Chief Complaint: Painless vision loss in both eyes, worse in the right eye.
History of Present Illness: This patient presented with bilateral painless progressive vision loss, which had occurred over the previous eight months. It was worse in the right eye. She denied double vision, transient visual obscurations, or pulse synchronous tinnitus.
Past Ocular History: Negative, including surgery, trauma, or vision loss.
Family Ocular History: Positive for cataracts in her father and sister, age at diagnosis unknown.
Past Medical History: She had no known medical problems, though due to financial concerns and lack of health insurance she had not seen a physician in over fifteen years.
Medications: Naproxen as needed for headaches.
Social History: Occasional alcohol use. No history of tobacco or illicit drug use.
Review of Systems: Positive for chronic, stable headaches. Positive for unintentional 30-pound weight loss over the preceding six months. Complete review of systems otherwise negative.
Exam:
Visual acuity without correction: 20/160 right eye (OD) (improved to 20/60 with pinhole); 20/80 left eye (OS) (no improvement with pinhole)
Intraocular pressure: 8 mm Hg both eyes (OU)
Pupils: 4.5 mm in dark, 2 mm in light OD; 4 mm in dark, 2 mm in light OS; no relative afferent pupillary defect OU
Confrontation visual fields: full to finger counting OU
Extraocular movements: flick of intermittent exotropia
Cranial nerves: slight weakness of right facial nerve
Anterior segment: no injection OU, clear corneas OU, normal irides OU, 4+ posterior subcapsular cataract (PSC) OD, 3+ PSC cataract OS
Posterior segment: hazy view OU secondary to cataract
Potential acuity meter: 20/60 OD, 20/80 OS
B-scan echography: no vitreous debris OU, attached retina OU, optic disc elevation OS
 |
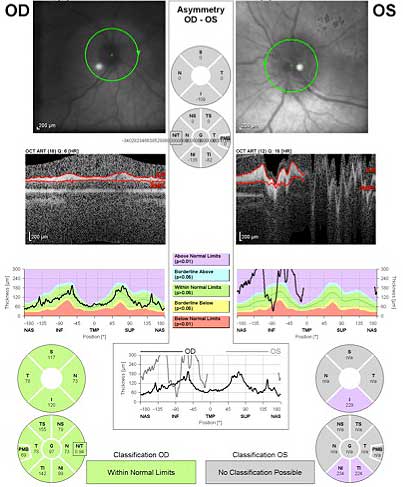 |
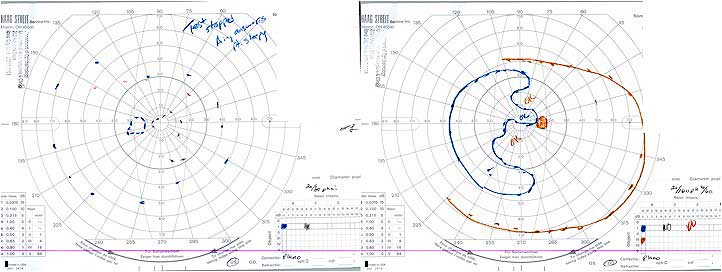
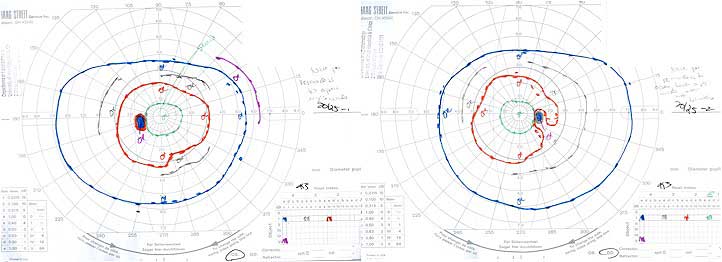
Clinical Course: This complicated case presented a diagnostic dilemma. It was felt that her dense cataracts were sufficient to explain her poor visual acuity, but she had no apparent risk factors for developing PSC; she denied history of steroid use, radiation, or neurofibromatosis type 2. She had no known history of diabetes mellitus and no apparent vitritis or pigmentary retinopathy, though posterior segment visualization was limited.
Furthermore, the etiology of her optic disc edema was unclear. She was a young, overweight female, but she denied symptoms of idiopathic intracranial hypertension, including new headaches, weight gain, transient visual obscurations, or pulse synchronous tinnitus, and MRI did not show an empty sella. She underwent lumbar puncture, which showed normal opening pressure and unremarkable cerebrospinal fluid indices. Chiefly to help restore her vision, but also to improve our ability to examine her posterior segment, she was referred for cataract surgery OU.
In addition, we ordered a number of laboratory tests and recommended she establish care with a primary care provider. She was found to have a normal complete blood count, electrolytes, thyroid stimulating hormone, folate, vitamin B12, and hemoglobin A1C. She underwent MRI of her orbits, which was unrevealing. Days later, her final lab test came back — the rapid plasma reagin (RPR) was positive. A confirmatory test, the Treponema pallidum particle agglutination assay (TP-PA), was also positive. The patient was diagnosed with syphilis.
