Nasolacrimal Stents: An Introductory Guide
Aaron M. Ricca, MD; Allison K. Kim, BS; Harinderpal S. Chahal, MD; Erin M. Shriver, MD, FACS
posted January 29, 2018
See related videos at https://eyerounds.org/video/plastics/index.htm#lacrimal
Nasolacrimal stents are small diameter tubes placed within the nasolacrimal system to maintain patency. The first described stent was made of silver wire and used by Graue in 1932.[1] Since that time, various materials have been used, including silk, nylon, polyethylene, and polypropylene.[2] Today, the tubes are typically composed of silicone, or another similar semi-rigid yet flexible material with an open central lumen. Intubation of the nasolacrimal system is generally done temporarily, with stents remaining in place for several months. In rare instances, however, intubation may be long term.[3] Nasolacrimal tubes are used primarily in cases of obstruction or laceration of one or more parts of the tear drainage system.[4]
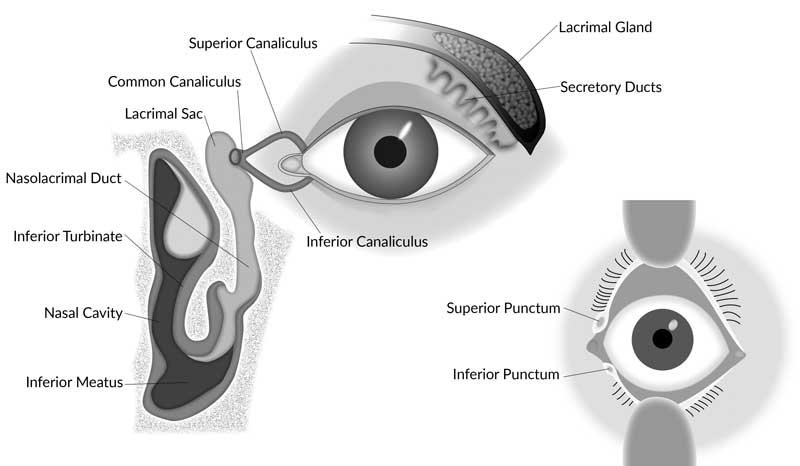
The differential diagnosis of nasolacrimal obstruction is broad and includes trauma, infection, malignancy, thermal injury, chemotherapy, radiation, and iatrogenic causes.[3] Regardless of the specific etiology, patients with nasolacrimal obstruction typically present with epiphora, an overflow of tears onto the cheek due to improper drainage through the nasolacrimal system.Normal tear drainage occurs with an intact nasolacrimal drainage system and a functioning lacrimal pump (Figure 1). Tears exit the ocular surface via the upper and lower puncta. They then enter the superior and inferior canaliculi, which coalesce to form a common canaliculus in 90% of people.