Chief Complaint: “Double vision”
A 57-year-old male presented with a complaint of diplopia following head trauma the week prior. He was standing on a stool to change a light bulb in the kitchen when he lost his balance, fell to the tiled kitchen floor, and struck his head. He lost consciousness for less than 1 minute. He noticed diplopia immediately upon awakening, but had no other neurologic symptoms. He presented to his local emergency department for evaluation. Magnetic resonance imaging (MRI) of his brain was unrevealing and computed tomography (CT) did not show any orbital fractures.
His diplopia persisted, prompting his initial visit to our clinic. The diplopia had not worsened or improved since onset. He described painless, binocular, vertical diplopia that worsened when he looked to the left, but improved when he tilted his head to the left. He thought that the diplopia was worse when he tried to read. He had been closing one eye to help relieve his symptoms.
Figure 1
The strabismus measurements showing a right hypertropia (RHT) in primary position that worsens in adduction (left gaze) and also in right head tilt. There is right superior oblique underaction and right inferior oblique overaction, as well as 7 degrees of excyclotorsion on double Maddox rod (DMR).
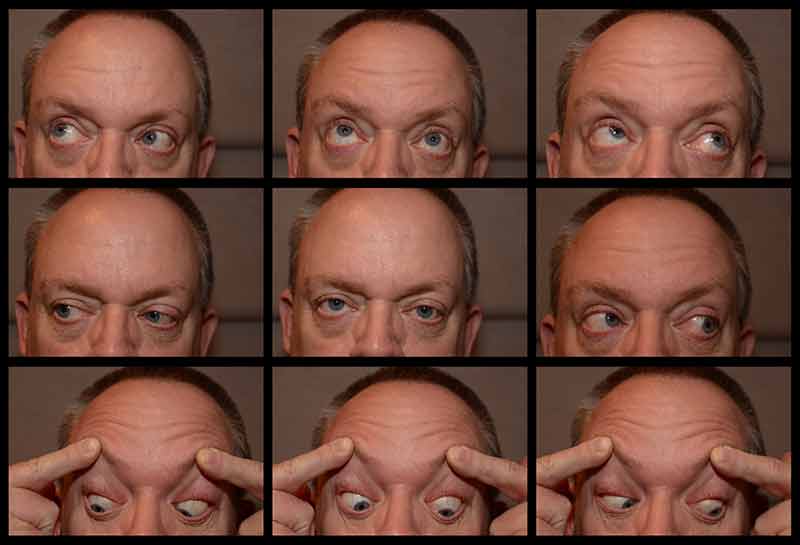
Figure 2
Note the compensatory left head tilt with a right hypertropia (RHT) in primary position that worsens in adduction (left gaze). There is right superior oblique underaction and right inferior oblique overaction, both notable in adduction.
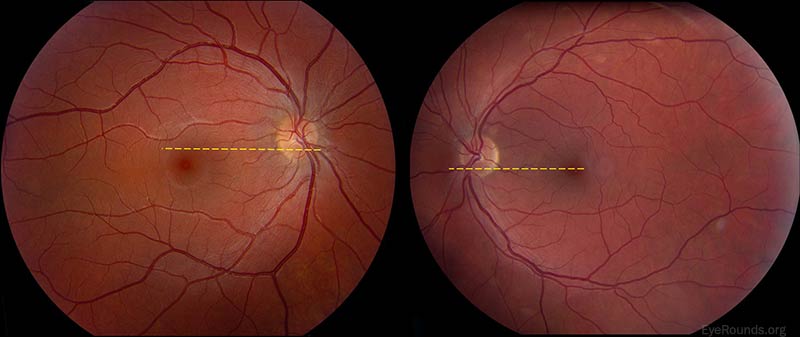
Figure 3
Excyclotorsion of the right fundus. Note that the yellow dashed line drawn horizontally from the inferior 1/3 of the disc in the left (normal) eye intersects the fovea. A line drawn in the same manner in the right eye crosses superior to the fovea. This is an objective sign of fundus excyclotorsion.
Traumatic right cranial nerve (CN) IV palsy
Given the acute, painless onset of the vertical diplopia with a positive Parks-Bielschowsky 3-step test (see "Clinical Features and Evaluation," below) for a right CN IV palsy in the absence of vascular risk factors, negative neuroimaging, and in the setting of recent closed head trauma – the diagnosis of traumatic right CN IV (trochlear nerve) palsy was made.
Given the incomitant nature of his misalignment and fundus torsion on the right, in addition to the patient not wanting to wear glasses at all, it was elected to not offer temporary symptomatic treatment with Fresnel prism. The patient was treated with occlusion (patch) therapy over his right eye. At his follow-up appointment 3 months later, he reported resolution of his diplopia. His alignment and motility had returned to normal.
