Global Causes of Preventable Blindness and Vision Impairment
Authors: Gabriel Velez, PhD; Christopher R. Fortenbach, MD, PhD; Thomas A. Oetting, MS, MD
Posted February 23, 2022
INTRODUCTION
With increasing life expectancy, many countries are seeing an increase in their average population age and a shift in disease burden towards acquired and age-related conditions. The growing and aging of populations has led to an increasing number of individuals with moderate to severe vision impairment and blindness. Many of the prevalent causes of vision loss are preventable or treatable. Thus, there is an ever-growing need to scale resources and access to eye-care professionals to preserve vision in these aging population groups. The purpose of this report is to summarize recent epidemiological studies on global blindness and provide an update on global and regional estimates of blinding eye diseases for practicing ophthalmologists and trainees.
TRENDS IN GLOBAL BLINDNESS
As of 2020, there were approximately 33.6 million cases of blindness and an estimated 206 million patients affected by near or distance vision impairment [1]. While the age-adjusted prevalence of blindness has decreased over the last 30 years, the trends for age-specific prevalence vary by etiology and severity [2]. A recent systematic review and meta-analysis by the Vision Loss Expert Group (VLEG), an international group of ophthalmologists, optometrists, and epidemiologists that curates a comprehensive online database storing world-wide ophthalmic epidemiological information, utilized data from over 500 sources to estimate the prevalence of different categories of vision impairment, with a focus on populations aged 50 and older [2]. Among this age group between 1990 and 2020, the number of global cases of moderate to severe visual impairment (MSVI) and blindness increased by 11% and 32%, respectively.
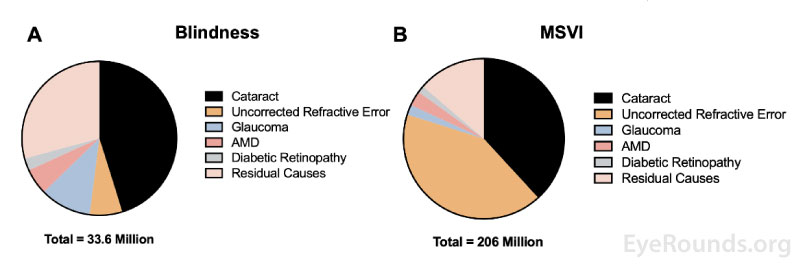
For the purposes of this report, mild vision impairment is defined as visual acuity greater than or equal to 20/63; MSVI is defined as visual acuity greater than or equal to 20/200 and less than 20/63; and blindness is defined as visual acuity less than or equal to 20/400 or less than 10 degrees of visual field around central fixation [3]. Cataract and uncorrected refractive error comprised a majority of global cases of blindness and MSVI in 2020 (Figure 1). Other prevalent causes of blindness and MSVI are summarized below.
Figure 1. Prevalence of causes of (A) blindness and (B) moderate-to-severe vision impairment (MSVI). Figure adapted from Global Disease Burden (GDB) 2019 Blindness and Vision Impairment Collaborators: Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: The Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021 Feb;9(2): e144-e160.
Uncorrected Refractive Error
Uncorrected refractive errors (e.g., myopia, hyperopia, astigmatism, and presbyopia) are important contributors to MSVI as they can be easily corrected by spectacles, contact lenses, or refractive surgery. Uncorrected refractive errors in patients aged 50 and older were responsible for approximately 86 million cases of MSVI in 2020. Uncorrected refractive error also presented the greatest burden in rural areas and low-resource regions; for example, cases of uncorrected refractive errors in India and China alone accounted for approximately 50% of global vision impairment and blindness [4, 5]. Presbyopia specifically is estimated to affect more than 1 billion individuals. Nearly half of these individuals are unable to access refractive services and spectacles to overcome their visual impairment [5]. The main strategies to address the global unmet need of uncorrected refractive errors are to increase access to refractive services and affordable spectacles, particularly in rural areas of low-resource countries [6].
Cataract
Cataracts are the largest contributor to blindness in adults aged 50 years and older [2]. According to the Global Burden of Disease, Injuries, and Risk Factors Study (GBD), there were an estimated 10.8 million individuals blind from cataracts in 2010 [7]. In 2020, there were over 15 million individuals affected, accounting for approximately 45% of global blindness. Although cataracts account for nearly 50% of blindness, the proportion varies considerably between countries and is affected by social and economic factors [8].
