Chief Complaint: Full term 2-month-old female referred to the pediatric ophthalmology clinic by the patient’s primary care provider for “poor fixation”
History of Present Illness: Mom noticed that the patient’s right eye wandered out significantly at birth but reports this has improved. Mom is uncertain if the patient sees well or not. This is the mother’s first baby.
Past Ocular History: Unremarkable
Past Medical History: Full term, normal spontaneous vaginal delivery, no pregnancy complications
Medications: None
Allergies: No known drug allergies
Family History: No known eye diseases
Physical Exam:
 |
|---|
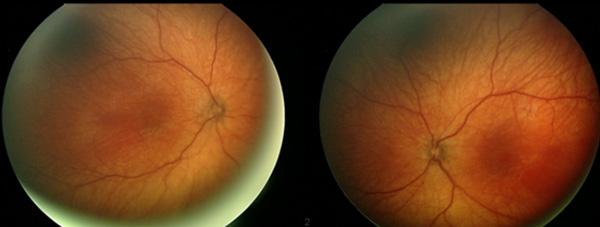
At the time of presentation, the patient had not demonstrated any growth abnormalities, seizures, or feeding difficulty. The mother also denied any acute illness or previous hospitalizations. There was no grossly visible nystagmus on exam, but the patient’s mother reported some nystagmus-like movement during feedings. Due to the concern for bilateral optic nerve hypoplasia, the guarded visual prognosis as well as the need for a well-coordinated, collaborative approach to this patient’s evaluation and management was discussed with the patient’s mother. The patient was referred for a brain MRI to assess for any midline central nervous system abnormalities as well as pediatric neuro-ophthalmology and pediatric endocrinology.
The optic nerve forms around 6 weeks gestation in human embryos with extension of the optic nerve fibers to the chiasm by 8 weeks gestation (Billson, 1986). Embryologic development of the corpus callosum and septum pellucidum occurs roughly at the same time as the optic nerve; therefore, midline central nervous system abnormalities are increased in patients with optic nerve hypoplasia. When optic nerve hypoplasia occurs with an absence of the septum pellucidum, it is known as septo-optic dysplasia or eponymously “de Morsier syndrome.” Only about 10% of children with optic nerve hypoplasia have septo-optic dysplasia, and about 50% of these children have associated endocrine abnormalities with the possibility of potentially fatal endocrine complications secondary to thermoregulation problems, dehydration, and congenital hypothyroidism (2, 3). Please see EyeRounds.org/cases/138-UnilateralOpticNerveHypoplasia.htm for further discussion on the diagnosis of optic nerve hypoplasia as well as the systemic findings and/or endocrine abnormalities that can be associated with this exam finding.
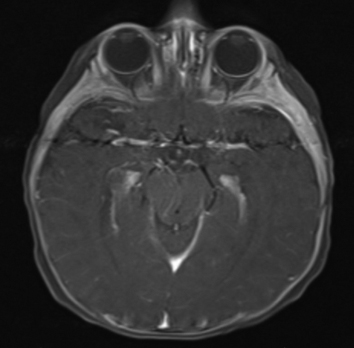
Approximately one month later, the patient underwent a brain MRI (Figure 2) with findings consistent with bilateral optic nerve hypoplasia and with panhypopituitarism. No midline anomalies were identified. Therefore, the patient was urgently referred to pediatric endocrinology.
 |
 |
|---|
Coordination of care is critical in the initial evaluation of many ophthalmic patients, and in particular, pediatric patients. Although not primary care physicians, ophthalmologists are often the initial point of care in diagnosing disorders with a variety of systemic manifestations, and therefore responsible for ensuring that patients obtain the appropriate referrals to address their systemic disease. In this case, the patient was referred for an MRI which showed findings concerning for panhypopituitarism. Due to this finding, there was concern that the patient could be at risk for fatal endocrine complications such as thermoregulation problems, dehydration, or other stress hormone-related problems. A call was placed immediately to pediatric endocrinology for an urgent consultation as soon as the MRI findings were discovered. The pediatric endocrinologist spoke with the patient’s mother and arranged for an appointment in the pediatric endocrinology clinic the next day. The patient was also seen by pediatric neuro-ophthalmology within the week.
The pediatric endocrinology team found that she had a neonatal history of hypoglycemia. Labs including: basic chemistry panel, urinalysis (to look for diabetes insipidus), free T4 (to rule out central hypothyroidism), ACTH/cortisol, and IGF-1 (to screen for growth hormone deficiency) were performed. Labs returned consistent with low-normal free T4 and low-normal cortisol levels. The patient was subsequently started on oral hydrocortisone 2.5 mg twice daily (and was instructed to increase the dose to 7.5 mg three times daily with onset of any acute illness). Two weeks later, she was started on levothyroxine 25 mcg per day with the plan to repeat her labs in 3 months. The family was also given instructions on how to manage the patient’s hydrocortisone if she has a procedure or sedation (25 mg hydrocortisone IV).
In conclusion, coordinated, collaborative care is crucial in the field of ophthalmology and in particular, in patients with optic nerve hypoplasia to avoid endocrine crisis.
Bilateral optic nerve hypoplasia with borderline achiasmia with mild endocrine deficiencies (cortisol, thyroid)
Baker MS, Longmuir SQ. 2-month-old with bilateral optic nerve hypoplasia: highlighting the importance of a multi-disciplinary approach. EyeRounds.org. May 18, 2012, Available from: https://eyerounds.org/cases/149-bilateral-optic-nerve-hypoplasia.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.