Chief Complaint: 32-year-old female patient presented with a "black spot" in the vision of her left eye.
History of Present Illness: The patient awoke the morning of presentation with a black spot inferotemporal to fixation. This was accompanied by blurry vision in the left eye. The patient had poorly controlled asthma the day prior to the onset of her visual symptoms associated with an intense coughing episode. She had no complaints regarding the right eye.
Past Ocular History: Unremarkable for surgery or trauma. She is myopic and wears -4.50 sphere spectacle correction in both eyes.
Medical History: History of asthma and migraine headaches.
Medications: Oral contraceptive pill daily. Albuterol inhaler and sumatriptan both as needed.
Family History: No history of coagulopathy.
Social History: Noncontributory.
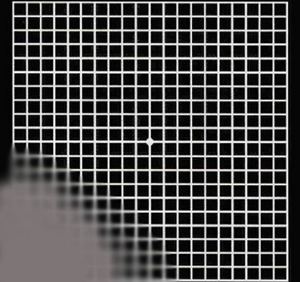
| Figure 1: Amsler grid, OS. Amsler grid testing can be used to evaluate the central 10 degrees of the visual field. The patient described a scotoma inferotemporal to fixation in the left eye, as depicted here. | Figure 2: Fudus photograph, OS. A large preretinal hemorrhage is visagle around the upper margin of the disc and extending into the macula. |
 |
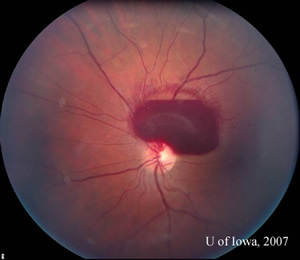 |
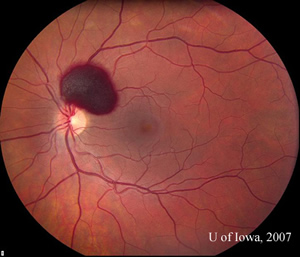
Course: Blood pressure measured 124/73. Complete blood count was normal, with a hemoglobin of 14.2 and platelet count of 300. The patient was seen by the Retina Service at the University of Iowa and the decision was made to observe the hemorrhage and improve control of her asthma symptoms with her Primary Care Physician. Two weeks later, the preretinal hemorrhage had diminished in size, but the patient continued to report blurry vision (VA 20/40) with the left eye (see Figure 3). She was seen again two months later and the hemorrhage had largely resolved. Her vision had recovered to baseline (VA 20/20) (see Figure 4).
| Figure 3: Fundus photo, OS, 2 weeks after initial presentation. | Figure 4: Fundus photo, OS, 2 months after initial presentation showing near complete resolution of hemorrhage. |
 |
 |
Discussion: Valsalva Retinopathy is a rare cause of preretinal hemorrhage (1). Typically, patients present with acute painless loss of vision after performing a Valsalva-type maneuver. Mechanistically, it is thought that an acute rise in intrathoracic/intraabdominal pressure from closure of the glotis leads to an intraoclular venous pressure increase and capillary rupture. The patient in this case provided a classic history of straining prior to the onset of symptoms (i.e. coughing during asthma attack). Valsalva retinopathy has also been described following weight lifting, vomiting, sexual activity, end stage labor, blowing musical instruments, and compressive injuries (2-6).
Some debate exists as to where the hemorrhage is actually located. Some have localized the hemorrhage to a sub-internal limiting membrane (ILM) location (7-9), while others have provided convincing data to support a subhyaloid position (10). While not utilized in this case, OCT can assist in identifying the exact location of such hemorrhages.
This patient was observed and the hemorrhage cleared relatively quickly. This is often the case, but occasionally the hemorrhage can be slow to resolve. Since the late 1980s, several authors have advocated the use of Nd:YAG hyaloidotomy / membranotomy to assist in visual recovery. A large hemorrhage that obscures the macula may prompt such an approach as these patients may have dramatically reduced vision. Results in the literature have been quite impressive with this treatment (11,12).
EPIDEMIOLOGY
|
SIGNS
|
SYMPTOMS
|
TREATMENTCan rule out other etiologies predisposing to preretinal hemorrhage:
Observation: hemorrhage resolves in weeks to months Patient shoud be instructed to avoid straining activites in the acute phase Avoid anticoagulation if possible Nd:YAG laser for non-clearing hemorrhage or if rapid improvement in vision is sought (monocular patient) |
Rauen M, Oetting TA, Weingeist TA: Valsalva Retinopathy: Vision loss after asthma attack. EyeRounds.org. July 10, 2007; Available from: http://www.EyeRounds.org/cases/67-Valsalva-Retinopathy-Vision-Loss-Asthma.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.