
This 73-year-old male patient presented to the Cornea service with a one-week history of right eye redness and pain. He had a remote history of open globe with multiple subsequent penetrating keratoplasties and a recent macula-involving retinal detachment all in the right eye with resulting hand motions vision. He was diagnosed with suture-related infectious crystalline keratopathy with associated epithelialized stromal melt. The dense crystals seen within the deep stroma represent arborizing aggregates of an infectious agent, often alpha-hemolytic streptococcus or Candida albicans, and often originating from a suture track. Microbial colonies proliferate within stromal lamellar spaces and are shielded by a biofilm [1]. Corneal cultures are often negative. Lack of host inflammatory response may be due to chronic immunosuppression, tear film irregularity, or suture [2].
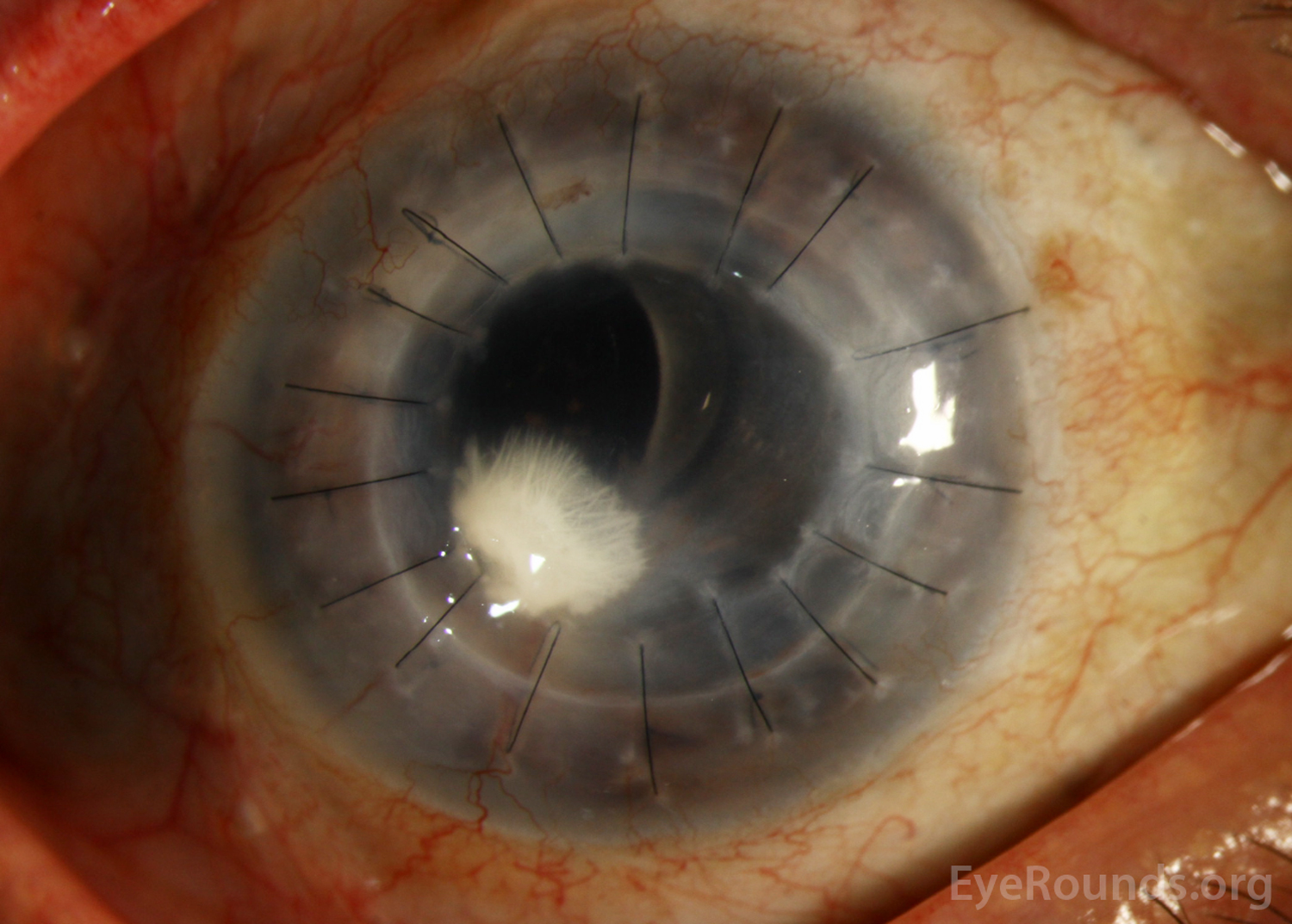
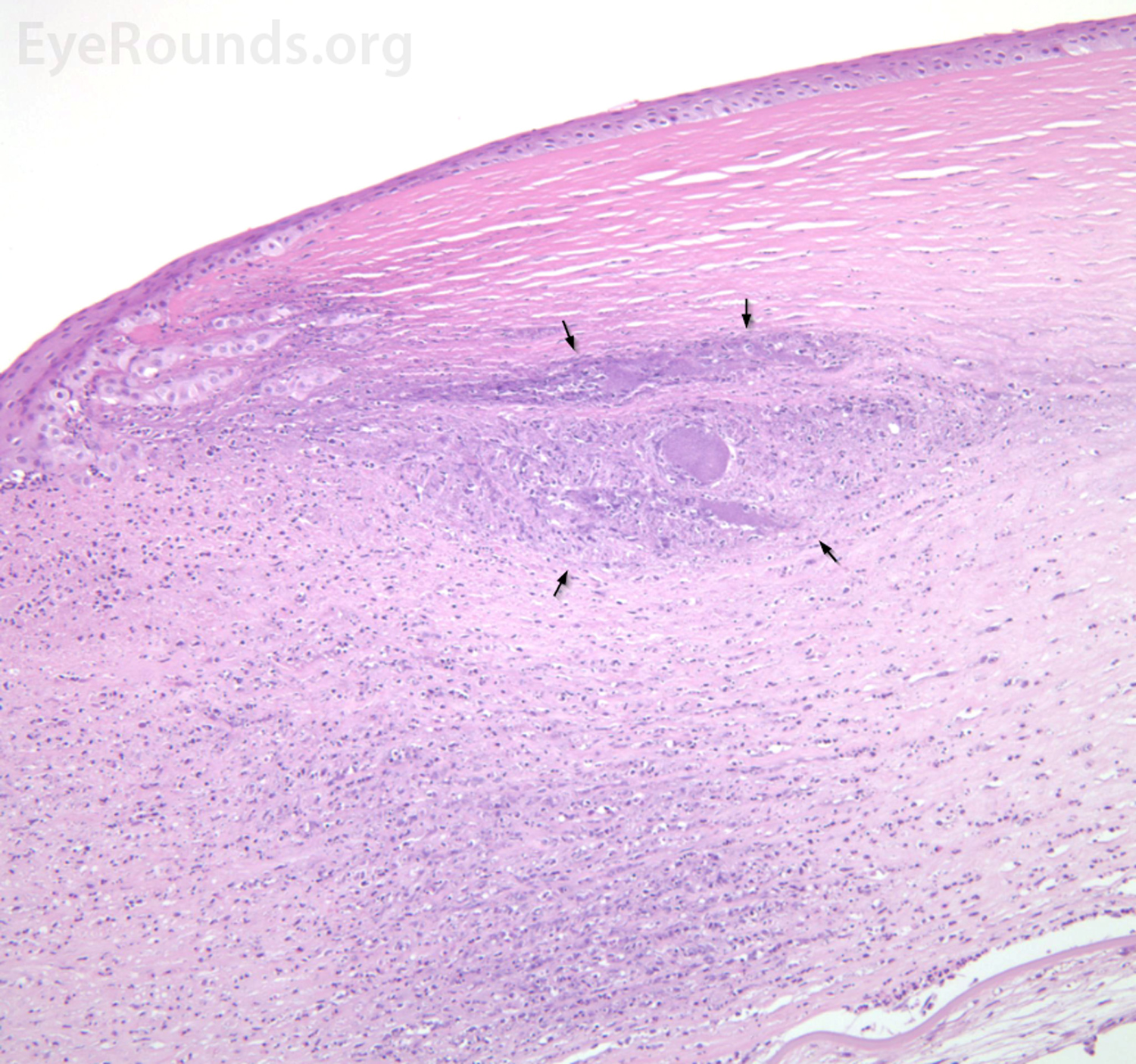

This 73-year-old male patient presented to the Cornea service with a one-week history of right eye redness and pain. He had a remote history of open globe with multiple subsequent penetrating keratoplasties and a recent macula-involving retinal detachment all in the right eye with resulting hand motions vision. He was diagnosed with suture-related infectious crystalline keratopathy with associated epithelialized stromal melt. The dense crystals seen within the deep stroma represent arborizing aggregates of an infectious agent, often alpha-hemolytic streptococcus or Candida albicans, and often originating from a suture track. Microbial colonies proliferate within stromal lamellar spaces and are shielded by a biofilm [1]. Corneal cultures are often negative. Lack of host inflammatory response may be due to chronic immunosuppression, tear film irregularity, or suture [2].
Infectious crystalline keratopathy in corneal transplant graft. Often strep viridans is the culprit.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.