
The University of Iowa
Department of Ophthalmology and Visual Sciences
Patient expectations for cataract surgery have increased significantly over the past several decades as surgeons have transitioned from standard extracapsular techniques to clear-cornea phacoemulsification. In addition to short operating times, topical anesthesia, and a sutureless procedure, patients increasingly expect spectacle independence following cataract extraction. In this tutorial we present the case of a 59-year-old male with a visually-significant cataract and consider the intraoperative management of astigmatism in a representative case of an individual with small-to-moderate cylindrical error.
Presbyopia correction is discussed separately in a tutorial entitiled "Intraocular lenses for presbyopia" by Tim Johnson, MD, PhD.
OD: -1.50 sphere
OS: -1.50 + 0.75 x 110
OD: 20/20
OS: 20/50
During the preoperative visit the patient indicated his desire for spectacle independence following surgery.
The surgeon has a number of options for the interaoperative management of astigmatism, including:
Peripheral corneal relaxing incisions (PCRI) or the slightly more peripheral limbal relaxing incisions (LRIs) can flatten astigmatism as an adjunct to cataract surgery (Osher 1984, Budak 1998). LRI's have been demonstrated to predictably alter the corneal curvature by flattening the cornea in the meridian in which they are placed and allowing for a commensurate amount of steepening 90 degrees away. A number of nomograms are available to determine the arc length and number of incisions for a certain amount and axis of astigmatism, such as the Donnenfeld nomogram (http://www.lricalculator.com). In addition to the degree of astigmatic correction desired, nomograms often take into account age, the distance the incisions are placed from the limbus, and corneal thickness. Limbal relaxing incisions have several strong points: the procedure is fast and easy to perform; the results are highly predictable and reproducible; and the technology is inexpensive. Incisions can be placed with a diamond knife, multi-use and single-use steel blades, and more recently with the femtosecond laser. LRIs are a great option in patients with pre-existing astigmatism who desire presbyopia correction with a multifocal or accommodating IOL as toric versions of these lenses are not FDA-approved at present. LRIs should be used with caution in patients with corneal ectasia, peripheral thinning, and advanced dry eye especially when associated with rheumatoid disease.
The first toric intraocular lens model was approved by the FDA in 1998. Widespread use of toric IOLs would not come until later, however, with approval of a foldable toric IOL in September 2005. Toric IOLs have the advantage of being able to correct large amounts of astigmatism. The most common toric IOL used in the US is the single piece acrylic (SPA) design, which is more stable than the earlier silicon plate haptic models (Chang 1998, 2009, 2003). Alcon has published a web site for their toric IOL calculation which is very useful and takes into account induced astigmatism from the wound (http://www.acrysoftoriccalculator.com). Click here to see a video of toric IOL marking and placement.
Drawbacks of the toric IOL include its cost and the potential for instability of the corneal astigmatism or possible rotation of the lens in the years following surgery. Pineda studied the cost of the toric IOL over a patient s life and determined that it may actually save money by reducing spectacle and contact lens expenditures (Pineda 2010). Corneal topography can change over time, raising the question of whether an axis shift down the road e.g. in a young individual, a patient with keratoconus, or a post keratoplasty patient could turn the cylindrical component of the IOL correction into a liability. One might be reluctant to implant a toric intraocular lens in a patient with a traumatic cataract, pseudoexfoliation syndrome, retinitis pigmentosa, or any other condition predisposing to loose zonules. Irregular astigmatism is not corrected with a toric lens and the toric IOL can make placement of a contact lens to treat the irregular astigmatism difficult.
Two recent studies have compared toric intraocular lens placement to peripheral corneal relaxing incisions for correction of astigmatism during cataract surgery. One study by Poll, et al found the two strategies to yield comparable results with mild-to-moderate astigmstism (Poll 2011). The toric IOL was favored for higher degrees of astigmatism. In a second study, Mingo-Botin, et al found that toric IOL implantation was more effective and predictable between 1.00 and 3.00 diopters of preexisting astigmatism (Mingo-Bot n 2010). Many surgeons consistently obtain excellent results with both of these strategies.
