
The University of Iowa
Department of Ophthalmology and Visual Sciences
February 4, 2016
Ocular ultrasound, also known as ocular echography, "echo," or a B-scan, is a quick, non-invasive test routinely used in clinical practice to assess the structural integrity and pathology of the eye. It can provide additional information not readily obtained by direct visualization of ocular tissues, and it is particularly useful in patients with pathology that prevents or obscures ophthalmoscopy (e.g., large corneal opacities, dense cataracts, or vitreous hemorrhage) (1).
Some academic centers employ a highly trained ocular ultrasonographer to perform ocular ultrasound during regular business hours. Consequently, ophthalmology residents may lack technical and practical experience in ocular ultrasound. These deficiencies are highlighted when seeing patients after hours, while on-call. Proficiency in performing ocular ultrasound is an invaluable tool to the on-call physician who seeks to quickly, safely, and inexpensively examine the globe and properly triage a patient. Please note, in the setting of a suspected open globe injury, echography should only be performed by an experienced echographer, as pressure on the eye can cause further damage. Here, we present a simple, introductory "on-call survival guide" for ophthalmology residents using ocular ultrasound.
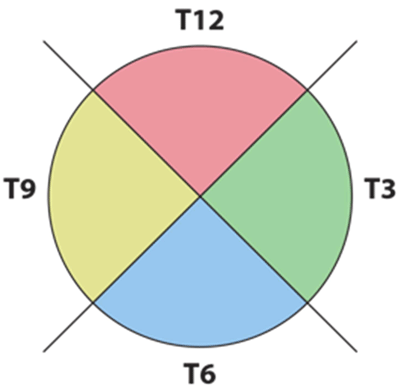
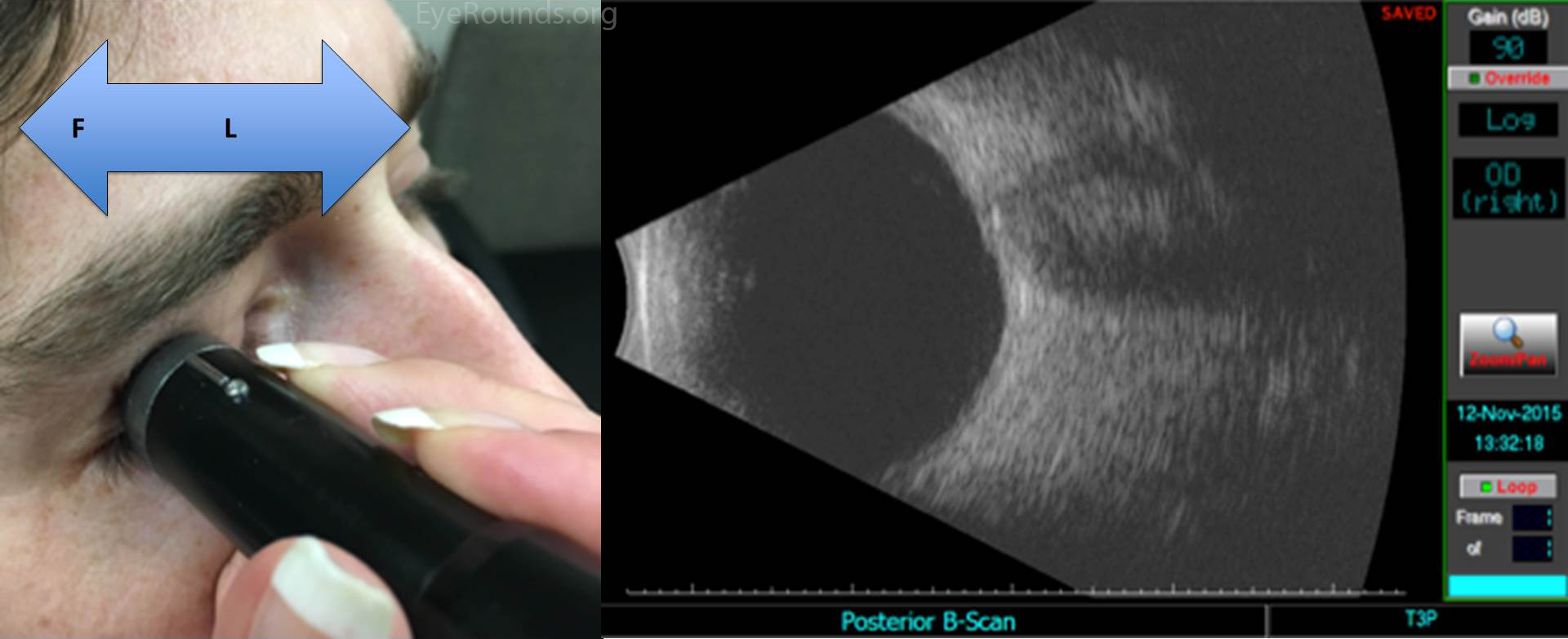
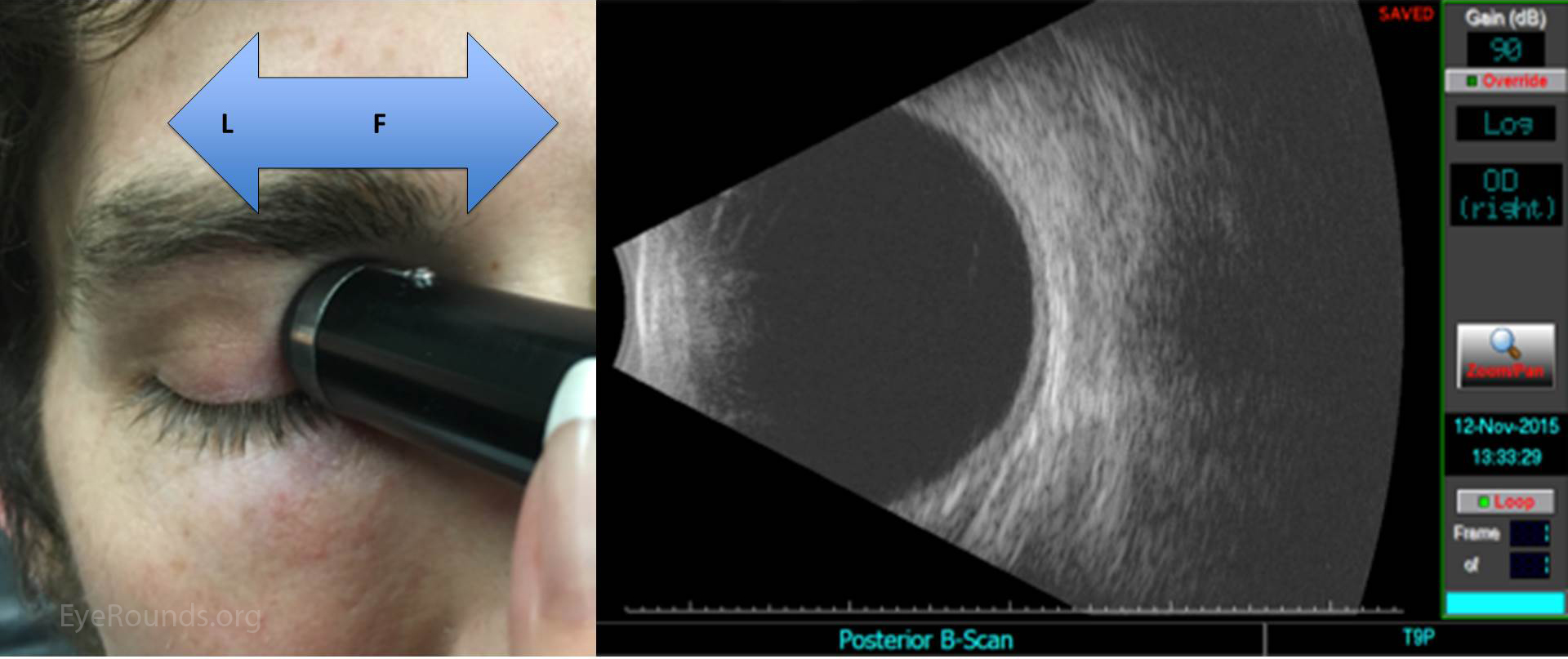
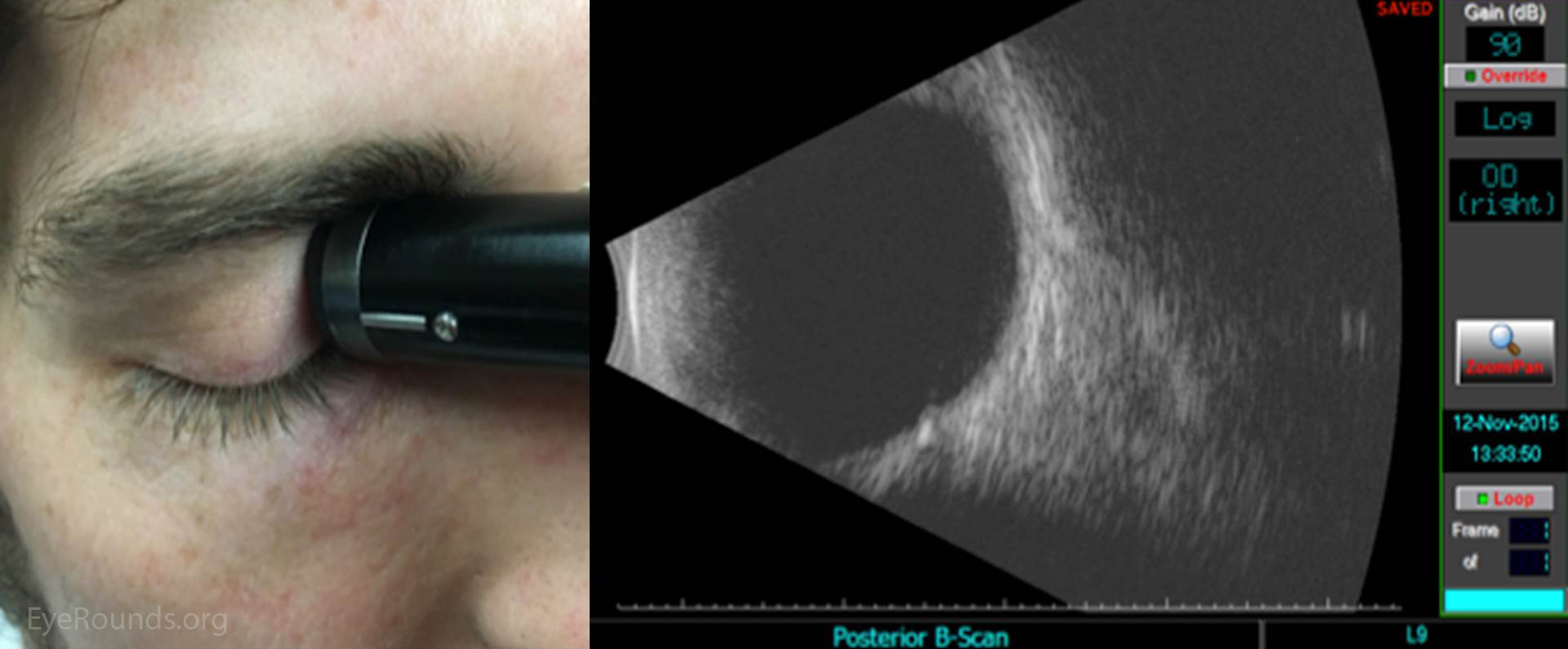
One can examine the entire globe in just five maneuvers, i.e. four dynamic quadrant views and one more static slice through the macula and optic disc, also known as longitudinal macula (LMAC). The quadrants views are designated T12, T3, T6, and T9. These numbered quadrants correspond to a clock face superimposed on the eye. For example, T12 is a view through the superior quadrant of the eye, T3 the nasal quadrant of the right eye (temporal quadrant of the left eye), and so on (Figure 1) (2).
