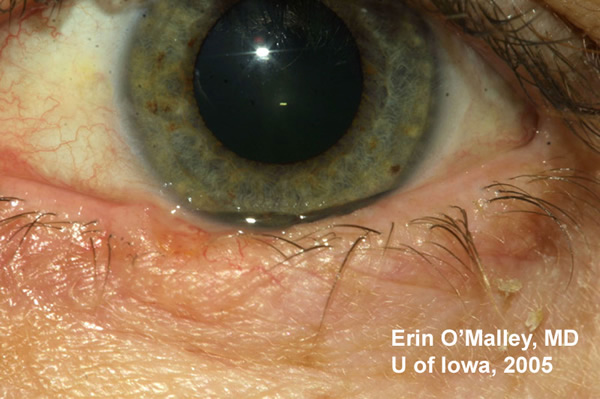
Chief Complaint: 49-year-old Caucasian female with a lesion on her left lower lid.
History of Present Illness: The patient noted that the lesion has been present for 2 years. She states that it occasionally gets inflamed, and then heals but it always comes back. She has not noted any change in size of the lesion during that time.
Ocular History: No previous ocular history. No eye surgery nor eye trauma.
Medical History: Hypothyroidism.
Medications: Levothyroxine
Family and Social History: Noncontributory. Patient is a non-smoker and occasional consumes alcohol.
 |
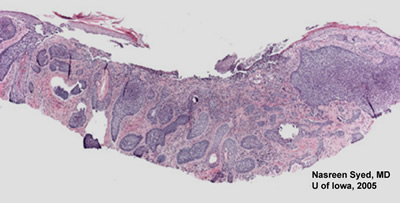
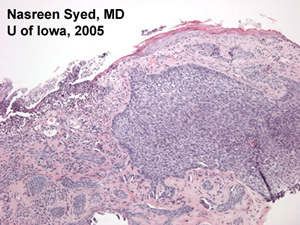
Course: An excisional biopsy was performed (see Figures 2 and 3) which demonstrated skin with central ulceration of the epidermis and multiple islands of basophilic neoplastic cells in the superficial dermis. The neoplastic cells appear to arise from surface epidermis. The diagnosis was consistent with basal cell carcinoma. Mohs surgery with oculoplastic reconstruction was planned.
 |
 |
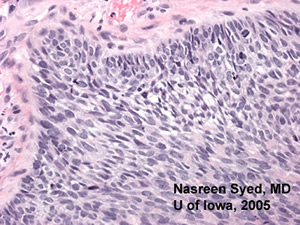 |
| Figure 3A: A 50x magnification demonstrating the neoplastic cells arising from surface epidermis. | Figure 3B: A 200x magnification demonstrating the pallisading quality to the borders of nests of neoplastic cells. |
Basal cell carcinoma is the most common malignancy of eyelids (90% of eyelid malignancies). Risk factors include exposure to sunlight and the patient may have a history of other skin cancers. Classically the lesion appears as a slowly enlarging ulceration with raised, pearly borders. There are multiple forms that this malignancy can take including nodular (as is this case), morpheaform (see EyeRounds Case #7), pigmented, and multicentric. The lower lid is most commonly involved, followed by the medial canthus and less frequently the upper lid and lateral canthus. Lesions involving the medial canthus are often more deeply invasive. Metastasis is rare with basal cell carcinoma, however these lesions may be deeply invasive and therefore clear surgical margins are extremely important.
The diagnosis is made with biopsy. On pathology, the tumor cells form cohesive nests of cells with bland appearing nuclei with nuclear palisading of the peripheral cell layer. The malignant cells originate from the basal layer of epidermis and only occur in hair bearing tissue. Tissue processing can cause artifactitious separation of tumor from surrounding stroma.
Treatment is with complete surgical excision. Mohs micrographic surgery is a technique described by Dr Frederic Mohs (1910-2002) from the University of Wisconsin. The goal of Mohs surgery is to remove all of the cancer while sparing the most amount of healthy tissue. He initially utilized fixed tissue and in the 1960s used fresh frozen tissue. The frozen tissue technique was first described for basal cell carcinoma of the eyelid. In Mohs surgery, first the visible tumor is removed. Next, thin, horizontal sections through tumor margins are examined under the microscope. Any microscopic "roots" of tumor are mapped to the original tissue and re-excised. This process is repeated as necessary until no tumor remains.
 |
In the patient above, Mohs surgery left a defect that was 4 X 12mm, deep to the tarsus (see Figure 4). Oculoplastics planned a myocutaneous advancement flap and free tarsal graft from the right upper lid for repair.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
O'Malley EM, Nerad JA, Syed NA. Nodular Basal Cell Carcinoma: 49-year-old female with left lower lid lesion. EyeRounds.org. August 24, 2005; Available from: http://www.EyeRounds.org/cases/44-Nodular-Basal-Cell-Carcinoma-BCC.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.