A third strategy for astigmatism management is to correct astigmatism postoperatively with an excimer laser. In appropriate candidates excimer ablation is safe and highly effective. An advantage of this approach is that residual spherical error can also be addressed by the ablation further refining the refractive outcome. Relative to the other strategies, cost remains the primary barrier to more widespread adoption of this approach.
Small amounts of astigmatism can be managed by placing the surgical wound to coincide with the steep axis of astigmatism. It may be difficult to operate along some axes, particularly if the patient is relatively enophthalmic or has a large brow or nose bridge. Only about 0.50 diopters of astigmatism can be relaxed with a typical clear corneal incision. Some surgeons performing microincisional phaco may not induce any astigmatism with their incision.
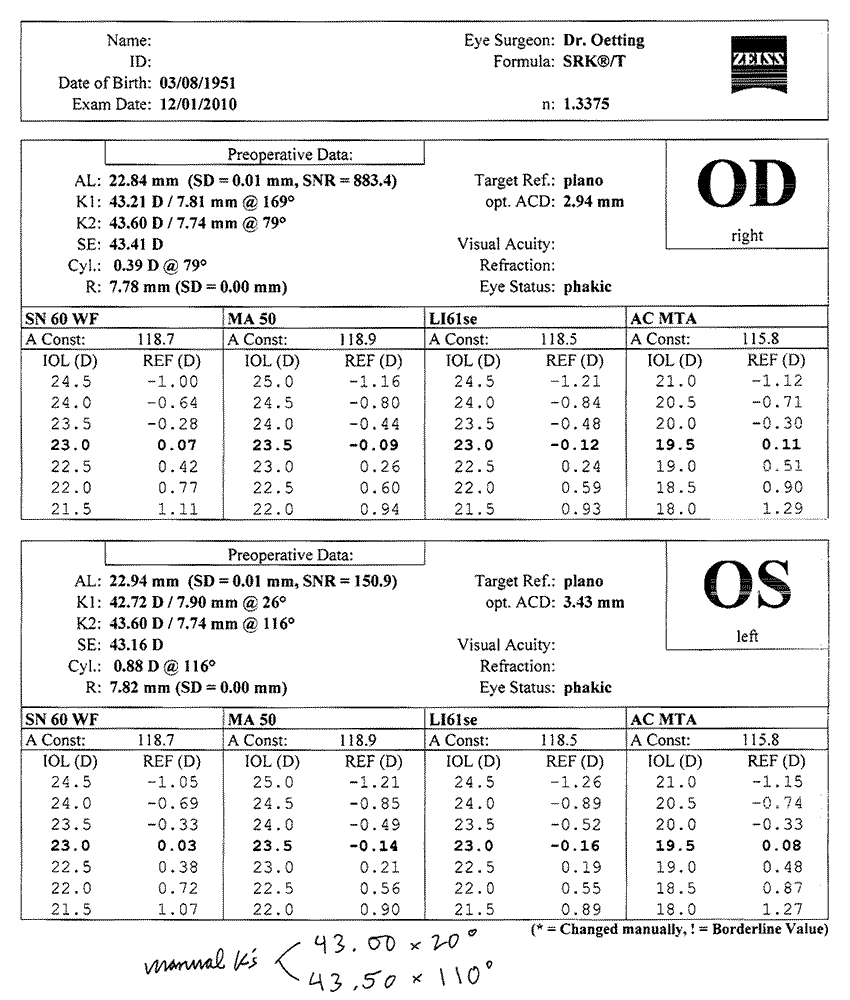
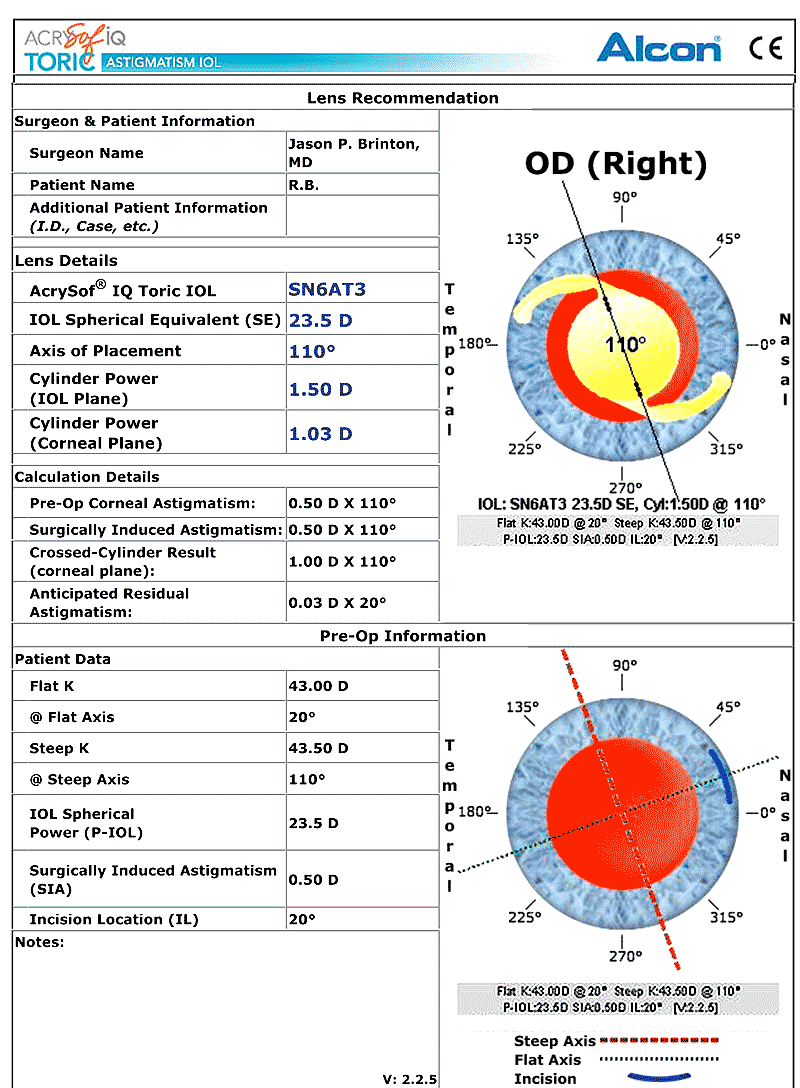
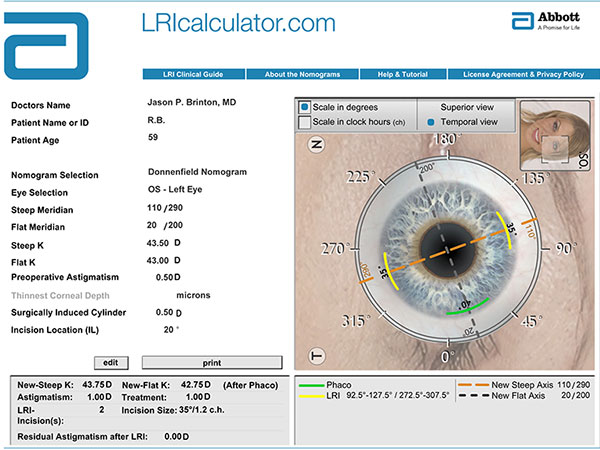
Topography, manual keratometry, and non-contact biometry (see Figure 1) were performed. The relevant keratometry and biometry values were entered into the toric IOL calculator at http://www.acrysoftoriccalculator.com (see Figure 2) and the LRI calculator at http://www.lricalculator.com (see Figure 3).
Topography showed regular bowtie with-the-rule astigmatism.
Manual keratometry was as follows: 43.00 @ 20° and 43.50 @ 110°.
