The patient was a 57-year-old man with vision loss in the right eye (OD) greater than left eye (OS) in the setting of a craniopharyngioma, which was resected 16 years prior. His visual acuity had been no light perception OD and 20/20 OS since the procedure.
Chief Complaint: 61-year-old Caucasian female presenting for evaluation of corneal mass OS found on routine exam ~2 months previous.
History of Present Illness: Patient was unaware of lesion when initially discovered. She denied pain or visual changes. Denied any growth of the lesion since discovery. She lives at a residential care facility.
PMH/FH/POH: schizophrenia, diabetes, and myopia. Medications: escitalopram oxalate, mupirocin, valproic acid, metformin, quetiapine fumarate, docusate, glipizide, lorazepam, and insulin.
EXAM
| OS | OS |
 |
 |
| Pigmented, elevated, fleshy mass on conjunctiva and extending onto the cornea. There is a sentinel vessel feeding the lesion. | Magnified view of the lesion denoting elevation and vascularity. |
| Pathology of Lesion | PAM with atypia |
|
|
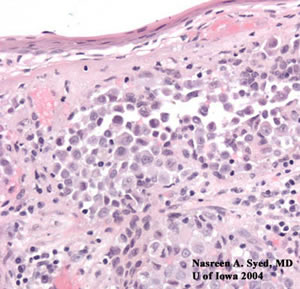
| Low powered view of lesion after excision from cornea and conjunctiva. There are areas of hypercellularity (blue cells) and inflammation. | Higher magnified view of the conjunctival epithelium denoting cellular atypia, discohesiveness, and nesting. These areas were Primary Acquired Melanosis (PAM) with atypia. |
| Pathology of Lesion | Nesting of Melanocytes |
 |
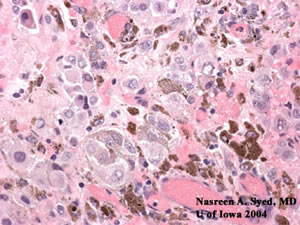 |
| Invasive cells with abnormal, large nuclei. These cells tend to spread in a pagetoid pattern and nested into groups. | Atypical melanocytes with large nuclei and pigment forming nests. |
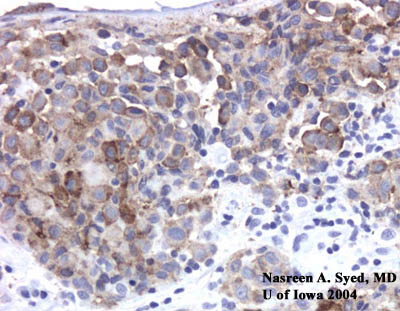 |
| Melanocytic cells were positive for MART-1. |
Conjunctival Melanoma
This conjunctival melanoma likely developed from primary acquired melanosis (PAM) with atypia and then grew onto the superficial surface of the cornea. In 1980, the WHO proposed the term PAM to describe this disorder. The term "primary" distinguished these lesions from complexion related, post-inflammatory, or systemic disease, and the term "acquired" distinguished these lesions from congenital. PAM has been suggested to be a precancerous melanosis, and lesions identified as PAM with atypia will have a 50% chance of progressing to a melanoma. PAM with atypia has a high recurrence rate if there is incomplete excision or corneal involvment.
Robert Folberg, M.D. described the following clinically significant histologic features of PAM: basilar hyperplasia (confined to basilar epithelium); basilar nests (anchored at basilar layer); intraepithelial nests (within epithelium, not anchored), pagetoid (individual melanocytes suprabasally); and in situ (full thickness). He also described cell types and atypia grade: small polyhedral (small round nuclei, scant cytoplasm - mild atypia); epithelioid (abundant cytoplasm - moderate atypia); spindle (large atypical cells perpendicular to the basement membrane - severe atypia); and, polymorphic (all of the above). In a study of 131 cases of conjunctival melanoma, 98 cases were associated with PAM and 33 cases were not associated with PAM. Of the 131 cases, 26% of the patients died from melanoma.
According to Dr. Folberg, risk factors for death from metastasis include:
Corneally displaced malignant melanomas are extremely rare. There are only 4 reported cases in the Finnish Cancer Registry between 1967 and 2000.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Maassen J, Goins K: Conjunctival Melanoma arising from Primary Acquired Melanosis (PAM): 61-year-old Caucasian female presenting for evaluation of corneal mass OS found on routine exam ~2 months previous. February 21, 2005; Available from: http://www.EyeRounds.org/cases/case15.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.