
The University of Iowa
Department of Ophthalmology and Visual Sciences
Laser vision correction is the world's most popular elective surgery with roughly 700,000 LASIK procedures performed in the U.S. each year (AAO, 2008). Since refractive errors affect half of the U.S. population 20 years of age and older, it comes as no surprise that many people are turning to laser vision correction to obtain improved vision (Vitale et al. 2008). Due to its popularity, medical students will inevitably be asked by patients, family, and friends about refractive eye surgery. It is important to have a basic understanding of laser vision correction, outcomes, and associated risks.
The goal of laser vision correction is to decrease dependence on glasses and contact lenses by focusing light more effectively on the retina. While there are a number of different surgeries used to achieve this result, this tutorial will focus specifically on laser vision correction, which consists of laser in situ keratomileusis (LASIK) and photorefractive keratectomy (PRK). In the U.S., LASIK comprises about 85% of the laser vision correction market with PRK making up the other 15% (ISRS 2009). The cost of surgery varies in price from hundreds to thousands of dollars and is not covered by insurance, similar to cosmetic surgery.
Laser vision correction is regarded as highly effective with studies showing 94% of patients achieving uncorrected visual acuity of 20/40 or better at 12 months (Salz et al. 2002), which is the visual acuity needed to drive without corrective lenses in most states. Smaller studies have shown that up to 93% of patients with lower refractive errors can obtain 20/20 vision without correction (Stonecipher et al. 2008). A meta-analysis completed in 2008 revealed that 95% of LASIK patients are satisfied with their improved vision (Solomon et al. 2009). To better understand how these surgeries improve vision, we need to review the relevant anatomy.
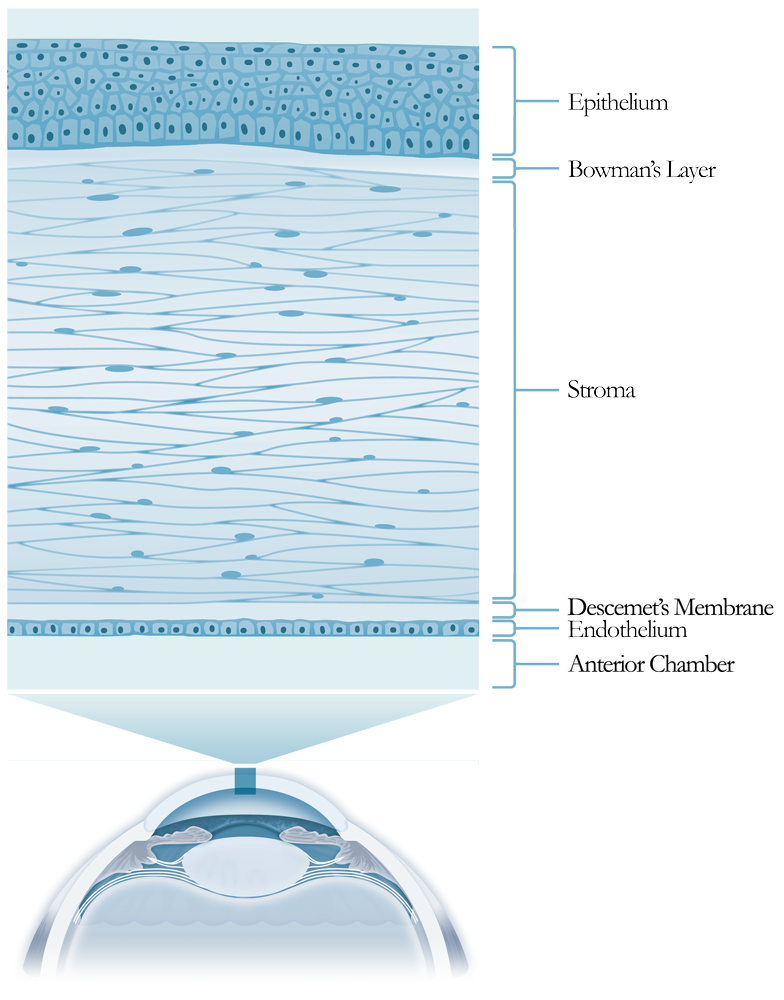
In order to see clearly, the cornea and lens must bend (refract) light rays to focus an image on the retina. The cornea is responsible for roughly 2/3 of the eye's total 60 diopters of refractive power. Unlike the lens, which is able to change its refractive power through accommodation, the cornea's curvature is fixed. The cornea is composed of 5 layers that provide a clear window and refractive power to the eye. These layers are shown in Figure 1. The stroma provides the cornea with structural shape and thus its refractive power. Laser vision correction removes stromal tissue in order to change the shape of the cornea, making it flatter or steeper.
