PMH/FH/POH: Hypothyroidism on thyroid replacement. Headaches, as described above. No POHx. Patient's rhinorrhea and headache had been treated symptomatically by previous physicians. The patient is a smoker (cigars and cigarettes).
EXAM OCULAR:LABS: ESR normal
 |
|
This gentleman originally presented to his primary care practitioner complaining of rhinorrhea and headaches. Suspecting that the headaches were due to sinus pressure, the patient was treated for infectious sinusitis. This offered no relief and the symptoms continued. Two weeks later, the patient returned to his primary care practitioner with more detailed complaints. At this second visit, he then further described excruciating, unilateral, throbbing headaches that came at varied times and did not subside despite attempts to rest, or to avoid light and noise, and that the patient was made more uncomfortable by attempts to remain still. He also noted that he had concurrent aching teeth and the previously described rhinorrhea. A diagnosis of cluster headache was made and the patient was offered acetaminophen and non-steroidal anti-inflammatory medications which provided only minimal relief. It was in the week that followed that the patient’s wife first began to notice that his right eye (ipsilateral to the headaches) seemed "sunken and droopy" and that his face flushed just preceding and during the headaches.
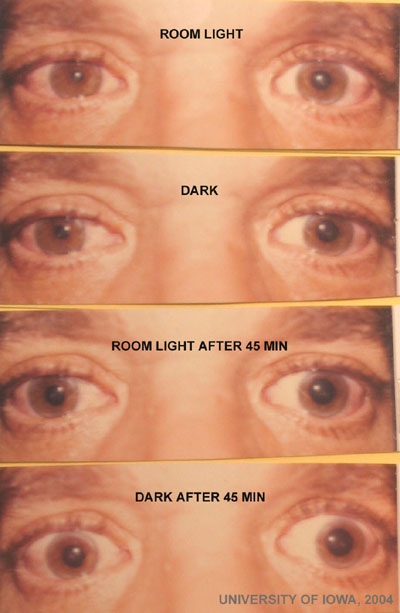
Noting these additional symptoms, the patient was directed to our ophthalmology service for further evaluation. Upon examination, the patient was seen to have mild ptosis and reverse ptosis as well as anisocoria (with small pupil, OD).
A cocaine test was done to confirm the suspected diagnosis of Horner's Syndrome.
 |
Note that the affected pupil (OD) dilates less to cocaine stimulation as compared to the normal pupil (OS). In the normal state, norepinephrine is released from the presynaptic neurons as part of baseline sympathetic tone. Reuptake of the norepinephrine is a constant part of neurotransmitter recycling. Cocaine blocks reuptake of norepinephrine, causing rapid accumulation within the synaptic cleft which results in dilation of a normal pupil. The presynaptic nerve endings in a Horner’s patient have diminished sympathetic tone and thus respond poorly to the effect of cocaine.
This positive cocaine test confirmed the diagnosis of Horner's Syndrome in our patient. To further evaluate where in the neuronal pathway the sympathetic nerves are being affected (i.e., 1st order, 2nd order, or 3rd order), the hydroxyamphetamine test was performed.
 |
Hydroxyamphetamine forces active release of stored norepinephrine from the presyntaptic nerve ending which will cause dilation of either pupil as long as the 3rd order neuron is intact. Postitive pupillary dilation in response to the hydroxyamphetamine test indicates that the cause for the Horner’s syndrome lies upstream, either in the 1st or 2nd order neuron.
In this case, his pupil did not responsd to hydroxyamphetamine, confirming 3rd order neuron involvement. Given the classic history in this particular case, cluster headache causing a 3rd order neuron Horner’s syndrome might already be strongly suspected. However, there is some discussion about the appropriate work-up for any new new-onset Horner’s syndrome. In this particular patient, with a strong smoking history, other etiologies must be considered. Though a 2nd order Horner’s (i.e., Pancoast tumor) has been ruled out by the hydroxyamphetamine test, mass in the head and neck could result in the same response to testing. Additionally, in young patients with recent chiropractic manipulation or other neck trauma (MVA, roller coaster, etc), carotid dissection cannot be firmly ruled out without imaging. Because the hydroxyamphetamine test is not 100% sensative in localizing incomplete lesions of the sympathetic pathway, some texts recommend that all new cases of Horner’s syndrome warrant imaging. A CT of the chest, MRI/MRA of the head and neck, and CBC are recommended.
In this case, MRI/MRA from the hypothalmus to T2 (the extent of the sympathetic pathway in the spinal column) was performed. This was negative.
In the absence of other positive findings on exam/MRI/MRA, and with a classic picture of cluster headache by history, the diagnosis was Horner’s syndrome due to cluster HA.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
1st order neuron:
2nd order neuron (spinal cord, thoracic cavity, and lower neck)
3rd order neuron (upper neck and carotid arterial pathway)
Graff JM, Lee AG: Horner's Syndrome (due to Cluster Headache): 46-year-old male presenting with HA and ptosis. February 21, 2005; Available from: http://www.EyeRounds.org/cases/case22.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.