[3] At the junction of the common canaliculus and the lacrimal sac is the valve of Rosenmueller, a small fold of mucous membrane. The sac narrows inferiorly, becoming the nasolacrimal duct, which opens beneath the inferior turbinate and into the inferior meatus of the nose. The valve of Hasner, located at the distal end of the nasolacrimal duct, prevents retrograde reflux of air, mucous, and food particles from the nose into the eye.
Figure 1. The nasolacrimal drainage system. Vaughan & Asbury's General Ophthalmology, 18ed. Chapter 1. "Anatomy & Embryology of the Eye" - Modified figure used with permission
Obstruction along any of the following sections of the nasolacrimal drainage system may be an indication for intubation:
- Punctum (superior or inferior)
- Proximal canaliculus (partial obstruction of the superior canaliculus, inferior canaliculus, or both)
- Common canaliculus
- Lacrimal sac
- Nasolacrimal duct
Blockage of flow anywhere in the system can be idiopathic or secondary to numerous causes including infectious, malignant, traumatic, autoimmune or other inflammatory disorders. One of the most common indications for intubation is post-surgical, such as in a dacryocystorhinostomy to maintain a patent osteotomy.[5 ,6] This procedure was first described by Lester Jones in 1962 and has since had numerous advancements in techniques and materials.[7 ,8]
