Chief Complaint: 61-year-old male presents to an outside hospital with eye pain and blurry vision, OD.
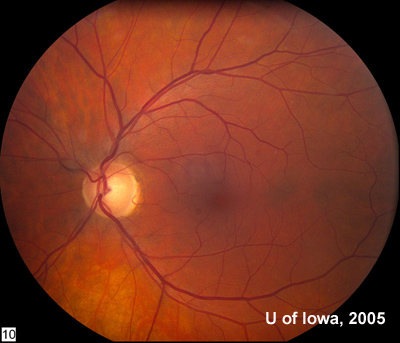
History of Presenting Illness: This patient initially noted blurry vision 6 weeks prior to this presentation. Pain had been steadily increasing since that time, for which the patient was referred to a local ophthalmologist. Locally, his vision was 20/80 and the physician noted inferotemporal choroidal infiltrate and exudative retinal detachment (RD). Echography of the eye was performed (B-scan) and mild choroidal thickening was observed.
Metastatic work up was performed due to the patient's history of lung cancer (see below). MRI of the head and orbits was performed at the outside facility and was negative for mass or infection. Laboratory work up and exam was otherwise negative. Following this evaluation, photocoagulation was applied to the choroidal lesion. Thereafter, the subretinal fluid was largely resorbed and the vision stablized.
However, 3-4 weeks later, the patient returned with increasing pain, nausea, and vision decreased again to 20/80. The patient was admitted locally for symptom control and further work up. Examination in the hospital revealed increased pain on extreme gaze, normal intraocular pressure (IOP), and a normal anterior segment examination. The globe was very tender to touch. On fundus examination, subretinal fluid (SRF) was noted to have recurred. A repeat B-scan was performed and again, slight choroidal thickening was evident, but there was no discrete mass. The patient was diagnosed with posterior scleritis and treated with steroids, NSAIDS, and pain control. While this regimen initially decreased the patients' pain and the SRF, both pain and SRF recurred within 2 months.
The patient was started on methotrexate and consultation from the University of Iowa was obtained. Examination is noted below.
Medications: aspirin, clopidogrel, metoprolol
 |
 |
 |
| 2A: Large exudative retinal detachment and pale inferotemporal mass, OD | 2B: Fundus, OD |
Fluorescein angiography was performed and is shown in Figure 3.
|
Ultrasound was performed, OD. This revealed thickening of the underlying choroid of 3 mm. The area had medium to high reflectivity and high vascularity. There appeared to be no subtenon or episcleral involvement.
Systemic work-up was repeated. The liver function tests and other lab tests were essentially normal. Positron Emission Tomography (PET) scan showed a lesion in the thoracic spine suspicious for malignancy. The radiation oncology team consulted on the case recommended a biopsy of the eye.
Pars plana vitrectomy (PPV) was performed with air-fluid exchange, endolaser, and retinotomy. A fine needle aspiration biopsy (FNA) was obtained and the retina was reattached over the mass. However, histological evaluation of the FNA material revealed no cellular material.
At this point, management concerns included lack of positive identification of the mass, unremitting eye pain for the patient, and a possible malignancy in the thoracic spine. Enucleation was considered as it may help deteremine curative versus palliative systemic treatment if the lesion was found to be a malignancy. Additionally, tissue examination of the eye may also help with diagnosis and management of the lesion in the thoracic spine.
The decision was made to enucleate for symptom control and diagnosis.