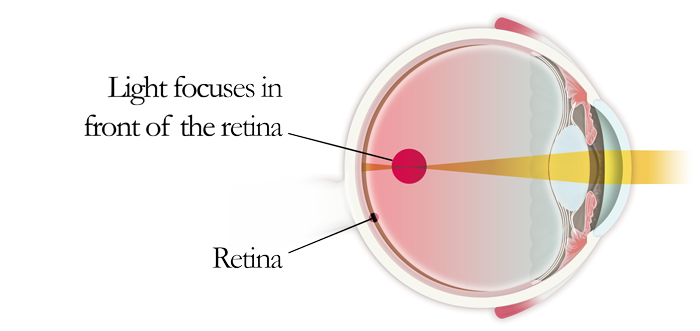
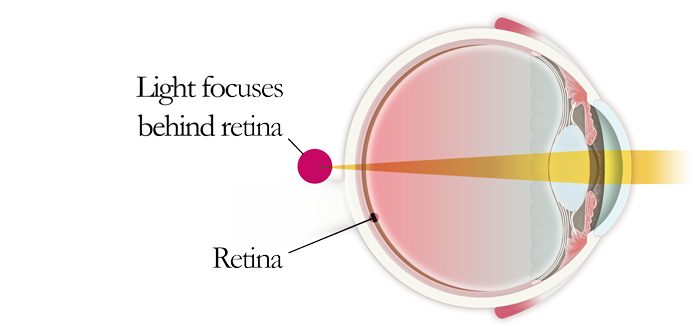
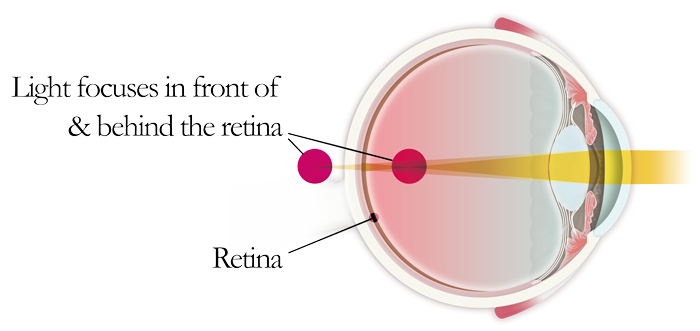
Laser vision correction is most commonly used to treat myopia (nearsightedness), hyperopia (farsightedness), and astigmatism. Figures 2, 3, and 4 illustrate these refractive errors. Depending on the refractive error, the cornea is made flatter or steeper to focus light on the retina.
In addition to corneal refractive errors, surgeons must account for presbyopia in patients who are middle aged or older. Presbyopia is the inability to focus on objects at near range due to loss of accommodation.Younger patients can accommodate, meaning they can make their relatively soft lens "thicker" to focus at near and "thinner" for distance. Presbyopia is a normal condition that typically occurs after the age of 40 and is caused by decreased lens compliance over time. With aging, the lens loses the ability to accommodate to see at near.Presbyopic patients have two options for laser vision correction: (1) Correct both eyes for distance and use reading glasses for intermediate/near work or (2) Correct one eye for distance and one eye for near (i.e., monovision) to decrease the dependence on glasses.
(Sakimoto et al. 2006, AAO 2007)
Since laser vision correction is an elective procedure, selection of the appropriate surgical candidates is paramount. Preoperative assessment begins with obtaining the patient's ophthalmic history and general medical history. Important aspects of the medical history to ask about are listed in Table 1.
| Patient History / Active Ocular Infection or Intra-ocular Inflammation |
Significance / Contraindication |
|---|---|
History of Herpes Simplex Keratitis |
A possible contraindication since application of the laser can potentially reactivate the herpes simplex virus |
Glaucoma |
A suction ring is used to hold the eye in place and elevates the intraocular pressure. However, patients with well-controlled glaucoma may be candidates. |
Keratoconus |
Contraindication due to unpredictable results |
Lifestyle/Vocation/Hobbies |
Ocular trauma can cause LASIK flap dislocation. Patients who are at higher risk for eye injuries, such as patients who play contact sports, should consider PRK instead of LASIK. |
Refraction |
Should be stable for 1 year prior to surgery. Patients under the age of 21 should wait, as their refraction may not be stable. |
Medications |
Certain medications can affect the cornea and are contraindicated for laser vision correction. (e.g., isotretinoin, amiodarone, sumatriptan) |
Pregnant or Nursing |
Women who are pregnant or nursing may have unstable refractions. Laser vision correction should be postponed until after pregnancy or for several months after nursing. |
Patient Expectations |
Patients with unrealistic expectations are not good candidates for refractive surgery. |
Systemic Immunologic Disorders |
Patients with systemic autoimmune disease, such as rheumatoid arthritis or systemic lupus erythematosus, are at risk for poor wound healing. |
A comprehensive eye exam should be performed. This should include a manifest and cycloplegic refraction, corneal topography, pachymetry, slit-lamp examination of the anterior segment, measurement of intraocular pressure, assessment for dry eye syndrome, and a dilated fundus examination (Table 2). Before the assessment, patients who wear contacts should not wear their contact lenses for at least 2 weeks (for soft contact lenses) or 4 weeks (for rigid gas permeable contact lens wearers). A contact lens holiday is necessary because contact lenses can warp or alter the shape of the cornea.