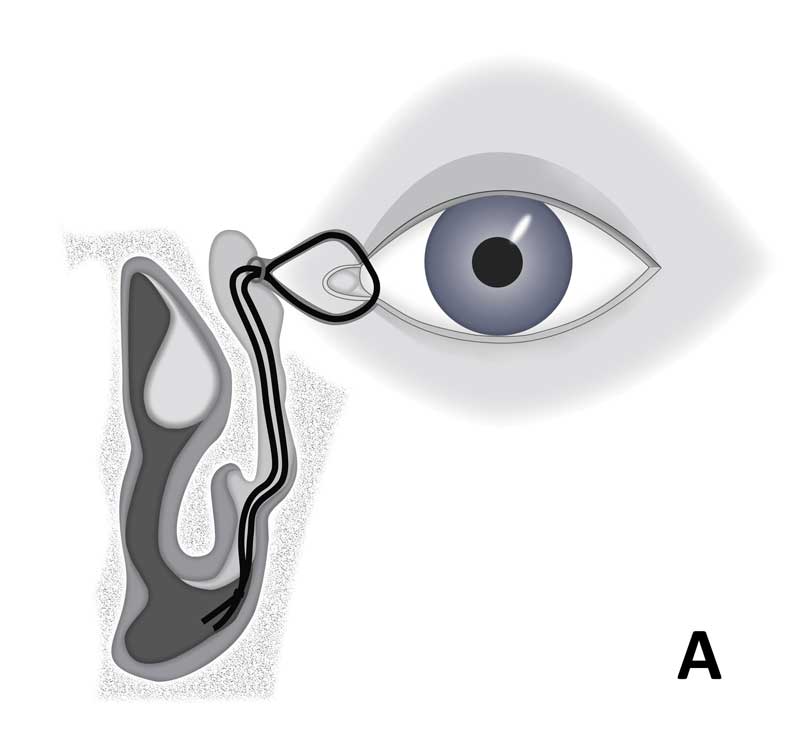
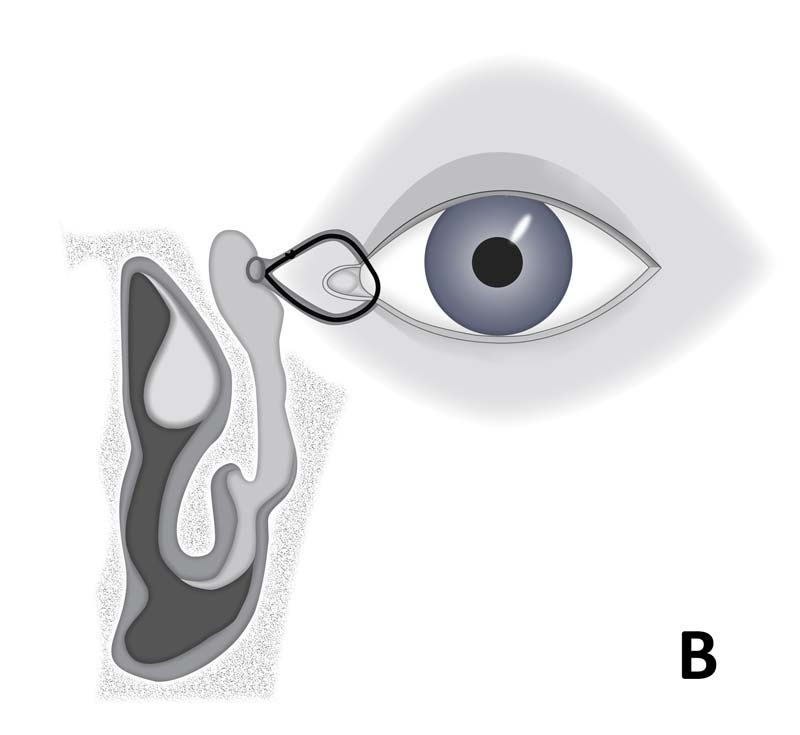
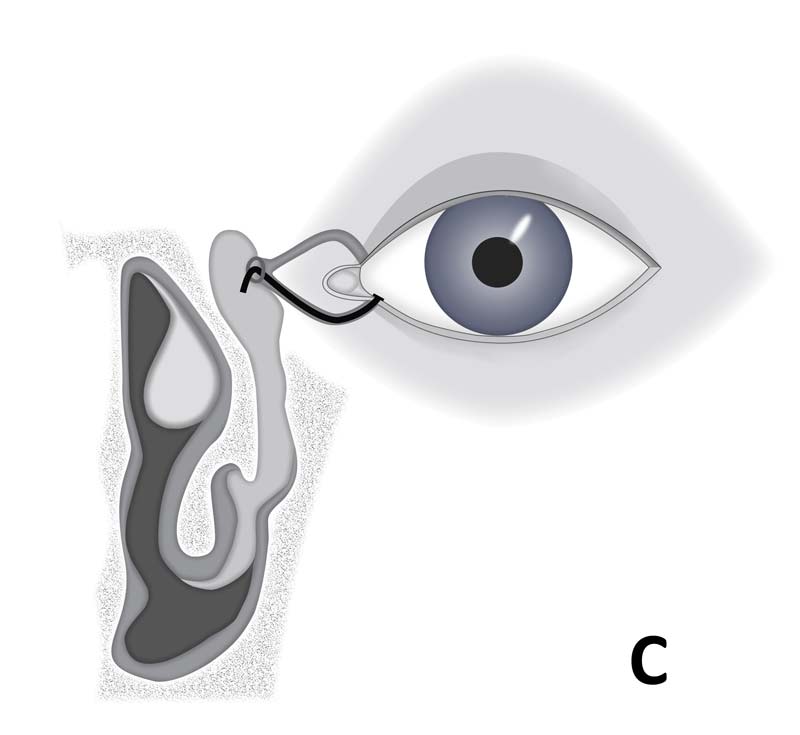
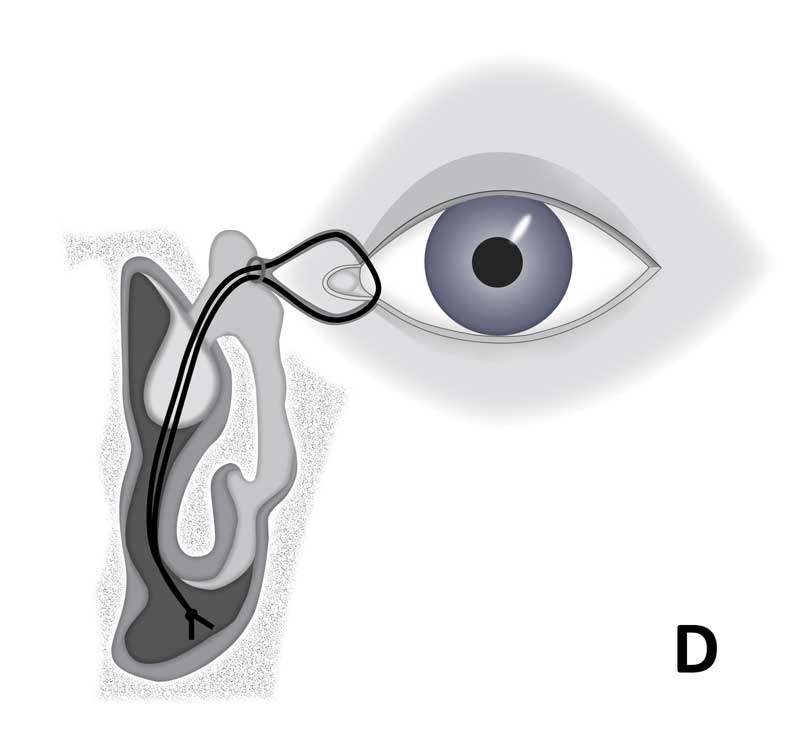
Canalicular stents can be organized based on the different parts of the nasolacrimal drainage system they intubate. The two main divisions of stents are bicanalicular versus monocanalicular. Bicanalicular stents pass through both the upper and lower canaliculus and typically create a closed circuit.[9] They can intubate the upper and lower canaliculi connecting via the common canaliculus or the lacrimal sac (Figure 2a). They can also intubate the entire nasolacrimal drainage system, including the lacrimal sac and nasolacrimal duct with the circuit being open or closed in the nose (Figure 2b). Monocanalicular stents do not provide a closed loop system, only intubating either the upper or lower canaliculus[4] (Figure 2c). A surgical procedure can create a new passageway for stents to be placed into the nose (Figure 2d) or completely bypass the entire canalicular system (Figure 2e). Several examples of both bicanalicular and monocanalicular stents are presented below. This list is by no means meant to be exhaustive, as there are numerous types of both bicanalicular and monocanalicular stents currently available on the market. Instead, this is merely representative of the major categories of stents currently utilized at the time of publication.