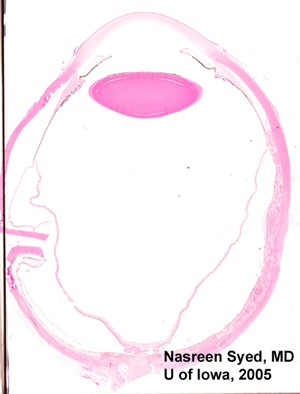 |
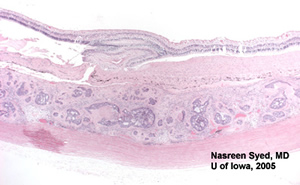 |
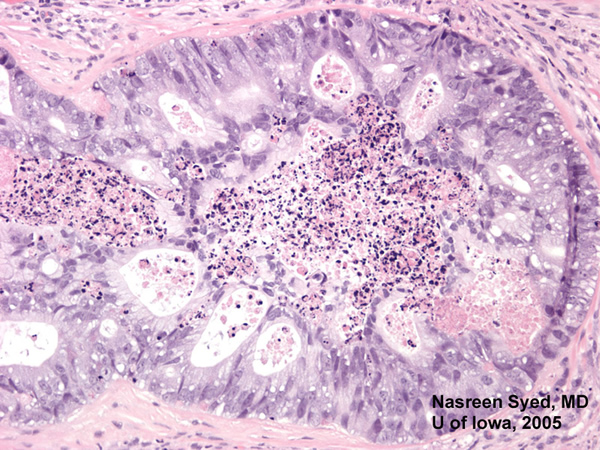
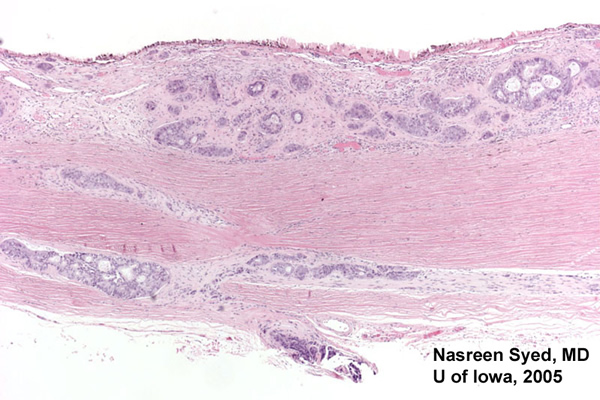
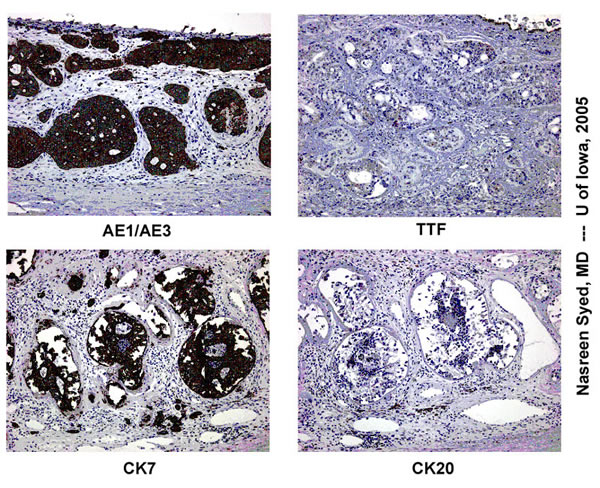
| Figure 4: Low power view of globe; PO section. Note extensive choroidal thickening along the right half of the photomicrograph. | Figure 5: Note glandular appearing tumor in choroid. Also note extensive fibrosis between choroid and retina. |
 |
 |
 |
Enucleation provided pain relief and definitive diagnosis. The thoracic spine lesion is likely another metastasis. The patient underwent palliative radiation therapy.
Metastasis is the number-one cause of intraocular malignancies. In autopsy studies, they are found in up to 12% of cancer deaths. Metastases are bilateral in 4.4%-23%. Multiple metastases are seen in one eye in up to 20% of cases. The choroid is the most frequent location probably due to its extensive blood supply.
For metastases diagnosed while patients are alive, the most common tumors differ based on age and gender. In adult men, lung cancers are most common, followed by malignancies with an unknown primary source. Even with detailed evaluation by oncologists, the primary source may not be identified in some cases of poorly differentiated tumors. In adult women, breast cancer is most common, followed by lung cancer.
In the case of lung cancers, metastases may be the initial presenting sign of cancer. This is important for the ophthalmologist to remember. Breast metastases, on the other hand, are typically discovered after diagnosis of the primary malignancy. However, breast metastases may be the first sign of recurrent disease. Other common primary adult tumors include GI (hepatoma, gastric, colorectal), renal, prostate, cutaneous melanoma, and testicular.
In the pediatric population, neuroblastoma is the most common cause of intraocular metastasis. Recall that rhabdomyosarcoma, a very common pediatric "eye" tumor, is an orbital—not an intraocular—tumor.
In the patient described in this report, the metastasis was a sign of recurrence. Radiation and multi-agent chemotherapy may prolong survival in advanced lung cancer.
Ultrasound can be a useful adjunct to diagnosis. It can be especially useful to differentiate metastasis from choroidal melanoma. Metastases demonstrate greater reflectivity on ultrasound than choroidal melanoma. They also demonstrate a lower height-to-base ratio than choroidal melanoma. Metastases are also more likely to present with multiple foci, either in the same or fellow eye, than are primary choroidal melanomas.
Fluorescein angiogram is useful to delineate borders of the metastasis. In some cases, early hyperfluorescence followed by late staining will be observed.
In cases of newly discovered intraocular mass, an appropriate systemic workup should be pursued based on the individual patient’s history and physical exam. Biopsy of the metastasis or enucleation may be helpful to provide a tissue diagnosis.
Treatment is based on the type of malignancy, and may include chemotherapy, hormonal therapy and radiation. External beam and plaque radiotherapy may be particularly useful for ocular metastases.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Tantri A, Syed NA, Weingeist TA. Metastatic Choroidal Lesion: 61-year-old male presents with pain and blurry vision OD. EyeRounds.org. March 9, 2005; Available http://www.EyeRounds.org/cases/35-MetastaticLungCA.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.