Exam |
Significance |
|---|---|
Visual Acuity and Refraction |
An accurate and stable preoperative refraction is important in determining if a patient is eligible for refractive surgery. Patients with a high amount of refractive error may not be good candidates for refractive surgery. Cycloplegic refraction eliminates the ability to accommodate yielding a more accurate refraction. |
Corneal Topography |
Laser vision correction is contraindicated in patients with irregular astigmatism and ectasia (bulging of the cornea, such as keratoconus) because these conditions may result in unpredictable refractive outcomes and worsening ectasia. |
Pachymetry |
Pachymetry is the measurement of corneal thickness. Laser vision correction reshapes the cornea by removing stroma. Only a certain amount of stromal tissue can be safely removed to ensure that the cornea remains stable in shape. Insufficient corneal thickness for the proposed ablation depth is a contraindication to laser vision correction. |
Pupillometry |
Pupil size is measured under dim and bright light. Although this is controversial, some surgeons attempt to make the treatment diameter greater than the largest pupil size to help prevent post-op glare and halos. |
Assessment for Dry Eye Syndrome |
Dry eye syndrome is a common post-operative complication after laser vision correction. Dry eye syndrome should be treated and controlled before laser vision correction. There are various methods to clinically detect dry eye syndrome, including Schirmer's tear production test. |
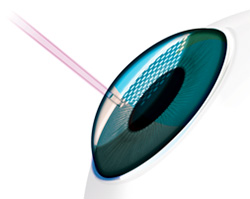
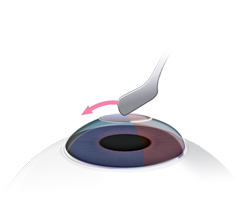
There are two main surgical techniques used to performlaser vision correction: LASIK and PRK. The major difference between these surgeries is the way in which access is gained to the anterior corneal stroma. In LASIK, a 100-200 µm corneal flap is created using a microkeratome (blade) or femtosecond laser (Sakimoto et al. 2006). In PRK, access to the stroma is gained by removing the epithelium of the cornea mechanically (by a brush or blade), chemically (i.e. with alcohol), or by laser (AAO 2007). After stroma is exposed (either by making a flap (LASIK) or by removing the epithelium (PRK)), the patient is asked to fixate on a central light. An eye-tracker is engaged to adjust for any eye movements during the ablation, and a pre-programmed excimer ablation, based on the patient's preoperative refractive error, is performed in seconds to minutes.
Patients are typically given an anxiolytic (i.e. diazepam) prior to surgery to help them relax during the procedure. To decrease infection risk and inflammation, patients generally are treated with an antibiotic drop and steroid drop for about one month after surgery. The patient is examined postoperatively at the following intervals: post-op day 1, 1 week, 1 month, 3 months, 6 months, and 1 year. Illustrations of these surgeries can be seen in Figure 5 and Figure 6.
Item |
LASIK |
PRK |
|---|---|---|
Initial examination |
Similar to PRK |
Similar to LASIK |
Procedural difference |
Corneal flap made with a microkeratome or femtosecond laser |
Surface epithelium removed by a variety of methods (blade, alcohol, brush, or laser) |
Excimer laser procedure |
Similar to PRK |
Similar to LASIK |
Postoperative discomfort |
Usually minimal |
Significant pain for the first several days postoperatively. Patients are given narcotics to control the postoperative pain. |
Visual recovery |
Starts improving at one day |
Starts to improve over the first week, but continues to improve over the first month and may take up to 3 months to achieve the final postoperative visual acuity. |
Possible Complications |
Glare/halo/ghosting |
Glare/halo/ghosting |
As mentioned previously, laser vision correction is very successful with 95% of patients satisfied with their results (Solomon et al. 2009). However, as with any surgical procedure, there is a small risk of complications (Table 4).
Complication |
Description |
|---|---|
Glare/Halos |
Seeing halos or starbursts around lights at night |
Dry Eye Syndrome |
Most common complaint after surgery. Usually relieved with the use of artificial tears. Usually resolves within weeks to months. May be persistent, especially in patients with pre-existing dry eye |
Under- or over-correction |
The goal of surgery is to achieve the desired visual result with one surgical procedure, but sometimes under-correction or over-correction may occur. In many cases, additional surgery, called an enhancement, is performed after the first surgery has healed to achieve a better result |
Flap complications |
For example, wrinkles in the flap (flap striae), hole in the middle of the flap like a donut (button hole), free flap (the flap comes completely off the cornea and does not have a hinge to attach it to rest of the cornea) |
Infection |
Rarely, infections can occur after laser vision correction |
Inflammation |
Diffuse lamellar keratitis is a type of inflammation which can occur in the first few days after LASIK surgery and requires prompt treatment with topical steroid drops and possibly re-lifting the LASIK flap depending on the degree of inflammation |
Haze |
Haze is a cloudiness of the corneal stroma that can occur in more nearsighted eyes after PRK. Most surgeons use Mitomycin C at the time of PRK in high risk patients to prevent haze formation |
Laser vision correction is an increasingly popular elective procedure that has provided improved vision to patients around the world. We hope you have gained a basic understanding from this tutorial and are more prepared to answer questions regarding laser vision correction. Listed below are additional educational resources.