repeated cycles of trauma to the supratrochlear and supraorbital nerves lead to altered nociceptive signaling perceived as pain in the periorbital or frontal hemicranial distribution [10].
Lastly, there may be a neuromuscular component to trochleodynia. This component may derive from myofascial trigger points (MTrP), especially in patients with a history of migraine and tension-type headaches11. It is theorized that provoking a MTrP could cause or even worsen nerve signaling11. MTrP in the superior oblique muscle could result in increased nociceptive input both from the supraorbital and/or supratrochlear nerves, therefore eliciting pain [12-14].
Signs/Symptoms
Pain associated with trochleitis is typically exacerbated both by up- and downgaze, especially in adduction. Physical examination is significant for erythema, edema, and point tenderness immediately overlying the superior oblique muscle and tendon in the trochlear region. Diplopia can also occur if inflammation is to the point of limiting extraocular muscle motility [1]. In some cases, the external examination can also be unremarkable.
Testing/Laboratory work-up
Thorough external, anterior, and posterior examinations should be performed for any patient presenting with concern for trochleitis. Assessment of extraocular motility is important to document for potential restriction. Cotton-tipped applicator testing to the trochlear region can also aide in the diagnosis to assess for focal trochlear tenderness.
Serum CBC and CMP should be obtained to evaluate for potential infectious etiologies or metabolic derangements. TSH should be tested for thyroid abnormalities, while ESR, CRP, RF, ANA, ANCA, and LFTs are used to evaluate for other associated systemic diseases [19]. Additional laboratory workup can be obtained depending on clinical presentation.
Imaging
Orbital imaging in the setting of trochleitis can be helpful in the workup of periorbital pain. Either CT or MRI of the orbits can be utilized and may reveal trochlear or superior oblique enlargement with signs of inflammation, though lack of radiologic abnormalities does not rule out trochleitis. Previous studies have shown only 20% of patients diagnosed with trochleitis exhibit radiographic findings [1,10,16,18,20-22]. Ocular echography is an additional tool to both evaluate extraocular muscle size and longitudinally assess treatment efficacy.
Treatment/Management/Guidelines
Current treatment options rely on anti-inflammatory therapies. Non-steroidal anti-inflammatory drugs (NSAIDs) are considered first-line therapy for mild, acute trochleitis [17]. If symptom resolution is achieved with NSAIDs alone, then NSAIDs can be used either on a scheduled or as needed basis.
More recently, local trochlear trigger point injections have been trialed with promising initial results [19]. Local trochlear trigger point injections with the combination of steroid and lidocaine can be used for patients who fail to find relief from NSAIDs alone, or those with persistent symptoms of trochleitis [19]. While there is no standard dose for the trigger point injections, published reports suggest 1– 3 mg dexamethasone with lidocaine, or alternatively, up to 40 mg triamcinolone with lidocaine, with an anticipated frequency ranging from 30 days to an as needed basis for flareups [19]. However, there are some conflicts with the safety profile between these two steroid medications, as triamcinolone has a larger particle size compared to dexamethasone and is associated with a higher risk of retinal artery occlusion [19].
The injection itself should be aimed slightly inferior or superior to the trochlea, but not in the direct region itself. Both an understanding of orbital anatomy and meticulous injection technique are advised to reduce the chance of iatrogenic globe rupture. Compiled studies revealed a 3.2% complication rate from local injections, including injection site hematoma, peri-trochlear hemorrhages, and incidental otitis, all of which spontaneously resolved shortly after [1,10,16,21].
Remission of symptoms varies widely in the literature, with some patients being strong responders following their first injection and no longer requiring subsequent treatment, while others needing several injections to achieve symptomatic relief of their trocheleitis [16]. A reported 95% of patients achieve a response to local steroid with lidocaine injections within 48 hours8, and these injections may lead to disease remission for a period of 18 months [19]. A separate report suggests local steroid and lidocaine injections early in the disease course may decrease the duration of inflammatory response and thus mitigate any extraocular muscle injury or development of refractory diplopia [20].
Oral steroids have also been documented in the treatment of acute onset of orbital myositis, most commonly with an initial dose of 60-80 mg per day for at least 2 weeks followed by a taper [23]. The literature reports an initial success rate of approximately 67% with the use of oral steroids, however, many patients experience side effects that hinder their ability to comply with the treatment [9.24.25]. Steroid sparing agents have also been documented in treating orbital myositis, including tacrolimus, infliximab, cyclosporine, cyclophosphamide, intravenous immune globulin (IVIG), and radiotherapy [26-30].
In summary, trochleitis should be considered on the differential of ocular pain. Although more studies are needed, advances have been made in the understanding of pathophysiology and management of the disease. Trigger point injections may represent a viable treatment option for patients suffering from trochleitis.
EPIDEMIOLOGY AND ETIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT/MANAGEMENT
|
References
Dotson AD, Diel RJ, Simmons BA, Shriver EM. Acute Onset of Unilateral Trochleitis . EyeRounds.org. August 25, 2022. Available from https://eyerounds.org/cases/330-acute-unilateral-trochleitis.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.