 |
 |
 |
 |
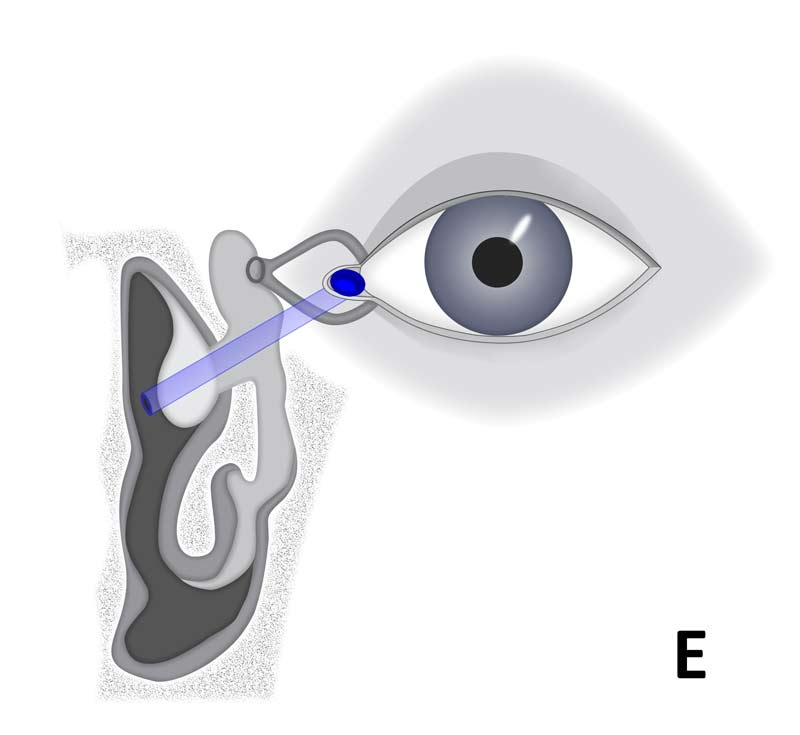 |
Figure 2. Diagrammatic representation of the different stents and the anatomical location they involve
1. Bicanalicular Stents
Stenting of upper and lower canaliculi
Crawford stent
Involves the entire nasolacrimal drainage system (Figure 2a)
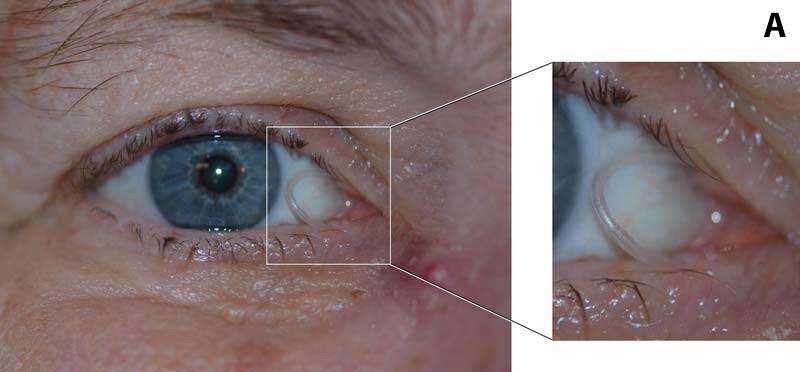
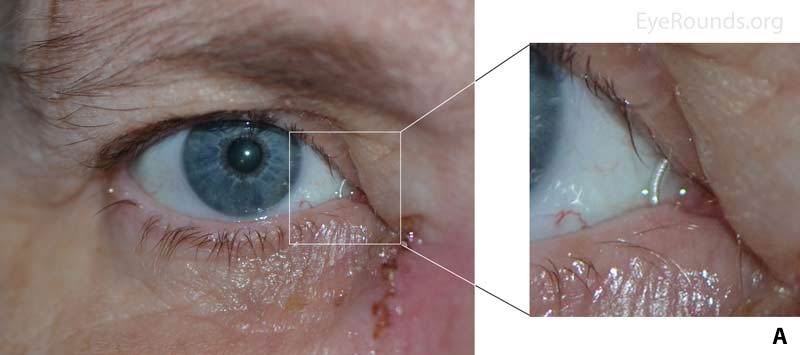
The Crawford stent is a bicanalicular stent attached to metal probes with bulbs on the distal ends of the probes. The probes and attached stents are passed through the superior and inferior canaliculi and retrieved in the nose via a retrieval hook or groove director that engage the bulbous tip of the probe (Figure 3b). The stents can be a full silicone rod or silicone tubing with an inner silk suture. The probes are subsequently cut and the stents are tied in the nose. When the stent contains a silk suture, the stent is stripped from the suture at the ends, and the silk is tied creating a loop of stent. This suture is barely visible once the stent is in place as the suture is white. To reduce risk of stent prolapse, some surgeons decrease the length of the stent loop with a ligating suture around the loop within the nose. The stent is either left free-floating in the nasal cavity or fixated with a suture to the mucosa of the lateral nasal wall. The small silicone stent passing between the upper and lower puncta is visualized in Figure 3a below. This was placed after a dacryocystorhinostomy (DCR) from an external approach, as is evident by the incision. In this procedure, a surgical opening is created between the lacrimal sac and the nasopharynx allowing for passage of the stent (Figure 2d).