She elected to receive treatment closer to her home, and received serial intramuscular penicillin G. She underwent uneventful cataract surgery OS first, then OD a week later, and at the time of publication her best corrected visual acuity was 20/20 OD and OS, and her disc edema had completely resolved.
 |
 |
Discussion: Originally described in the 1400s, syphilis is caused by the spirochete bacteria Treponema pallidum. In the United States, there has been a recent resurgence in incidence over the past decade, particularly among non-Caucasians, men who have sex with men and intravenous drug users. Over the past five years, the infection rate among young black men has increased 134 percent.[1] In 2006, the United States Centers for Disease Control estimated that men who have sex with men accounted for 64 percent of all cases of primary and secondary syphilis.[2]
Syphilis is staged according to the body parts affected, and is characterized by episodes of active disease intermixed with periods of latency. Primary syphilis involves the painless chancre, which begins within weeks of exposure as red papules which later coalesce into a firm, painless chancre that is typically found on the penis, anus/rectum, mouth, cervix, or labia. This lesion lasts 4-6 weeks before spontaneous resolution. Because serous discharge from the chancre is densely loaded with spirochetes, mucosal contact with the chancre is the primary route of transmission.[3]
Secondary syphilis begins 6-8 weeks after the chancre heals, if untreated, and involves a rash which begins as flat macules before progression to raised papules. It commonly involves the palms and soles and is not pruritic, which helps explain why it may be unrecognized by the patient.
Tertiary syphilis occurs in roughly 33% of untreated patients. It may be benign, displaying only gummatous granulomas in the skin, mucous membranes, or uveal tract. More severe manifestations include cardiovascular disease (aneurysms) or neurological disease (tabes dorsalis or generalized paresis).
Just as extraocular syphilis can affect multifarious body systems in myriad ways, the manifestations of ocular syphilis are also protean, as virtually every ocular substructure can be involved either individually or collectively. It is perhaps easiest to divide ocular syphilis into two groups: congenital and acquired.
Regarding congenital syphilis, the easiest systemic features for an ophthalmologist to recognize may be the widely spaced, centrally notched anterior incisors (Hutchinson’s teeth) and the abnormal facies (saddle nose), though other features may be present and are beyond the scope of this discussion. Congenital syphilis may present with interstitial keratitis, uveitis, optic neuritis, glaucoma, cataract, and/or retinal vasculitis. Nonulcerative stromal interstitial keratitis is the most common inflammatory sign of untreated congenital syphilis.[4]
Acquired syphilis may affect any number of ocular structures. The following table gives some examples, organized according to the progression of the ocular examination.
External adnexae |
Dacryocystitis, dacryoadenitis, lymphadenopathy |
Conjunctiva/sclera |
Chancre, conjunctivitis, scleritis, gumma |
Cornea |
Interstitial keratitis (more common in congenital syphilis) |
Pupil |
Light near dissociation, Horner’s syndrome |
Motility |
Internuclear ophthalmoplegia |
Lens |
Cataract |
Uveal tract |
Iris nodules, iritis, vitritis, multifocal choroiditis |
Optic nerve |
Papillitis, disc edema |
Retina |
Retinitis, neuroretinitis (especially in HIV+ patients), exudative retinal detachment |
Laboratory testing for syphilis involves two types of assays: non-treponemal and treponemal. The non-treponemal tests, such as RPR and VDRL, are less sensitive and less specific, and become negative after treatment. The sensitivity of these non-treponemal tests is estimated to be 78-86 percent in primary syphilis, and above 95 percent in secondary and latent syphilis.[5] The treponemal tests, such as TP-PA and FTA-ABS, are more sensitive and more specific, but because they remain positive for life even despite treatment, they are not typically used as an initial screening tool. Importantly, HIV patients may have negative serologies due to their immunosuppressed status.[6] It is recommended that all patients with documented syphilis undergo lumbar puncture for VDRL testing of the cerebrospinal fluid. Due to the relatively high co-infection rate, patients should also be tested for HIV.
Treatment of ocular syphilis is controversial, but always involves parenteral penicillin. Some argue that with anterior segment findings alone, ocular syphilis may be managed with benzathine penicillin intramuscular injections, with 2.4 million units injected intramuscularly once weekly for three weeks. Others argue that any ocular manifestations of syphilis warrants intravenous penicillin G for 10-14 days.[7,8] Some feel that intravenous treatment is warranted only if retinal or optic nerve involvement is present. Options for patients with penicillin allergy include ceftriaxone, doxycycline, or tetracycline; in this scenario an infectious disease consult is warranted. Residual inflammation is managed with cycloplegia and corticosteroids, administered either topically or via injection.
If recognized and treated early, the visual prognosis is excellent and full recovery may be possible. However, if left untreated, ocular syphilis can progress to glaucoma, optic atrophy, and retinal necrosis. Follow-up involves repeat ocular examination and serial measurement of VDRL at three and six months. A four-fold drop in the titer is desirable.
Given the extremely variegated possible presentations of ocular syphilis, a high degree of suspicion is necessary to make the diagnosis. In addition to cases involving the “classic” scenarios listed below, testing for syphilis may be warranted when other diagnostic possibilities have been eliminated or in atypical or severe presentations. It is particularly important to consider in high-risk patients with uveitis, scleritis, episcleritis, or optic neuritis.
Finally, regarding our patient, syphilis manifesting with optic disc edema has been infrequently reported in the literature.[9] To our knowledge there is no report of syphilis manifesting with PSC cataract in the absence of vitritis, as was the case with our patient. Given the family history, it is conceivable that her cataracts were familial or spontaneous, and unrelated to the syphilis infection.
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENT
|
Weed M, Johnson AT, Thurtell M. Ocular Syphilis Presenting with Posterior Subcapsular Cataract and Optic Disc Edema: 30-year-old female with progressive bilateral vision loss EyeRounds.org. Posted Oct 10, 2012. Available from http://www.EyeRounds.org/cases/157-ocular-syphilis.htm.

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.