Chief Complaint: 3-year-old female referred for evaluation of increased size of left eye (OS).
History of Present Illness: The patient was initially noted to have tearing, OS, and was treated with antibiotics. At 1 year of age, the parents noted slightly increased size of the eye, OS. The patient was not seen by an ophthalmologist until age 3, when the asymmetric eye size became obvious and corneal haze noted, OS.
Ocular History: No previous ocular history. No eye surgery nor eye trauma.
Medical History: Unremarkable.
Medications: None
Family and Social History: Noncontributory
| A: External photograph during initial examination. Note the increased tear lake in the affected eye. | B: External photograph taken during examination under anesthesia (EUA). Note the increased corneal diameter, OS compared to OD, in both photographs. |
 |
 |
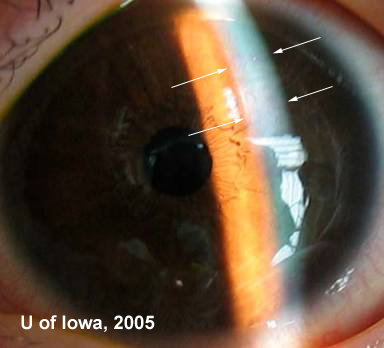
| Handheld slit lamp exam during examination under anesthesia. Note stromal edema superiorly (arrows). |
 |
Course: This patient's increased intraocular pressure, corneal edema, increased horizontal corneal diameter, and increased axial eye length point toward the diagnosis of buphthalmos and likely primary congenital glaucoma. The history of approximately 2 years of increased eye size OS would place the onset of disease around 1 year of age; typical onset of primary congenital glaucoma is between 3-6 months of age. The absence of any angle recession, posterior embryotoxon/iris strands/iris hypoplasia/corectopia, Peter’s anomaly, or aniridia help solidify this diagnosis.
The patient was treated with a trabeculotomy (SURGICAL VIDEO). After the surgical procedure, the intraocular pressure in the affected eye returned to normal (16 mm Hg). No further surgery was required and no pressure-lowering drops were needed to control the intraocular pressure thereafter.
Discussion: Glaucoma in infants can result from a number of secondary causes or be associated with systemic anomalies. However, when glaucoma develops within the first 3 years of life in the absence of any secondary cause or related systemic problem, the term primary congenital glaucoma is applied. The cause of primary congenital glaucoma is not completely understood, though there is significant research to suggest that the trabecular meshwork is immature and compressed. Studies suggest that the normal posterior migration of embryonic neural crest cells destined to become the trabecular meshwork is abnormally halted (Alward, 2000). The angle of children with primary congenital glaucoma is described as immature, thick, and compressed. High intraocular pressures are believed to be a consequence of increased resistance to aqueous outflow in this abnormal trabecular meshwork.
By definition, primary congenital glaucoma occurs in children between the ages of 6 months and 3 years. The majority of cases do not present at birth, presumably because even the abnormal drainage system can handle the minute amounts of aqueous humor that are produced in the infant eye during the first several months of life. Cases diagnosed at birth, then, tend to be more severe.
Though there have been some documented patterns of autosomal recessive inheritance of the disease (mutations in CYPB gene), most cases of primary congenital glaucoma appear to be sporadic.
Usually, parents will notice that their child experiences photophobia, tearing (epiphora), and/or blepharospasm in bright lights. This is the classic or "diagnostic triad" of symptoms. The pediatric eye will grow increasingly in response to the elevated intraocular pressure. This often results in an enlarged cornea and increased axial eye length in the affected eye. This can result in an enlargement of the globe, often referred to as "buphthalmos", meaning "ox eye". Corneal edema and haze is a common sign of the disease, as are horizontal or circumferential breaks in Descemet's membrane termed "Haab's striae" (see Figures 3 and 4). Haab's Striae will remain visible on examination throughout the patient's life, even if the edema resolves with normalization of intraocular pressure. On gonioscopy there is higher, flatter insertion of the iris at the level of the scleral spur, and the trabecular meshwork appears compacted.
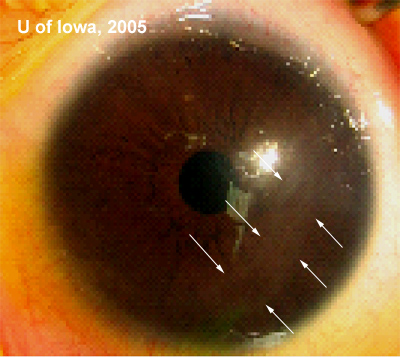
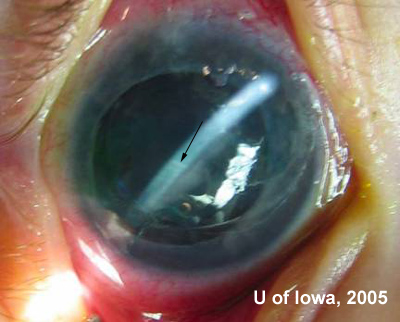
| A: Faint Haab's striae (arrows) from a different patient. | B: A second example of Haab's striae as seen in another patient. |
 |
 |
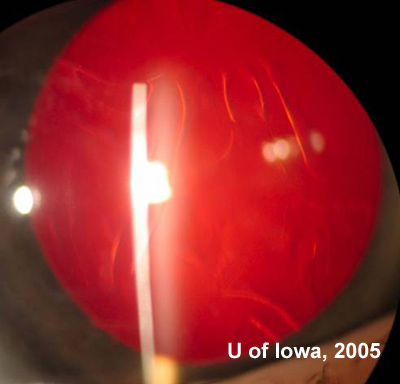
| Haab's striae as seen on retroillumination in another patient. |
 |
Unlike adult open angle glaucoma, the first-line treatment for congenital glaucoma is often surgical. First, however, the child must be examined carefully (usually in the operating room under anesthesia due to the difficulty of a detailed exam of an infant in the exam lane) to obtain accurate pressures, a detailed ocular exam, and photos. This will help to properly rule out any secondary cause of the glaucoma and obtain baseline data before proceeding with treatment. Once the diagnosis is confirmed under anesthesia, the surgeon will often proceed with appropriate surgery during this same anesthesia. The surgical treatment of choice is either a trabeculotomy or goniotomy. Both of these procedures surgically open up the immature, non-functioning trabecular meshwork and aim to restore normal outflow of aqueous from the anterior chamber to the Schlemm's canal. If surgery is succesful, intraocular pressure can be adequately controlled without the need for long-term topical medications.
Diagnosis: Primary Congenital Glaucoma (Infantile Glaucoma) with Buphthalmos, OS.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Maassen J, Kwon YH. Primary Congenital Glaucoma (Infantile Glaucoma): 3-year-old female referred for evaluation of increased eye size, OS. EyeRounds.org. June 20, 2005; Available from: http://www.EyeRounds.org/cases/42-Primary-Congenital-Glaucoma-Infantile-Glaucoma.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.