Figure 3. (A) Silicone tubing of the Crawford stent connecting the upper and lower puncta and a healing incision from DCR. (B) Diagram of Crawford stent attached to metal probe, compliments of FCI Ophthalmics
Ritleng Stent
Involves the entire canalicular system (Figure 2a)
Designed by Dr. P. Ritleng, this system utilizes an introducer with a hollow lumen and stylette. The introducer, loaded with the stylette for rigidity, is used to enter the nasolacrimal system. Once inside, the stylette is removed and one end of a bicanalicular stent is advanced through the hollow lumen of the tube.[1] The procedure is repeated via the opposite punctum, and the stents are tied in the nose. The Ritleng stent is the bicanalicular stent of choice for some surgeons because the design minimizes manipulation inside the nose.
Figure 4. (A) Silicone tubing of the Ritleng stent connecting the upper and lower puncta. (B) Diagram of stent with stylette, compliments of FCI Ophthalmics
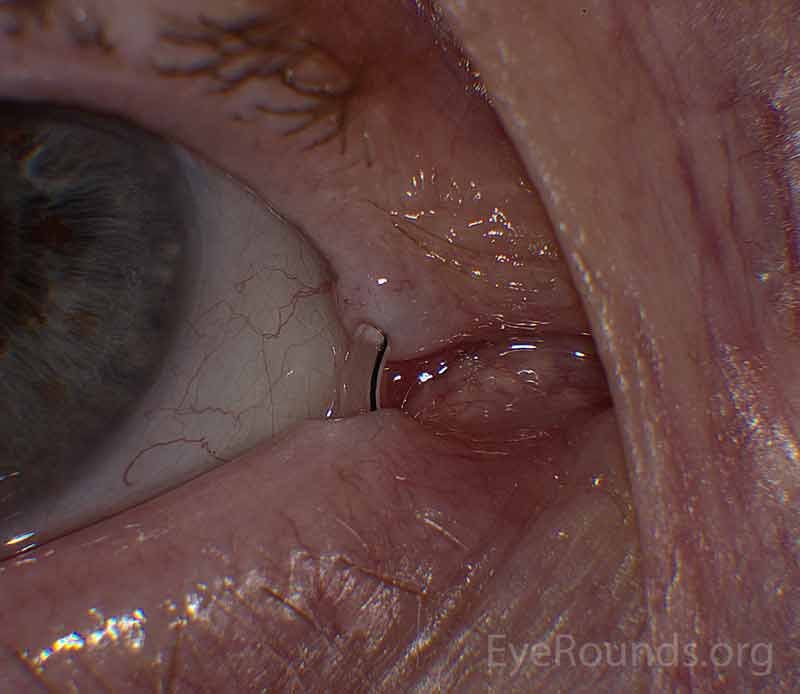
Pigtail/Donut stent
Involves the upper, lower, and common canaliculi (Figure 2b)
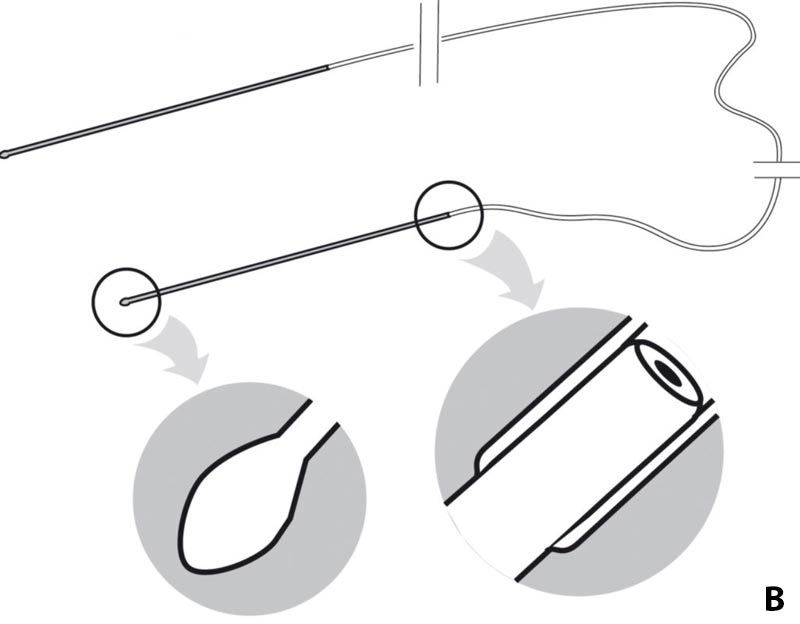
This stent is used for bicanalicular intubation. It is commonly used in traumatic canalicular laceration repairs where the patency of the nasolacrimal duct remains intact. One end of the pigtail-shaped probe is designed for insertion through the upper canalicular system, while the opposite end is designed for insertion through the lower canalicular system. The probe is passed through one puncta and rotated, following the natural curvature of canalicular system, then retrieved via the opposite punctum. A small islet at the tip of the probe facilitates passage of a guide-wire suture (we prefer a 6-0 nylon suture) through the canalicular system. A piece of hollow silicone tubing, cut to approximately 25 mm in adults, is then passed over the guide wire to successfully intubate the canalicular system. The suture is then cut and tied and the stent rotated to bury the knot. When viewing only the stent between the puncta, one can distinguish between a Crawford and a pigtail stent by the presence or absence of a black nylon or blue prolene suture within the stent lumen vs no suture or a white silk suture in the Crawford stent (Figure 6).