The cataract surgical rate (CSR) is defined as the number of cataract operations performed per million individuals in a single year and has been used by researchers as an indicator of access to eye care in each region [8]. CSR and economic indicators (e.g., gross domestic product per capital [GDP/P] and gross national income per capita [GNI/P]) are strongly associated, highlighting resource disparities and access to cataract surgery. Despite advances in cataract surgery, cataract remains the leading cause of blindness in developing countries in Sub-Saharan Africa, Latin America, and Caribbean regions [8]. For example, the proportions of cataract blindness in Paraguay and Panama are 44% and 66%, respectively, and 50% in the African and Eastern Mediterranean regions [8].
Even in highly developed countries, minorities are affected by disparities in eye care access and delivery. It is estimated that of those individuals with MSVI from cataracts in the United States, 27% are African American [8, 9]. Thus, the total burden of cataract-related blindness even in historically resource-rich countries has yet to be fully addressed.
Glaucoma
Glaucoma is the leading cause of irreversible blindness (second leading cause of overall blindness) and fourth leading cause of MSVI worldwide [2].There are an estimated 76 million individuals worldwide affected by glaucoma and nearly 3.8 million were blind as result of the disease in 2020 [2, 10]. The prevalence of primary open angle glaucoma (POAG) and primary angle closure glaucoma (PACG) in individuals aged 40 to 80 are highest in Africa and Asia, respectively [10]. The prevalence of glaucoma may, in fact, be underestimated as glaucomatous damage often goes unnoticed in early disease or may go undetected by providers in patients with dense cataracts [2]. Once detected, therapies aimed at lowering intraocular pressure can slow progression in a significant portion of cases. However, screening for glaucoma in the general population has been challenging. The two most readily accessible screening methods, visual acuity testing and tonometry, have not been shown to be useful screening techniques for the general population (e.g., patients without a known family history of glaucoma) [11]. This highlights the need for more accurate and efficient means to surveil the general population for this blinding eye disease.
Age-Related Macular Degeneration
A total of 170 million individuals are affected by age-related macular degeneration (AMD) globally. The prevalence in the United States alone is estimated to be 11 million, accounting for $4.6 billion in direct annual healthcare costs [12]. In 2020, an estimated 1.8 million patients went blind from AMD [2]. Despite this, the age-adjusted prevalence of blindness due to AMD has decreased by nearly 30% in the last three decades. This decrease has been attributed to the widespread use of anti-vascular endothelial growth factor (VEGF) therapies to treat exudative (wet) macular degeneration. However, these treatments are expensive and are not widely available to patients in Asia, Africa, and Latin America. It is estimated that two-thirds of these patients do not have access to these therapies as of 2014 [13]. Furthermore, there is still no effective treatment for non-exudative (dry) AMD or geographic atrophy. More individuals are predicted to be affected with the rapidly aging global population.
Diabetic Retinopathy
While the age-adjusted prevalence of other causes of blindness and MSVI (e.g., refractive error, cataract, glaucoma, and AMD) have decreased, the global prevalence of diabetic retinopathy (DR) has increased over the last 30 years, particularly in southern sub-Saharan Africa, east Asia, and North America [2]. It is estimated that over 100 million individuals worldwide were affected with DR in 2020, and this number is projected to increase to 160 million by 2045 [14]. Furthermore, due to the increase in life expectancy for patients living with diabetes mellitus, the rate of DR and its resulting visual impairment is expected to increase.
The management of DR requires a disproportionate number of resources compared to cataract and refractive error. Severe diabetic eye disease is often managed by ophthalmologists trained in vitreoretinal surgery [15]. These specialized providers are often scarce in low-income regions, with countries having fewer than five general ophthalmologists per 1,000 patients [15]. Thus, accurate data on the prevalence of DR is important for resource allocation, particularly with the increasing use of anti-VEGF to treat visually significant diabetic macular edema (DME).
Another concern is for the increasing prevalence in younger working populations, which has implications for the global economy. Regional policy planning should not only focus on diabetes prevention and screening, but also on the allocation of resources (e.g., intraocular anti-VEGF therapy) to low-income countries and training of ophthalmologists to manage vision-threatening DR.
Residual Causes of Vision Loss
Residual causes of vision loss encompass a wide variety of diseases including trachoma, retinopathy of prematurity, vitamin A deficiency, undiagnosed posterior pathology, and undifferentiated (idiopathic) pathology. Trachoma causes blindness through repeated conjunctival infections with Chlamydia trachomatis leading to irreversible corneal opacification. It is prevalent in areas of extreme poverty, where the infection can spread easily through flies and fomites [16]. Due to several decades of community-based interventions, such as the mass distribution of azithromycin by the International Trachoma Initiative, the prevalence of trachoma has decreased significantly [17]. The prevalence has fallen from 1.5 billion in 2002 to 142 million in 2019, a 91% decrease. There are an estimated 1.9 million individuals visually impaired from chronic trachoma infections (i.e., trachomatous trichiasis) [18].