Non-contact biometry was performed and gave the following measurements: axial length 22.94mm, K1 42.72 @ 26°, K2 43.60 @ 116° (see Figure 1). Targeting plano, a 23.5D SN60WF lens was tentatively selected.
Some surgeons use keratometry readings from a single source (such as IOL Master) to enter in the online toric IOL calculator. Some surgeons use multiple sources. If keratometry readings obtained via manual and automated methods differ greatly, further investigation is warranted. If these measurements are close we have opted to use the manual keratometry readings. Other surgeons, notably Brian Little, use an arithmetic mean of the figures obtained by the different sources and input these numbers into the online calculator. We are presently using a 2.75mm clear corneal incision, which is typically responsible for about 0.50D corneal flattening when placed temporally.
In this case, assuming an incision placed at 20° (for convenience of hand position), the resultant crossed-cylinder astigmatism is 1.00D x 110° as shown on the toric IOL calculation sheet. Using an SN6AT3 23.5D SE lens oriented at 110° would yield an anticipated residual astigmatism of 0.03D X 20°. The patient has no history of trauma or any other condition leading us to suspect loose zonules.
The LRI calculator called for paired 35° or 1.2-clock-hour peripheral corneal relaxing incisions centered at 110°. The planned residual astigmatism following the procedure would be 0.00D. The patient did not have dry eye or any other contraindication to LRIs.
After discussing the various options with the patient we decided to place the wound along the steep axis of astigmatism. Postoperatively the patient had a negligible amount of asgtigmatism and had excellent uncorrected vision at distance. He was pleased with the results of the procedure.
Intraocular lenses for presbyopia, Eyerounds tutorial by Tim Johnson, MD, PhD.
LRI calculator http://www.lricalculator.com
Acrysof Toric Calculator http://www.acrysoftoriccalculator.com
Video: Toric IOL
Video: Abortatoric
Video: Tora Toric
Budak K, Friedman NF, Koch DD. Limbal relaxing incisions with cataract surgery. J Cataract Refract Surg. 1998;24:503-508. PMID: 9584246
Chang DF. Comparative rotational stability of single-piece open-loop acrylic and plate-haptic silicone toric intraocular lenses. J Cataract Refract Surg. 2008;34(11):1842-7. PubMed PMID: 19006728.
Chang DF. Early rotational stability of the longer Staar toric intraocular lens: fifty consecutive cases. J Cataract Refract Surg. 2003;29(5):935-40. PMID: 12781279
Chang DF. Repositioning technique and rate for toric intraocular lenses. J Cataract Refract Surg. 2009;35(7):1315-6. PubMed PMID: 19545827.
Mingo-Bot n D, Mu oz-Negrete FJ, Won Kim HR, Morcillo-Laiz R, Rebolleda G, Oblanca N. Comparison of toric intraocular lenses and peripheral corneal relaxing incisions to treat astigmatism during cataract surgery. J Cataract Refract Surg. 2010;36(10):1700-8. PMID: 20870116
Osher RH. Combining phacoemulsification with corneal relaxing incisions for reduction of preexisting astigmatism. Paper presented at: The Annual Meeting of the American Intra-Ocular Implant Society; 1984; Los Angeles, CA.
Pineda R, Denevich S, Lee WC, Waycaster C, Pashos CL. Economic evaluation of toric intraocular lens: a short- and long-term decision analytic model. Arch Ophthalmol. 2010;128(7):834-40. PMID: 20625042
Poll JT, Wang L, Koch DD, Weikert MP. Correction of astigmatism during cataract surgery: toric intraocular lens compared to peripheral corneal relaxing incisions. J Refract Surg. 2011;27(3):165-71. PMID: 20873707
Suggested Citation Format: Brinton JP, Oetting TA. Phacoemulsification: Considerations for Astigmatism Management. EyeRounds.org. June 20, 2011; Available from: https://eyerounds.org/tutorials/phaco-astigmatism-management.htm