Chief Complaint: Decreased vision in the right eye after a BB gun injury
History of Present Illness: An 18-year-old male with no past ocular history presented to the Emergency Treatment Center at the University of Iowa Hospitals and Clinics (UIHC) after being shot in the right orbit with a BB gun at a distance of around 5 feet one day prior. The patient was not wearing safety glasses at the time of the injury. He noted an immediate decrease in vision after the gunshot, after which he rinsed the eye with artificial tears and went to bed. Upon awakening the next morning the eye was red, watery, irritated, and he noted tenderness of the right eye with far left gaze. His vision continued to be reduced in the right eye. He presented to an outside hospital where computed tomography (CT) was performed and the patient was emergently transferred to UIHC for further evaluation of decreased vision in the right eye.
Medications: None
Family History: Non-contributory
Social History: No tobacco or alcohol use
Review of Systems: All systems negative, except as noted above
Visual acuity (without correction):
Intraocular pressure (IOP) by Tonopen:
Confrontation Visual Fields:
Motility:
Pupils:
Lids/Lashes:
Conjunctiva/Sclera: (Figure 1)
Cornea:
Anterior chamber:
Iris:
Lens:
Vitreous:
Disc:
- OD: Small hemorrhage on the disc temporally, whitening of peripapillary retina, no optic nerve edema
- OS: Normal
Macula:
- OD: Diffuse retinal whitening with poor foveal reflex
- OS: Normal
Vessels:
- OD: Pre-retinal hemorrhage along inferior arcade
- OS: Normal
Periphery:
- OD: Broad area of deep whitening consistent with bare sclera inferonasally at 4:00 in the mid-periphery with associated intraretinal and pre-retinal heme, extensive retinal whitening nasally as well as temporally, no holes or tears OS: Normal
Figure 2. Fundus
CT orbit: Fracture of the medial orbital wall with soft tissue swelling and intraorbital air. Hyperdense round object (consistent with BB pellet) resting in the sphenoid sinus (Figure 3). No intraocular foreign body.
B-scan echography: Retina attached, no intraocular foreign body.
Figure 3. CT Scan.
The patient was initially treated with scopolamine drops twice daily and prednisolone acetate 1% every 2 hours in the right. After 10 days, the scopolamine drops were discontinued and the patient was tapered off the prednisolone drops. The patient was noted on follow-up to have nasal and temporal angle recession on gonioscopy. He was fitted with polycarbonate lenses for monocular precautions and was closely followed to monitor for retinal tears (though these are uncommon in this setting) and elevated IOP. His best corrected visual acuity OD slowly improved from counting fingers to 20/60-2 at 6 weeks after the injury. Vision was felt to be limited due to traumatic optic neuropathy and commotio retinae.
The term sclopetaria may originate from the old English word “sclow” which means to claw or tear, or from the Latin word “sclopetum” which was a Roman gun. When a high-velocity projectile such as a BB passes adjacent to the globe, there are direct and indirect shock wave forces which can lead to simultaneous retraction of the choroid and retina leaving an area of bare sclera at the site of the break. Immediately after the injury, there is usually extensive intraocular hemorrhage, with subretinal, intraretinal, and vitreous hemorrhage, with large overlying retinal breaks. The hemorrhage resorbs and organizes, leaving extensive fibrous proliferation that seems to fuse the retina and the choroid. The lesion has irregular borders, sometimes with a claw-like configuration. Due to significant post-traumatic fibrovascular proliferation and scar formation, there is very low risk of retinal detachment after injury (1).
Each year in the United States (US) there are at least 2 million eye injuries that require medical treatment (2). Nearly 1 million Americans have significant visual impairment from an eye injury and over 75% of these individuals are considered monocularly blind. Eye injury is second only to cataract as the leading cause of monocular blindness in the US (3). Ocular trauma is the number one cause of non-congenital unilateral blindness and monocular disability in children (4).
While around 2000 U.S. workers will sustain an eye injury each day on the job, the home has become an increasingly common location to sustain an injury and currently accounts for over 44% of all eye injuries. In addition, over 40% of eye injuries are related to sports or recreational activities (5). Males are more likely than females to sustain an ocular injury, by a rate of 2- 7.3 to 1. The peak age of injury is around 20 years old with 35% of ocular injuries occurring at 17 years of age or younger (6).
In a large study of emergency department-treated eye injuries the most common type of injury (Figure 4) was contusion or abrasion (44.4%) followed by foreign body (30.8%), burn (10.2%), conjunctivitis (9.9%), laceration (1.8%) and puncture wound (0.5%).