Figure 5. Pigtail probe used to pass the guide-wire suture through the canalicular system. Image compliments of Indiamart (https://www.indiamart.com/proddetail/lacrimal-pigtail-probe-14549996330.html)
Figure 6. Pigtail stent with a black nylon suture visible within the stent lumen
Kaneka Lacriflow stent
Involves the entire nasolacrimal system (Figure 2a)
The Kaneka Lacriflow stent is a new system that was approved for bicanalicular intubation by the FDA in 2012.[10] The stent is made of a central thin intra-canalicular portion with larger diameter tubing at either end that intubates the lacrimal sac and duct. The ends are attached to stainless steel bougies allowing for insertion (Figure 7). Once placed, the ends of the stent reside under the inferior turbinate without suture fixation. The benefit is that the stent is self-retaining with minimal intranasal manipulation allowing for placement under local anesthetic.
Figure 7. (A) Kaneka Lacriflow stent with attached bougies, (B) Schematic of the stent demonstrating variable diameter and openings in the system [10], images compliments of Kaneka Pharma America, Kaneka-eye.com
2. Monocanalicular Stents
Stenting of upper or lower canaliculi
Monoka Stent
Involves a single canaliculus (Figure 2c)
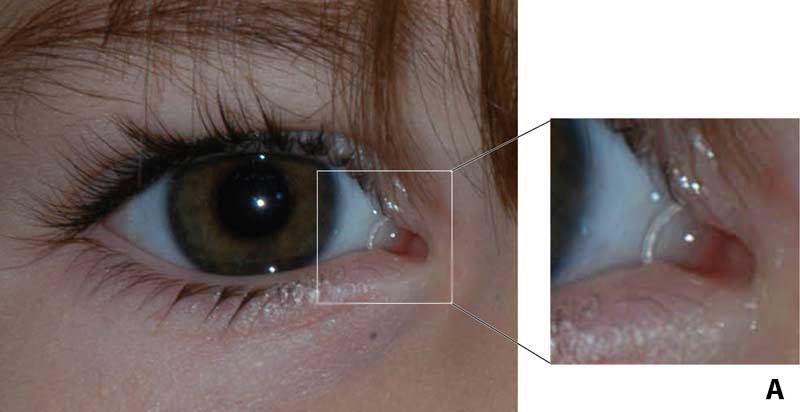
This silicone stent is anchored at the punctum by a plug/cap on one end. No suturing is necessary to keep it in place, although some surgeons prefer to secure the stent to the eyelid with a suture through the lip of the stent. This type of stent is used to treat nasolacrimal duct obstructions, canalicular stenosis, and it can be used for canalicular lacerations.[1]
The mini Monoka stent is a smaller version and is used to treat lacerations or obstructions that occur in the canaliculus. Like the full-size version, it is anchored at the punctum of the eye by a plug on the end of the stent.[1]
![Mini Monoka stent over a patient's eyelids prior to insertion[1]](Fig8a.jpg) |
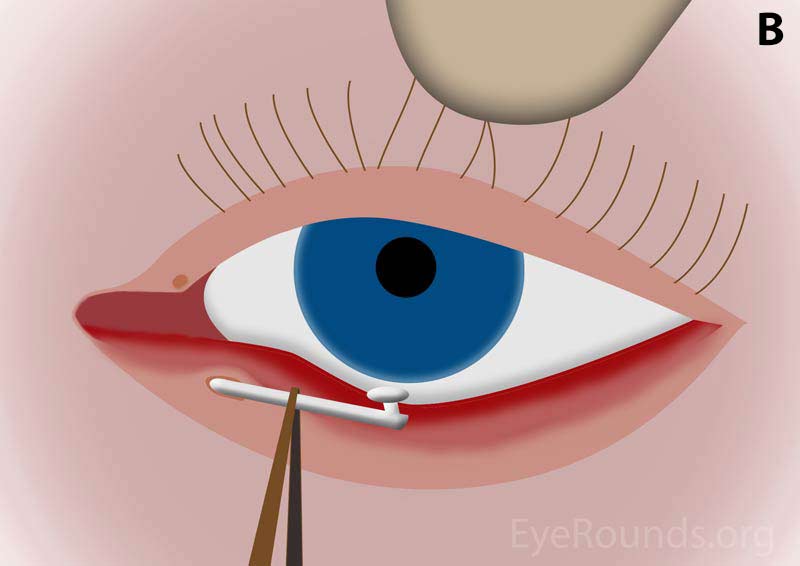 |
Figure 8. (A) Mini Monoka stent over a patient's eyelids prior to insertion[1]. (B) Diagram demonstrating insertion of the stent into the inferior punctum.