Cranial nerve IV (trochlear nerve) is a somatic motor nerve that innervates the superior oblique muscle, which intorts, infraducts, and abducts the globe. The nucleus of CN IV lies at the level of the inferior colliculus in the tegmentum of the midbrain. The CN IV fascicle decussates to the contralateral side at the superior (anterior) medullary velum in the roof of the fourth ventricle prior to exiting the dorsal brainstem. After it leaves the brainstem, CN IV curves around the cerebral peduncle laterally at the superior border of the pons, emerging ventrally between the posterior cerebral and superior cerebellar arteries along with CN III. Its pathway continues anteriorly to pierce the dura at the borders of the tentorium cerebelli, into the cavernous sinus along its lateral wall, before entering the orbit through the superior orbital fissure superior to the annulus of Zinn. From there, it passes ventrally and medially to innervate the superior oblique.
CN IV has the longest intracranial course of any of the cranial nerves and is the only nerve to exit the brainstem dorsally. Consequently, it is especially susceptible to damage in the setting of head trauma. Trauma accounts for roughly 44% of acquired trochlear nerve palsies with nearly 25% of cases being bilateral and, thus, it is the most common etiology of an acquired CN IV palsy [1]. Approximately 75% of all CN IV palsies are congenital [2] and in the pediatric population nearly 50% are congenital [3]. The exact cause of congenital CN IV palsy is often uncertain, but it has been speculated that it may result from hypoplasia of the CN IV nucleus, birth trauma, anomalous muscle insertion, muscle fibrosis, structural abnormalities of the tendon, or inferior oblique muscle abnormalities [4].
Lesions affecting CN IV can occur anywhere along its course from the midbrain to the orbit. Lesions affecting the CN IV nucleus can arise from hemorrhage, infarction/stroke, trauma/surgical injury, or demyelination in the midbrain and will result in dysfunction of the contralateral superior oblique muscle. Both unilateral and bilateral superior oblique pareses have been reported in association with the dorsal midbrain syndrome. Since the oculosympathetic fibers traveling to the pupil descend adjacent to the CN IV fascicle in the brainstem, a lesion in this location can give a contralateral superior oblique paresis with an ipsilateral Horner’s syndrome.
As the nerve fibers exit the brainstem and enter the subarachnoid space, they become especially prone to injury from head trauma resulting in unilateral or bilateral superior oblique pareses. Occipital and frontal impact can give rise to bilateral CN IV palsies due to a contusion at the point of decussation of the nerves or a unilateral palsy due to either compression or shearing of the individual nerve by the tentorium. Damage to CN IV can even occur in the setting of seemingly minor head trauma without loss of consciousness. Compression from tumors that form in this space (i.e., primary tumors or metastases) as well as intrinsic neoplasms of the fourth nerve itself (i.e., schwanommas) can also cause CN IV palsy. Inflammation due to infectious disease (e.g., bacterial meningitis) or due to a primary inflammatory disease (e.g., sarcoidosis) occasionally causes CN IV palsy. In the subarachnoid space, CN IV receives its blood supply from branches of the superior cerebellar artery. Loss of perfusion to the vasa nervorum of the nerve will result in a microvascular (ischemic) CN IV palsy. Microvascular CN IV palsy typically occurs in patients older than 50 years of age who have risk factors for small vessel disease (e.g. hypertension, hyperlipidemia, diabetes, smoking). The CN IV palsy is typically accompanied by periorbital pain, which can be severe. Microvascular ischemia is the second most common cause of acquired CN IV palsy.
It is uncommon to see an isolated CN IV palsy from lesions in the cavernous sinus given the presence of other cranial nerves passing though this space. Trauma, along with herpes zoster, inflammation, aneurysmal compression, and neoplastic compression are among the common causes of damage to CN IV in this region, but, again, these entities usually do not give rise to an isolated CN IV palsy. Similarly, lesions in the orbit causing CN IV palsy are also commonly seen in association with other cranial nerve palsies and orbital signs, such as chemosis, proptosis, and conjunctival injection. Trauma, inflammation, or mass effect in the orbit can damage the nerve, but could also affect the trochlea, superior oblique muscle, or superior oblique tendon. Although rare, giant cell arteritis can give rise to a cranial mononeuropathy and should be screened for in appropriate populations.
