Chief Complaint: 43-year-old male referred for evaluation of binocular diplopia.
History of Present Illness: Patient had a sudden onset of binocular, vertical and torsional, diplopia subsequent to a CVA 2 years prior to presentation. He noticed some improvement over the initial 6 months but the diplopia had been constant since then. He also complained about oscillopsia that was more pronounced in upgaze. The family members noticed an anomalous chin up position subsequent to the CVA.
PMH/FH/POH: Patient was comatose after a sudden onset of intracranial bleed 2 years prior to presentation, and he underwent bilateral ventriculostomy followed by ventriculoperitoneal shunt for acute hydrocephalus. Developed pulmonary embolism 1 month after the bleed. Developed lower limb deep venous thrombosis 6 months prior to presentation. FH significant for blood coagulopathies in multiple family members.
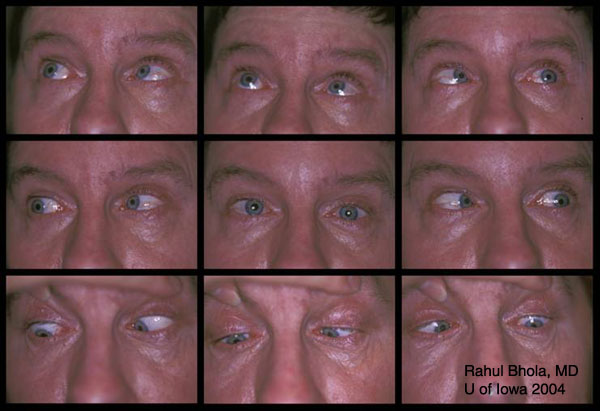
SYSTEMIC: Ataxia, sluggish speech, tremors of the right hand and weakness of lower extremities. OCULAR:
 |
 |
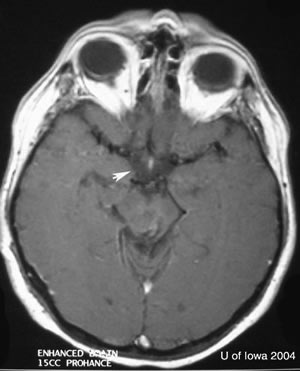 |
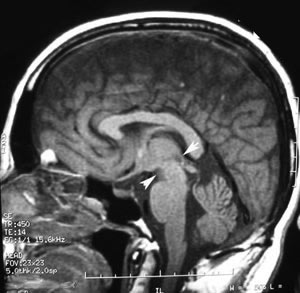
| Saggital T1 MRI scan of the head without contrast. Evidence of prior brainstem hemorrhage (arrowheads) extending vertically from posterior pontomesencephalic junction into the cerebral peduncle with hemosiderin staining of superior cerebellar peduncle. | Axial T1 MRI scan of head with contrast. Following administration of contrast, there was enhancement along the margins of the hemorrhagic cleft which could be an underlying occult vascular malformation/sequelae from prior hemorrhage. |
The cause of diplopia, oscillopsia, and anomalous head posture in this patient was a combination of dorsal midbrain syndrome and bilateral superior oblique palsy. This patient developed an idiopathic brainstem hemorrhage that extended from the ponto-mesencephalic junction upto the cerebral peduncles involving the rostral midbrain. Subsequent angiography was inconclusive for arteriovenous malformation. The signs of dorsal midbrain syndrome seen in this patient were light near dissociation, convergence retraction nystagmus, and vertical gaze palsy. The signs of bilateral superior oblique palsy seen in this patient were chin-up position, ‘V’ pattern esotropia, alternating hypertropia, bilateral superior oblique underaction and significant excyclotorsion.
The supranulcear vertical gaze limitation in this syndrome results from involvement of the posterior commissure, interstitial nucleus of Cajal, or rostral interstitial nucleus of the medial longitudinal fasciculus.
Considering the amount of torsion, head posture, and significant ‘V’ pattern, we performed a bilateral superior oblique tucking (15 mm OD and 11 mm OS) along with a bilateral recession of medial recti by about 4.5 mm with half-tendon-width infraplacement of the medial rectus tendons. Postoperatively the torsion was significantly corrected, and the patient had a moderate residual esotropia in primary gaze.
EPIDEMIOLOGY
|
SIGNSMAJOR COMPONENTS
MINOR COMPONENTS
|
SYMPTOMS
|
TREATMENT
|
Bhola R, Keech RV, Olson RJ: Dorsal Midbrain Syndrome (Parinaud's Syndrome) with Bilateral Superior Oblique Palsy: 43-year-old male referred for evaluation of binocular diplopia. February 21, 2005; Available from: http://webeye.ophth.uiowa.edu/eyeforum/case21.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.