Jones Tube
Does not involve the canaliculi
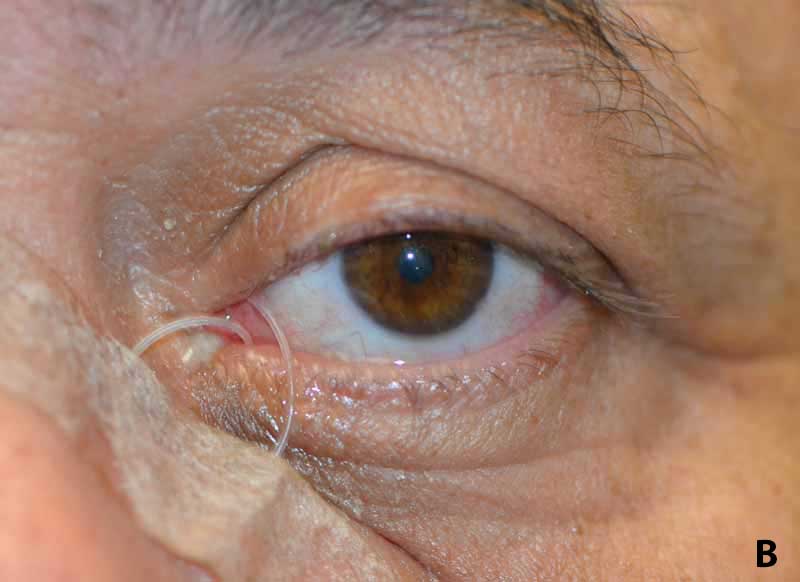
The Jones tube is a Pyrex glass tube that is used to bypass an obstruction of the canalicular system in order to drain tears from the eye. It is placed from the conjunctival cul-de-sac through a surgically created bony ostium, and exits into the nose (Figure 2e).[6] It can be secured into place with sutures on the conjunctival end of the tube (Figure 9b). Some Jones tubes have a flexible silicone internal flange to resist extrusion.[11]
 |
 |
Figure 9. (A) Several different sizes of StopLoss Jones tubes. Image compliments of Lester Jones Tubes, www.lesterjonestube.com/ (B) Jones tube in place
The techniques for stent removal are individualized depending on the type of stent utilized. Crawford stents can be removed from either an endonasal approach or from the punctum. The endonasal approach is preferred to minimize risk of the stent breaking on removal. For the endonasal approach, the patient is asked to blow his or her nose with the head down. Once the nasal passages are cleared, the location of the stent is found within the nose, and the knot is held in place while the stent is then cut at the exposed portion between the puncta. The knot is then pulled out the nose and the cut ends of the stent freely follow, exiting the canalicular system. The approach for removing the stent from the punctum is typically used when the stent is not visualized in the nose and the stent loop is free and able to be rotated. A drop of proparacaine is placed in the ipsilateral eye. A muscle hook, finger, or needle driver is used to grasp and prolapse the stent. The stent is then rotated until the knot is visualized with fingers, forceps, or needle drivers. Once the knot is visualized, the stent is removed taking care to hold onto the knot portion of the stent so that the part of the stent without the knot is pulled through the canaliculi.
Ritleng stents are removed in a similar fashion to Crawford stents. Pigtail stents are rotated so that the knot is externalized out a punctum, the suture is cut at the knot, and the stent and suture are pulled free. The Kaneka Lacriflow stent is removed by simply pulling on the exposed stent between the puncta. Monoka stents are removed by cutting any sutures that hold the stent in place and then pulling the stent out of the punctum with forceps. Jones tubes are removed by cutting the suture that is wrapped around the tube (if one is present) and then pulling out the tube with forceps.While rare, placement of nasolacrimal stents can result in the following complications:
- Prolapse of the stent:In some cases, the stent may prolapse from its position in the medial canthus resulting in a bothersome loop of stent material protruding from the puncta. In some cases the stent can be repositioned, though stent removal may be required. A temporary fix for this complication is to tape the prolapsed loop of stent to the side of the nose.