Patients with acquired CN IV palsy typically present with acute onset, binocular vertical or oblique diplopia that may have a torsional component. The diplopia is typically worse in down gaze (consequently, they will often complain of difficulty reading) and lateral gaze toward the contralateral side. The patient may adopt a compensatory contralateral head tilt. Strabismus measurements will show an incomitant hypertropia, which can be objectively measured with cover testing and prism neutralization in the different gaze positions and head tilts. Maddox rod or red filter testing can be useful when evaluating smaller degrees of misalignment. The hypertropia will worsen with adduction of the hypertropic eye and with head tilt to the ipsilateral side. It is typically accompanied by excyclotorsion of the affected eye ranging anywhere from 1 to 8 degrees in amplitude. The hypertropia worsens when the affected eye is adducted, because the superior oblique is an infraductor of the eye in this position; its weakness will be more apparent because there is no opposition to its antagonist muscle, the inferior oblique, in this position. The hypertropia worsens with ipsilateral head tilt since this position stimulates the vestibular-ocular reflex driven ocular counter-roll that activates the ipsilateral intorters (superior oblique and superior rectus) and the contralateral extorters (inferior oblique and inferior rectus). When the ipsilateral superior oblique is weak, the ipsilateral superior rectus acts alone for intorsion in this capacity, but secondarily worsens the hypertropia by elevating the eye [4]. The excyclotorsion results from the reduced incyclotorsion of the ipsilateral eye, which can be clinically assessed with double Maddox rod testing or objective fundus torsion on dilated funduscopic examination. Additionally, a small esotropia may be found on down gaze as the superior oblique is also a weak abductor. There may be underaction of the ipsilateral superior oblique accompanied by overaction of the ipsilateral inferior oblique on evaluation of versions, but the versions may also appear normal. Because of this, the diagnosis of CN IV palsy is not made by versions, but rather with the Parks-Bielschowsky three-step test (see video).
The sudden onset of an acquired CN IV palsy without a history of head trauma or painful onset in a patient who has risk factors for small vessel disease (e.g., hypertension, hyperlipidemia, diabetes), should be considered for further neurological work-up and neuroimaging if the clinical situation dictates, especially if accompanied by other neurologic signs or symptoms.
Bilateral CN IV palsies usually present with a large V-pattern esotropia (typically greater than 25 PD change from upgaze to downgaze). A trademark characteristic of bilateral CN IV palsies is the presence of alternating hyper-deviations on gazes and head tilts (i.e., a right hypertropia in left gaze and right tilt that changes to a left hypertropia in right gaze and left tilt). Affected patients often report a torsional component to their diplopia, as it is common for them to have excyclotorsion of 10 degrees or more between the two eyes. Some bilateral CN IV palsies may be “masked.” In these cases, the palsy of the other eye does not become manifest until the original palsy has been surgically treated. The second palsy may take days, weeks, or months to become manifest after surgery. In evaluating a patient with a possible masked bilateral CN IV palsy, fundus examination or photography to assess objective torsion should be considered, in addition to double Maddox rod testing and taking measurements in tertiary positions -- particularly in gaze up and to the right and up and to the left.
Patients with congenital CN IV palsies often present later in life due to decompensation from the gradual loss of fusional amplitudes that accompanies aging. These patients tend to display larger than normal vertical fusional amplitudes (e.g. 10-15 PD, where normal is 1-3 PD) and may report a history of intermittent diplopia when they are tired or ill and experience difficulties such as diplopia or asthenopia when reading since the deviation increases in downgaze. It can be beneficial to examine old photographs or the patient’s driver license to assess for a longstanding head tilt (ocular torticollis). Facial asymmetry (hemifacial microsomia) on the side of their preferred head tilt may also be noted.
The treatment of CN IV palsy includes both non-surgical and surgical interventions; the indications vary with etiology. Many cases of acute acquired CN IV palsy spontaneously resolve with time. In these cases, treatment is only temporary and geared at symptomatic relief until the condition resolves. Management options include recommending anomalous head postures to alleviate cyclo-vertical diplopia, prisms to compensate for diplopia in primary gaze, or occlusion (patching) of the paretic eye. Management with prism can be challenging given the incomitant nature of the deviation, especially when there is a torsional component to the deviation. Botulinum toxin injection into the inferior oblique muscle has been used with variable success to reduce the hyper-deviation and thereby alleviate diplopia during recovery. Microvascular CN IV palsies usually resolve spontaneously within 3-4 months and require no further treatment outside of symptomatic occlusion or prism if the diplopia persists. If a presumed microvascular CN IV palsy does not spontaneously recover as expected, neuroimaging is warranted to investigate for an alternate etiology. Although many acquired CN IV palsies fully recover, others only partially recover while others show very little improvement at all. One study reported that at least 82% of patients with acquired CN IV palsies show a partial recovery in a 6-month period, with 52% showing a complete recovery in a 6-month period [6]. Patients with CN IV palsy due to trauma or microvascular ischemia were the most likely to recover. A recovery time of 6-12 months with subsequent stability of alignment measurements is recommended before performing strabismus surgery. Strabismus surgery is indicated in congenital and non-recovered, acquired CN IV palsies in order to restore binocularity, relieve diplopia, and/or alleviate anomalous head positioning. Possible procedures include strengthening the underacting muscle (i.e., superior oblique tuck), weakening the ipsilateral direct antagonist (i.e., inferior oblique recession), or weakening the yoke muscle (i.e. contralateral inferior rectus recession).
Etiology
|
Signs
|
Symptoms
|
Treatment
|
Klauer AJ, Kirkpatrick CA, Thurtell MJ. Cranial Nerve IV (Trochlear Nerve) Palsy: 57-year-old male complaining of vertical diplopia after head trauma. EyeRounds.org. posted Nov. 10, 2015; Available from: https://eyerounds.org/cases/225-CN-IV-palsy.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.