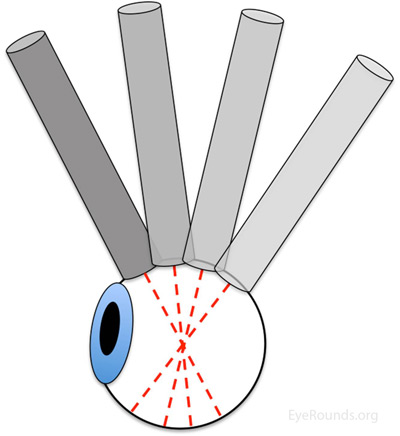
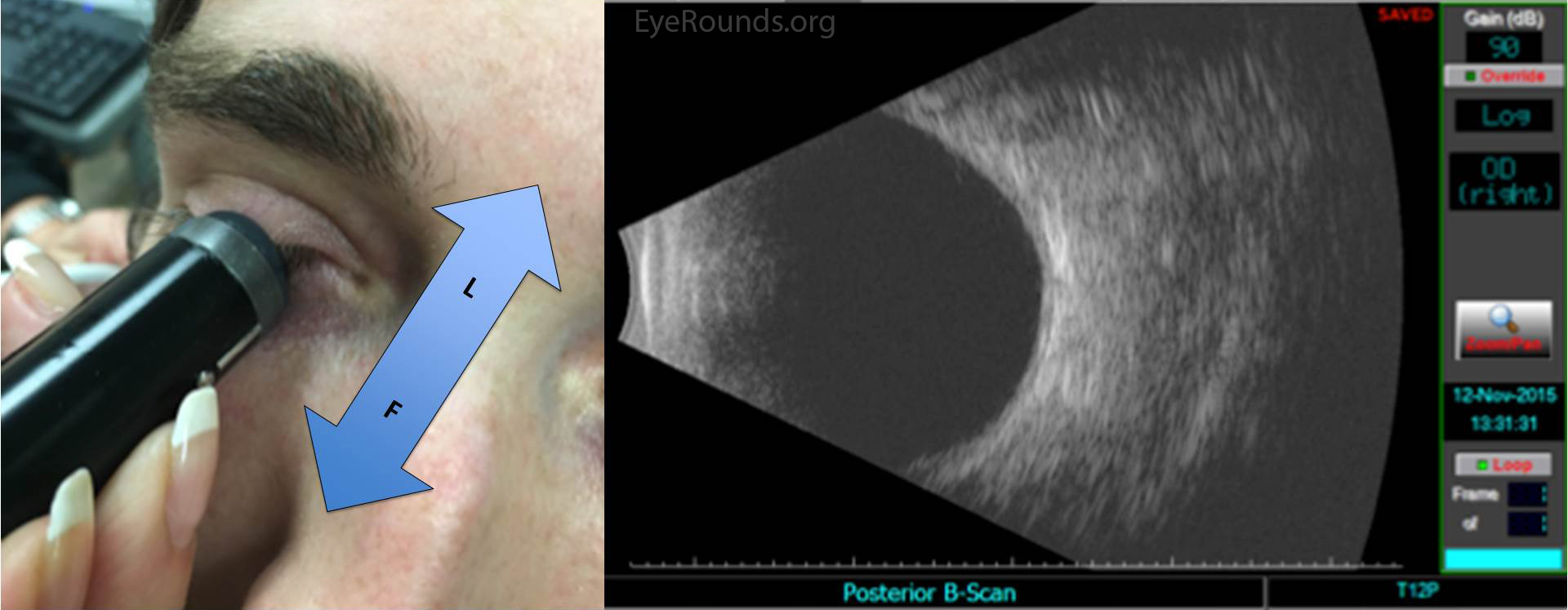
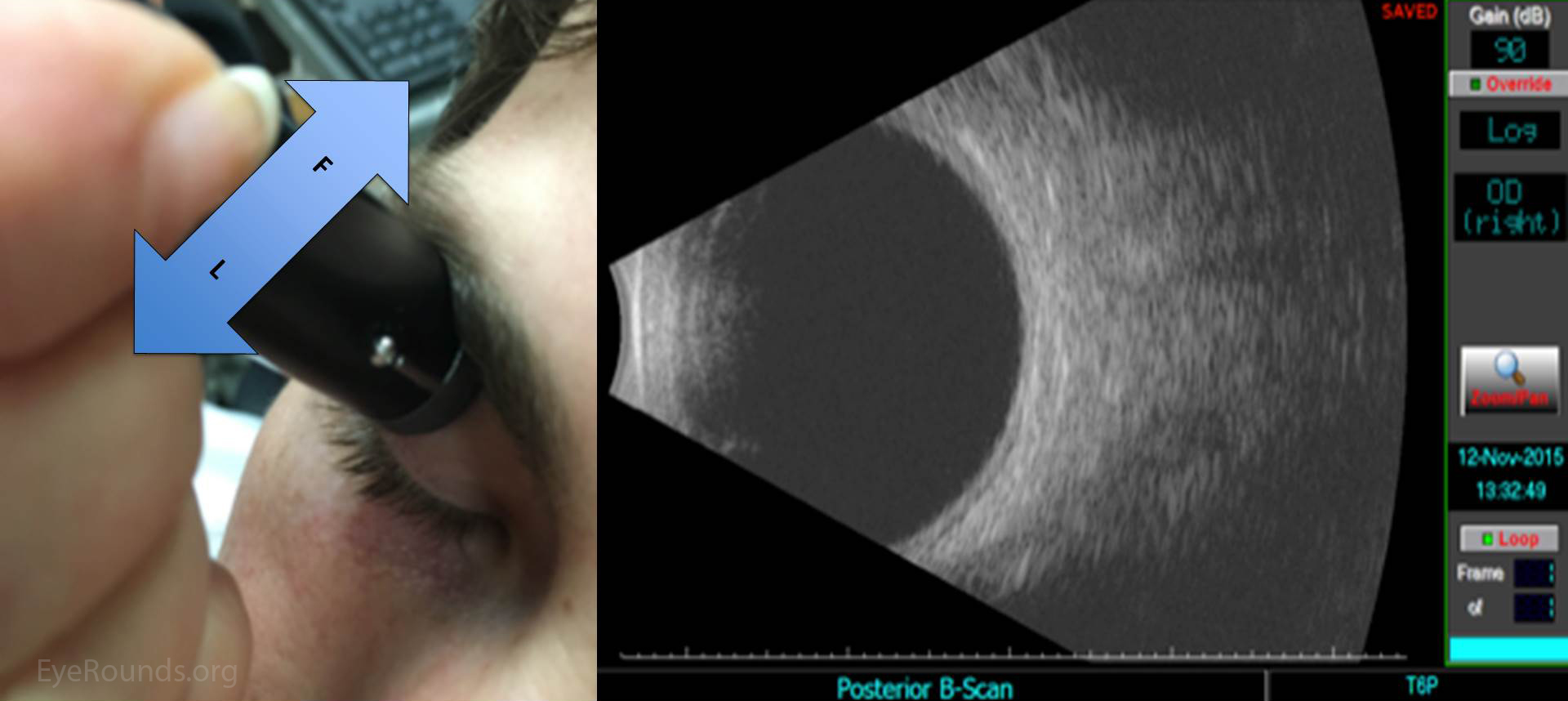
Ultrasound images can be obtained through the patient's eyelids (as depicted in this tutorial) or with the probe directly on the surface of the eye with appropriate topical anesthesia. Begin with the gain on high. The patient should look in the direction of the quadrant to be evaluated. The marker on the probe is always oriented superiorly or nasally by convention. Use a limbus-to-fornix rocking, rotational motion so that the tip of the probe moves a small distance, while the base of the probe moves a larger distance (Figure 2) (3). The probe rotates around the globe so that the sound waves always pass through the center of the eye. This rotational motion will maximize the amount of retina visualized during the scan. See the "Additional Information" section for more detail.
The on-call ophthalmologist must be proficient at ocular ultrasound, as it is an indispensible tool for the diagnosis and triage of ophthalmic emergencies. One can systematically examine the entire globe with just five maneuvers, i.e. four dynamic quadrant views and one longitudinal cut through the macula and disc. One must always remember that this is simply a starting point, and a more detailed, comprehensive ultrasound examination should be guided by additional clinical data and preliminary ultrasonographic findings.
Fairbanks A, Myers (Provencher) L, Flanary W, Warner L, Boldt HC. Ocular Ultrasound: A Quick Reference Guide for the On-Call Physician. EyeRounds.org. posted February 4, 2016; Available from: http://www.EyeRounds.org/tutorials/ultrasound/