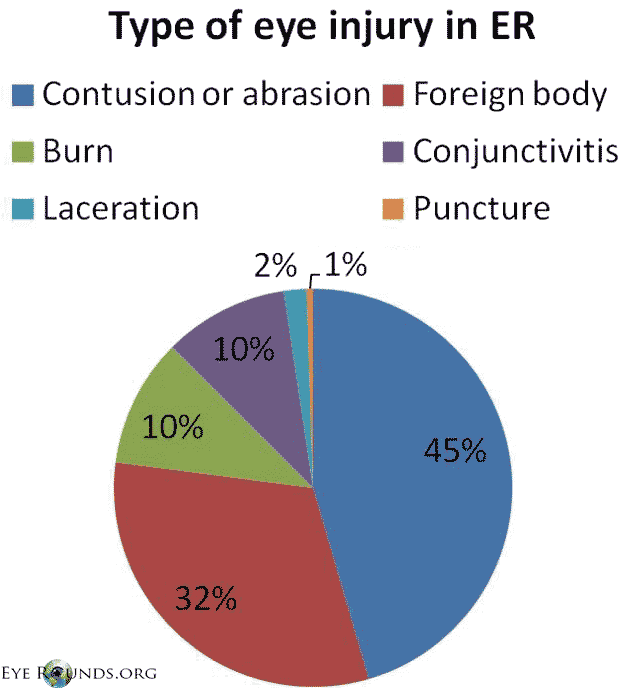
Figure 4. Type of Eye injury in ER
The most common mechanisms of injury (Figure 5) were foreign body (44.6%), being struck by an object (33%), burns (12%), machinery (3.1%), motor vehicle crashes (2.3%) and falls (1.8%) (7).
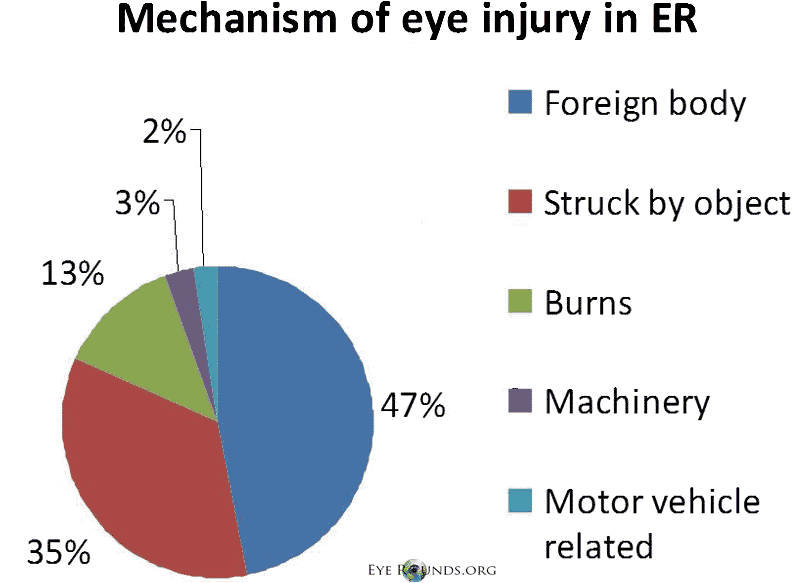
Figure 5. Mechanism of Eye injury in ER
In a study of work-related eye injury the most common activities associated with eye injury (Figure 6) were welding (30.4%), drilling/cutting (13.4%), splashing of chemicals (11.7%), hammering (10.2%), equipment cleaning/maintenance (7.1%), mowing (6.4%) and grinding (6.0%).
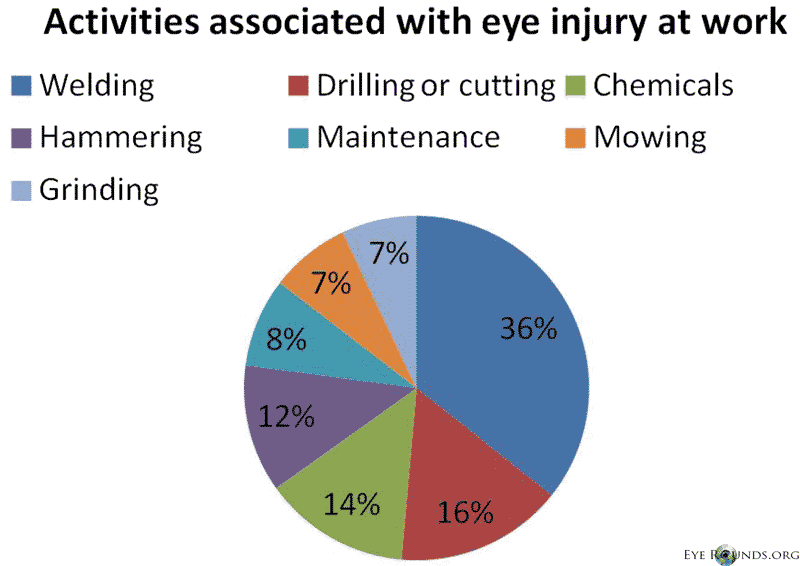
Figure 6. Activities assciated with eye injury at work
The type of injuries (Figure 7) included photokeratitis (33.2%), eyeball laceration/penetration (22.3%), chemical burn (14.1%), corneal abrasion/foreign body (12.4%), ocular adnexa injury (9.2%), blunt trauma (4.9%) and scalding burn (3.9%) (8).