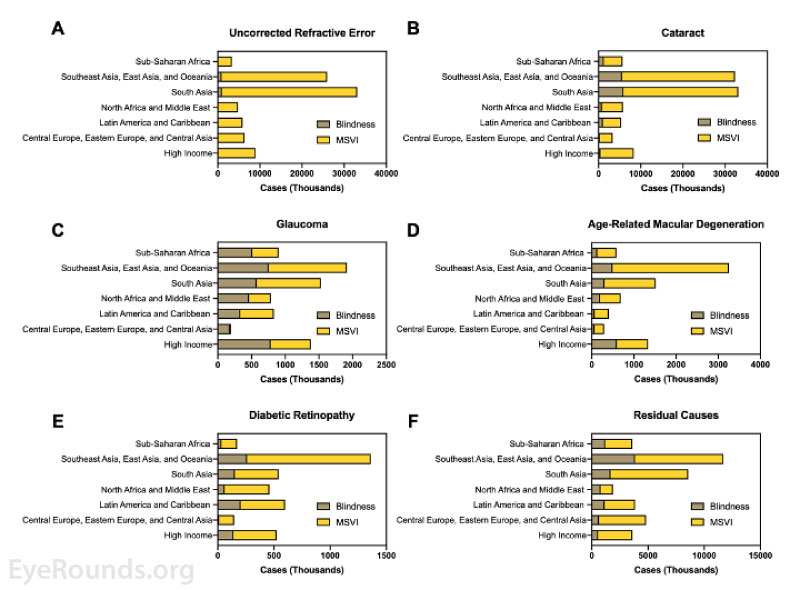
Figure 2. Regional prevalence of blindness and MSVI caused by (A) uncorrected refractive error, (B) cataract, (C) glaucoma, (D) age-related macular degeneration (E) diabetic retinopathy, and (F) residual causes (e.g., trachoma, vitamin A deficiency, etc.). Figure adapted from GBD 2019 Blindness and Vision Impairment Collaborators: Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: The Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021 Feb;9(2): e144-e160.
DISCUSSION
Despite the decrease in age-adjusted prevalence of blindness over the last three decades, global healthcare systems have not kept pace with needs. The VLEG study estimated that by 2050, 61 million people will be blind, and 474 million people will have MSVI [19]. While advances in the surgical and pharmacologic treatments have improved the management of blinding eye diseases in developed countries, newer surgical techniques and drugs are often unavailable to the general population of low-resource countries, furthering the disparity in healthcare access. For example, phacoemulsification for the treatment of cataracts leads to comparable visual outcomes and complication rates as sutureless small-incision extracapsular cataract surgery (SICS), but is far more expensive, takes longer, and requires more technological development. Thus, SICS may be a more appropriate treatment option for cataracts in the developing world [20]. Additionally, the use of anti-VEGF agents for the treatment of retinovascular diseases places a large financial and logistical burden on the strained healthcare systems in these developing countries. Bevacizumab is considerably less expensive than second generation anti-VEGF agents (e.g., aflibercept and ranibizumab) and its widespread use would widen access for patients in these regions [21].
These disparities are expected to increase with the ever-growing aging population. Therefore, global estimates of blindness and MSVI are necessary to guide the allocation of resources, providers, and interventions to better combat blindness and vision loss, particularly in developing countries.
References
- Blindness and vision impairment. Word Health Organization (WHO), 2021. [Last rev.; accessed on May 8, 2021 2021] https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment.
- Blindness GBD, Vision Impairment C, Vision Loss Expert Group of the Global Burden of Disease S. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health 2021;9(2):e144-e160. https://PubMed.gov/33275949. DOI: 10.1016/S2214-109X(20)30489-7
- Dandona L, Dandona R. Revision of visual impairment definitions in the International Statistical Classification of Diseases. BMC Med 2006;4:7. https://PubMed.gov/16539739. DOI: 10.1186/1741-7015-4-7
- Honavar SG. The burden of uncorrected refractive error. Indian J Ophthalmol 2019;67(5):577-578. https://PubMed.gov/31007210. DOI: 10.4103/ijo.IJO_762_19
- Fricke TR, Tahhan N, Resnikoff S, Papas E, Burnett A, Ho SM, Naduvilath T, Naidoo KS. Global Prevalence of Presbyopia and Vision Impairment from Uncorrected Presbyopia: Systematic Review, Meta-analysis, and Modelling. Ophthalmology 2018;125(10):1492-1499. https://PubMed.gov/29753495. DOI: 10.1016/j.ophtha.2018.04.013
- Organization WH. World report on vision. 2019.
