Chief Complaint: 81-year-old white male with sudden, painless vision loss OS.
History of Present Illness: The patient described a sudden black spot in his vision that spread out over his complete visual field OS over a 15-minute time frame. He drove directly to his optometrist. The optometrist documented visual acuities of 20/40 OD and light perception (LP) vision OS. It was noted that the patient had a normal fundus examination. The patient was sent to the University of Iowa for further evaluation on the following day.
PMH/FH/POH: coronary artery disease s/p CABG & balloon angioplasty, right carotid endarterectomy (1980s), left carotid stenting (endovascular) recently with transient right hemiparesis (resolved). No history of ocular surgeries or trauma. MEDS: ASA, Plavix, nitroglycerine PRN and alfalfa pills
ROS: denied headaches, jaw claudication, scalp tenderness, weight loss, and loss of appetite
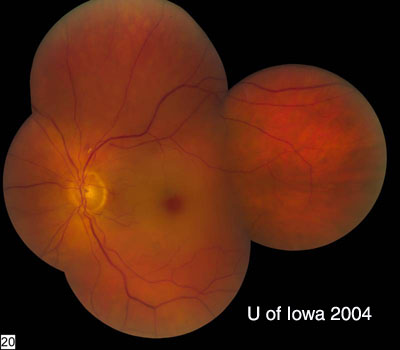 |
| Closer view of the optic nerve. | Arteriolar Dropout |
|---|---|
 |
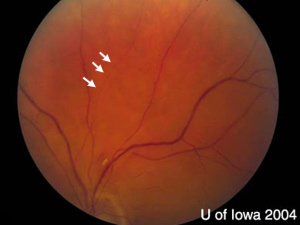 |
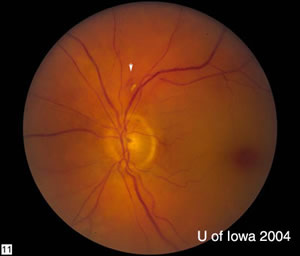
| There is an exudate and hemorrhage superior to the disc (arrowhead). The vessels also show some attenuation and their normally smooth appearance is irregular, especially in the superior-temporal arcade. Optic nerve is normal in appearance. | There is "box-carring" of the flow through the small vessel nasal to the hemorrhage (arrowhead). |
| Box-Carring of Vessel
|
Angiography
|
| There is "box-carring" of the flow through the small vessel nasal to the hemorrhage (arrowhead). This is a magnified view of the photo above. | FFA images at 1:00 minute demonstrating very poor filling. The earliest filling that occurred on the angiogram was not until 21 seconds. |
The patient’s classic description of painless, sudden loss of vision one day prior to presentation, and the appearance of the "cherry-red spot" on fundus examination made the diagnosis of a central retinal artery occlusion (CRAO). This elderly patient had a history of coronary artery disease s/p bypass surgery as well as carotid vascular disease treated with an endartectomy on the right in the 1980s; and more recently, endovascular stenting of the left carotid, the same side as the CRAO. We believed that the CRAO was likely to have been caused by the carotid disease. Our differential diagnoses included carotid artery dissection, stent thrombosis, carotid artery restenosis, or an arteriole embolism, for example from the carotid or less likely, a cardiac source. Although our patient had a negative review of systems for giant cell arteritis, 5-10% of CRAOs are associated with giant cell arteritis (Walsh and Hoyt). A STAT erythrocyte sedimentation rate and c-reactive protein was performed and both were normal.
We elected to continue the patient’s aspirin and plavix. In the acute presentation of a CRAO, some interventions are recommended to attempt to restore blood flow to the retina. These maneuvers include ocular-digital massage with or without an anterior chamber paracentesis, and with or without oral medications such as acetazolamide to lower the intraocular pressure. The theory behind ocular-digital massage is that the steep increase in pressure followed by a sudden return to normal pressure may act to plunge an embolus farther along the vascular pathway into a distal branch with potentially less catastrophic compromise to the retinal blood supply. The patient should be educated on the use of ocular-digital massage for the contralateral eye if a second CRAO occurs. The anterior chamber paracentesis and oral medications act to lower intraocular pressure and may help to relieve any compression of the vasculature. Some may argue that even in this case of presentation greater than 24 hours after onset, the less invasive procedures should be tried because they could have some benefit. However, Dr. Hayreh has demonstrated that irreversible damage occurs after as little as 100 minutes of occlusion and more recently has demonstrated that greater lengths of time of occlusion (from 97 minutes to 240 minutes) are associated with more damage histopathologically (Hayreh 1980, 2004). Given that the patient presented to us 29 hours after the onset, we did not perform these interventions. However, we did obtain consultation by our neurology Stroke Service. They continued the patient’s aspirin and plavix, admitted the patient to the hospital, and performed an angiogram to evaluate the carotid circulation. This demonstrated a left carotid dissection at the site of the carotid stent. Interventional radiology then placed a telescoping stent over the site of the dissection. The patient will require carotid ultrasound every 6 months to monitor for stenosis or development of new dissection.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
O'Malley E, Lee AG: Central Retinal Artery Occlusion (CRAO): 81-year-old white male with sudden, painless vision loss OS. February 21, 2005; Available from: http://www.EyeRounds.org/cases/case20.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.