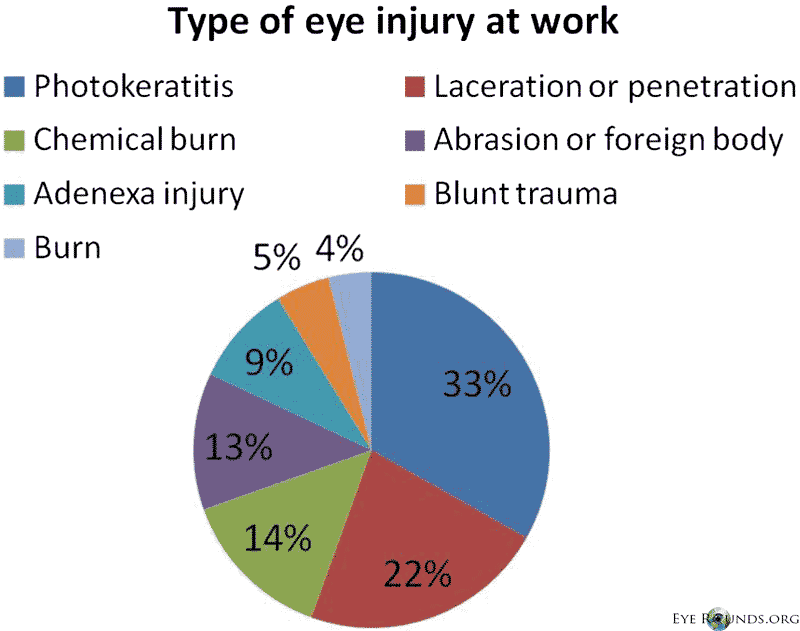
Figure 7. Type of eye injury at work
It has been estimated that over 90% of eye injuries could have been prevented or decreased in severity with increased education, use of safety equipment, and limiting known risk factors of certain activities (9). There is a strong correlation with occupational eye injury and lack of protective eyewear (10) and only approximately 18% of injured workers were found to be wearing protective eyewear at the time of injury (8). A review of eye injury prevention literature demonstrates that while research has been effective in understanding the mechanisms of injury and barriers to use of protective eyewear, very little is known about the success of education and prevention programs (11). Two exceptional examples in athletics provide a model for future programs. When the Canadian Amateur Hockey Association recognized that over two-thirds of player injuries included the face and eye, they began requiring the use of full-face protective devices in 1981. The incidence of eye injury in hockey fell from 257 in 1974 to zero in 1983 (12). Given the high incidence of eye injury in little league baseball, facemasks were introduced optionally to helmets in 1984. In a study of 4,233 little league baseball players, the use of softer and more deformable safety balls was associated with decreased ball-related injury (adjusted rate ratio, 0.77) and the use of faceguards resulted in decreased facial injury (adjusted rate ratio, 0.65) (13).
There are a number of recommendations for eye injury prevention for work, home and recreation activities. The American Academy of Ophthalmology (AAO) provides a comprehensive website at www.geteyesmart.org/eyesmart/living/preventing-eye-injuries.cfm. Risks of eye injury at home include use of household chemicals, hot grease splashes while cooking food, opening champagne bottles, drilling or hammering, falls, and projectiles while mowing or weed-eating. Every home should have at least one pair of approved protective eyewear to be used in high-risk situations. In addition, in patients with an elevated fall risk, cushioning of sharp corners and handrails can limit injury. At work, injuries commonly occur from flying particles, tools and chemicals, and the most important recommendation is for 100% full-time use of protective eyewear in these situations. It is also known that eye injuries are more common when performing unfamiliar tasks or during periods of fatigue. It is recommended that when working with flying particles or dust the protective glasses should have side shields, and goggles are necessary to prevent injury from chemicals and volatile gasses.
Children are most often at risk of eye injury during athletics or recreation, and polycarbonate lenses are recommended for all major sports including baseball, basketball, football, racquet sports, soccer, etc. Supervision is suggested when children are using pencils, rubber bands, paper clips, scissors or bungee cords. Children should avoid projectile toys such as arrows and darts and should never be allowed to use BB guns, pellet guns, potato guns, lawn darts or fireworks. Dog bites cause eye injury in 15% of cases, and because the second bite is often likely to be more serious if not fatal, the physician should always advocate for the removal or euthanization of a biting dog.
In order to decrease the incidence of eye injuries at a systems level, awareness and patient education are the first and most important steps. On hospital-wide level, we have created an eye injury prevention screen saver which displays hospital-wide to raise awareness of the prevalence of eye injury and tips for prevention. This was displayed in the month of July, in observance of “Eye Injury Prevention Month,” as designated by the AAO. On an individual level, we stress the importance of eye protection and monocular precautions with our patients regularly.
Additionally, in this article, we hope to consolidate the available resources for patients and eyecare providers:
The following links provide more information for eye injury prevention:
Welder JD, Kemp PS, Boldt HC, Kitzmann AS. Chorioretinitis Sclopetaria: A Systems Based Approach to Eye Injury Prevention. EyeRounds.org. August 21, 2013; available from https://eyerounds.org/cases/175-sclopetaria-chorioretinitis.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.