- Damage to the puncta: Excess tension from stents may result in distortion or damage to the puncta.
- Granuloma formation
- Trauma to the canalicular system with creation of a false passage:This may be caused by probing of the canalicular system prior to stent placement or by the metal portion of the stent on insertion.
- Infection of the nasolacrimal drainage system: Infection has been recently linked to biofilm production from organisms such as nontuberculous mycobacteria.[12]
Figure 10. Various amounts of Crawford stent prolapse, (A) mild, (B) moderate, and (C) severe.
- Singh M. Lacrimal Stents and Intubation Systems: An Insight. Delhi Journal of Ophthalmology 2015;26(1):14-19.
- Henderson JW. Management of strictures of the lacrimal canaliculi with polyethylene tubes. Arch Ophthal 1950;44(2):198-203. https://pubmed.gov/15433670
- Nerad JA. Oculoplastic surgery (the requisites in ophthalmology). St. Louis: Mosby, 2001.
- Zadeng Z, Singh M, Singh U. Role of Lacrimal Canalicular Trephination and Mini-Monoka Stent in the Management of Idiopathic Distal Canalicular Obstructions: Our Experience of 23 Cases. Asia Pac J Ophthalmol (Phila) 2014;3(1):27-31. https://pubmed.gov/26107304
- Doucet TW, Hurwitz JJ. Canaliculodacryocystorhinostomy in the treatment of canalicular obstruction. Arch Ophthalmol 1982;100(2):306-309. https://pubmed.gov/7065950
- Devoto MH, Bernardini FP, de Conciliis C. Minimally invasive conjunctivodacryocystorhinostomy with Jones tube. Ophthal Plast Reconstr Surg 2006;22(4):253-255. https://pubmed.gov/16855494
- Athanasiov PA, Madge S, Kakizaki H, Selva D. A review of bypass tubes for proximal lacrimal drainage obstruction. Surv Ophthalmol 2011;56(3):252-266. https://pubmed.gov/21501738
- Jones LT. The cure of epiphora due to canalicular disorders, trauma and surgical failures on the lacrimal passages. Trans Am Acad Ophthalmol Otolaryngol 1962;66:506-524. https://pubmed.gov/14452301
- Liarakos VS, Boboridis KG, Mavrikakis E, Mavrikakis I. Management of canalicular obstructions. Curr Opin Ophthalmol 2009;20(5):395-400. https://pubmed.gov/19587600
- Silbert DI. Success rate of placement of a bicanalicular stent for partial nasolacrimal obstruction in adults under local, monitored anesthesia care and general anesthesia. Saudi J Ophthalmol 2017;31(3):140-144. https://pubmed.gov/28860910
- Jones tubes - what are they, how do they work and what's the right tube for you? . [Online publication]: Lester Jones Tubes, 2013. [Last rev. on 10/28/2017; accessed, http://www.lesterjonestube.com/].
- Samimi DB, Ediriwickrema LS, Bielory BP, Miller D, Lee W, Johnson TE. Microbiology and Biofilm Trends of Silicone Lacrimal Implants: Comparing Infected Versus Routinely Removed Stents. Ophthal Plast Reconstr Surg 2016;32(6):452-457. https://pubmed.gov/26588208

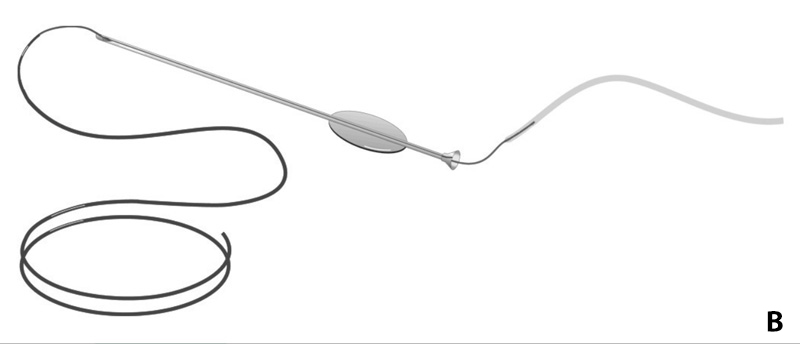

![(A) Kaneka Lacriflow stent with attached bougies, (B) Schematic of the stent demonstrating variable diameter and openings in the system [10]](Fig7a.jpg)
![(A) Kaneka Lacriflow stent with attached bougies, (B) Schematic of the stent demonstrating variable diameter and openings in the system [10]](Fig7b.jpg)