- Khairallah M, Kahloun R, Bourne R, Limburg H, Flaxman SR, Jonas JB, Keeffe J, Leasher J, Naidoo K, Pesudovs K, Price H, White RA, Wong TY, Resnikoff S, Taylor HR, Vision Loss Expert Group of the Global Burden of Disease S. Number of People Blind or Visually Impaired by Cataract Worldwide and in World Regions, 1990 to 2010. Invest Ophthalmol Vis Sci 2015;56(11):6762-6769. https://PubMed.gov/26567788. DOI: 10.1167/iovs.15-17201
- Wang W, Yan W, Fotis K, Prasad NM, Lansingh VC, Taylor HR, Finger RP, Facciolo D, He M. Cataract Surgical Rate and Socioeconomics: A Global Study. Invest Ophthalmol Vis Sci 2016;57(14):5872-5881. https://PubMed.gov/27802517. DOI: 10.1167/iovs.16-19894
- Rao GN, Khanna R, Payal A. The global burden of cataract. Curr Opin Ophthalmol 2011;22(1):4-9. https://PubMed.gov/21107260. DOI: 10.1097/ICU.0b013e3283414fc8
- Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 2014;121(11):2081-2090. https://PubMed.gov/24974815. DOI: 10.1016/j.ophtha.2014.05.013
- Ervin AM, Boland MV, Myrowitz EH, Prince J, Hawkins B, Vollenweider D, Ward D, Suarez-Cuervo C, Robinson KA. Screening for Glaucoma: Comparative Effectiveness. Rockville (MD); 2012.
- Xu X, Wu J, Yu X, Tang Y, Tang X, Shentu X. Regional differences in the global burden of age-related macular degeneration. BMC Public Health 2020;20(1):410. https://PubMed.gov/32228540. DOI: 10.1186/s12889-020-8445-y
- Wong WL, Su X, Li X, Cheung CM, Klein R, Cheng CY, Wong TY. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health 2014;2(2):e106-116. https://PubMed.gov/25104651. DOI: 10.1016/S2214-109X(13)70145-1
- Teo ZL, Tham YC, Yan Yu MC, Chee ML, Rim TH, Cheung N, Bikbov MM, Wang YX, Tang Y, Lu Y, Hin Wong IY, Wei Ting DS, Wei Tan GS, Jonas JB, Sabanayagam C, Wong TY, Cheng CY. Global Prevalence of Diabetic Retinopathy and Projection of Burden through 2045: Systematic Review and Meta-analysis. Ophthalmology 2021;10.1016/j.ophtha.2021.04.027. https://PubMed.gov/33940045. DOI: 10.1016/j.ophtha.2021.04.027
- Teo ZL, Tham YC, Yu M, Cheng CY, Wong TY, Sabanayagam C. Do we have enough ophthalmologists to manage vision-threatening diabetic retinopathy? A global perspective. Eye (Lond) 2020;34(7):1255-1261. https://PubMed.gov/31992863. DOI: 10.1038/s41433-020-0776-5
- Mabey DC, Solomon AW, Foster A. Trachoma. Lancet 2003;362(9379):223-229. https://PubMed.gov/12885486. DOI: 10.1016/S0140-6736(03)13914-1
- Mecaskey JW, Knirsch CA, Kumaresan JA, Cook JA. The possibility of eliminating blinding trachoma. Lancet Infect Dis 2003;3(11):728-734. https://PubMed.gov/14592604. DOI: 10.1016/s1473-3099(03)00807-7
- Trachoma. World Health Organization (WHO), 2021. [Last rev.; accessed on May 23, 2021 2021] https://www.who.int/news-room/fact-sheets/detail/trachoma.
- Blindness GBD, Vision Impairment C, Vision Loss Expert Group of the Global Burden of Disease S. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. Lancet Glob Health 2021;9(2):e130-e143. https://PubMed.gov/33275950. DOI: 10.1016/S2214-109X(20)30425-3
- Ruit S, Tabin G, Chang D, Bajracharya L, Kline DC, Richheimer W, Shrestha M, Paudyal G. A prospective randomized clinical trial of phacoemulsification vs manual sutureless small-incision extracapsular cataract surgery in Nepal. Am J Ophthalmol 2007;143(1):32-38. https://PubMed.gov/17188040. DOI: 10.1016/j.ajo.2006.07.023
- Kwong TQ, Mohamed M. Anti-vascular endothelial growth factor therapies in ophthalmology: current use, controversies and the future. Br J Clin Pharmacol 2014;78(4):699-706. https://PubMed.gov/24602183. DOI: 10.1111/bcp.12371
Suggested Citation Format
Velez G, Fortenbach CR, Oetting TA. Global Causes of Preventable Blindness and Vision Impairment. EyeRounds.org. February 23, 2022. Available from https://eyerounds.org/tutorials/global-blindness/index.htm