Chief Complaint: Abnormal screening exam in a pediatric patient
History of Present Illness
A 7 year-old healthy girl presented to the pediatric ophthalmology clinic for further evaluation after having an abnormal screening exam with a local eyecare provider. The patient did not have any visual complaints in either eye. The patient’s mother denied noticing any eye crossing, eye drifting. The patietn denied eye pain, photophobia or nyctalopia. There was no known history of ocular trauma.
Past Ocular History
Past Medical History
Medications
Allergies
Family History:
Social History:
Review of Systems:
OCULAR EXAMINATION
| OD | OS | |
|---|---|---|
| Disc | Normal | Normal |
| Cup-to-disc (C/D) ratio | 0.3 | 0.3 |
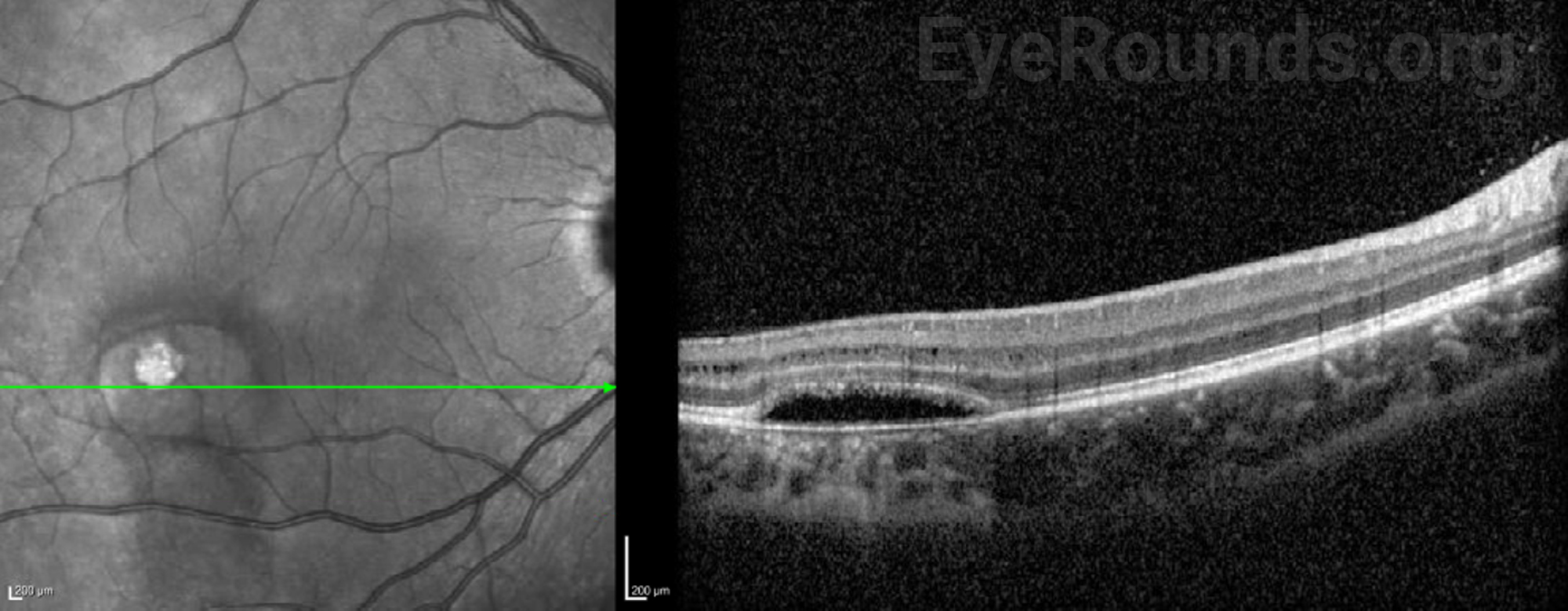
| Macula | In the inferotemporal aspect of the macula is a torpedo-shaped, well-demarcated, hypopigmented lesion without adjacent subretinal fluid | Normal |
| Vessels | Normal | Normal |
| Periphery | Normal | Normal |

Differential Diagnosis
DIAGNOSIS: Torpedo Maculopathy
CLINICAL COURSE
The examination and diagnostic imaging findings, in addition to an asymptomatic presentation, in this case are consistent with a clinical diagnosis of torpedo maculopathy. In the absence of any ocular sequalae (i.e., CNVM), expectant management was recommended with plan for serial examination in the future.
DISCUSSION
Etiology/Epidemiology
First described as a solitary hypopigmented nevus by Roseman and Gass in 1992, torpedo maculopathy (TM) is a rare, benign congenital abnormality of the retinal pigment epithelium (RPE), leading to changes in the architecture of the outer retinal layers.[1] Given the disease is often asymptomatic, the epidemiology is likely underestimated, however, a case series of eight pediatric patients in Northern Ireland estimated a prevelance of approximately 2 patients per 100,000 population under the age of sixteen.[2]
Pathophysiology
The pathophysiology is not fully understood, though various mechanisms have been proposed. One proposed pathophysiology is that the clinical lesion develops as a result of incomplete differentiation of the nerve fiber layer along the horizontal raphe during development,[3] from primary disturbances of the choroidal development and vasculature.[4] The most widely accepted mechanism is that torpedo maculopathy results from a persistent defect in the development of the RPE in the fetal temporal bulge, which is a dense collection of RPE cells that occurs in the temporal macula between the 4th and 6th month of embryologic development. This corresponds with the location of torpedo maculopathy. When the bulge retracts, it is thought that a residual depression can remain, leading to the characteristic lesion seen on exam.[5]
While the lesion is typically not progressive and classically does not affect vision, there have been few case reports of (CNV) associated with the condition.[2, 6-8] Additionally, there have been reports of neurosensory retinal detachment and central serous chorioretinopathy occurring in torpedo maculopathy.[9-11]
Signs/Symptoms
TM is typically an asymptomatic condition, rarely affecting visual acuity. However, there have been reports of central scotomas occurring with TM, which may also be a byproduct of sequaelae such as CNVM.[9, 11, 12]
Testing/Laboratory work-up
Imaging
The classic finding on fundus photos in TM is a solitary, unilateral, oval- or “torpedo”-shaped, hypopigmented lesion, located along the horizontal raphe, temporal to the fovea with a tip pointing to the central macula.[13] These findings are typically sufficient for diagnosis. On OCT, torpedo maculopathy is characterized by preservation of the inner retinal layers, thinning of the outer retina above the lesion, hyperreflectivity of the RPE, and hyperreflectivity of the deep choroid, likely secondary to RPE attentuation.[11, 14] Photoreceptor loss has also been reported in one case.[11] Based on OCT findings, TM lesions can be classified as either type 1 or type 2. Type 1 lesions have a pattern of outer retinal attenuation without outer retinal cavitation, whereas type 2 lesions have both attenuation of outer retinal structures and outer retinal cavitation.[15] OCT angiography (OCTA) findings in TM consistently demonstrate a normal superficial retinal vascular plexus and diffuse attenuation of the choriocapillaris.[16-20] Varying involvement of deep retinal layers have been reported, from loss of deep vessels corresponding to the lesion [16] to few, isolated changes in the deep vascular network.[18] These dissimilar findings have been noted in patients at different ages, with the diffuse vascular loss occurring in an older patient, possibly suggesting that changes to the retinal vascular plexus develop over time.
Treatment/Management
Given that TM is typically an incidental, asymptomatic finding, and that it is usually stable and non-progressive, there is no specific treatment targeting the condition. Since there have been reports of CNVM, management usually consists of regular follow-up with monitoring of the lesion.[2]
EPIDEMIOLOGY OR ETIOLOGY
|
CLINICAL SIGNS
|
SYMPTOMS
|
TREATMENT/MANAGEMENT
|
Shonka B, Mansoor M, De Andrade L. Torpedo Maculopathy. EyeRounds.org. Posted January 4, 2024; Available from https://EyeRounds.org/cases/351-torpedo-maculopathy.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.