
The University of Iowa
Department of Ophthalmology and Visual Sciences
January 9, 2023
Amblyopia is the most common cause of unilateral vision loss in children. It affects roughly 1-4% of children worldwide and if untreated, causes significant, irreversible visual impairment [1,2]. Amblyopia may impact academic outcomes, self-esteem, and lead to increased feelings of frustration, isolation, and depression [3]. Children with amblyopia demonstrate significantly slower reading times and multiple-choice answer completion times than their peers, even when treatments result in 20/30 or better vision of the amblyopic eye [4,5]. Studies have also shown children with amblyopia are more likely to experience bullying and difficult interactions with peers, with impact on education, activities, and self-esteem [3].
In this article we will introduce the development of the normal visual processing system of the eye and the pathophysiology of amblyopia and its subtypes (deprivation, refractive, and strabismic). We will also discuss how to detect amblyopia, treatment options, and describe the prognosis of patients with and without early detection.
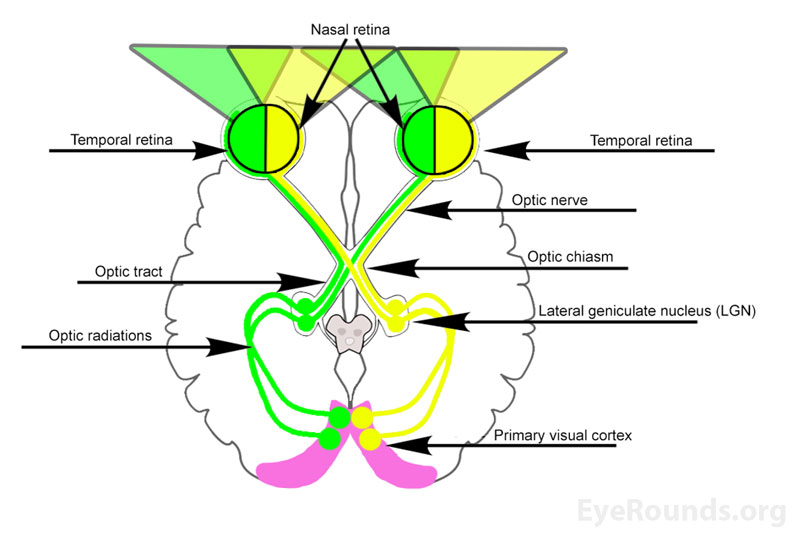
Under normal conditions, light passes through a clear cornea and a clear lens until it reaches the photoreceptors of the retina. These receptors are known as rods and cones and generate chemical signals in response to light entering the eye. These signals are transmitted through the bipolar cells to activate the cell bodies of the ganglion cell layer, the axons of which serve as the foundation of the retinal nerve fiber layer (RNFL). The RNFL consists of temporal and nasal fibers, which relay impulses from the nasal and temporal aspects of the visual field, respectively. These fibers then congregate at the optic disc to form the optic nerve [6].
The optic nerve enters the middle cranial fossa through the optic canal and continues until the optic nerves from each eye join to form the optic chiasm directly above and behind the pituitary gland. At the chiasm, the nasal fibers from each eye decussate and join the temporal fibers of the contralateral eye to form the optic tracts. The optic tracts then synapse at the lateral geniculate nucleus (LGN) within the thalamus. These fibers continue to form the optic radiations of the parietal and temporal lobes, which terminate at the cuneus gyrus and lingual gyrus of the primary visual cortex, respectively [6] (Figure 1).
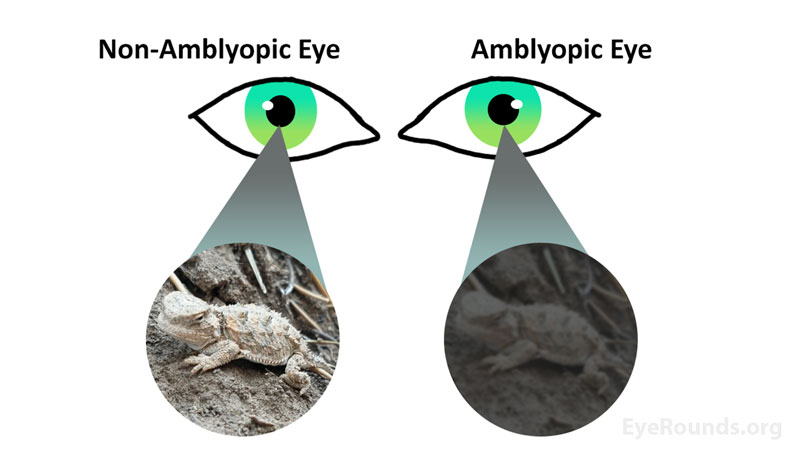
Amblyopia is most commonly a unilateral disease, however it can also present bilaterally. In unilateral amblyopia, the visual stimulation of one eye is impaired. As the visual system develops, the eye with normal visual stimulation is favored, causing more neural networks to be devoted to the normally stimulated eye. As a result, fewer neural connections are made to the eye with impaired visual stimuli and amblyopia develops. This amblyopia is characterized by a neurogenic suppression of signals from one eye, despite the initial visual potential being equal between the two eyes (Figure 2). The visual disruptions responsible for development of unilateral amblyopia are categorized into three main etiologies: Strabismic, Deprivation, and Refractive [2,7]. Bilateral amblyopia will be discussed later in this article.
Strabismic Amblyopia
Strabismus, defined as an abnormal alignment of one or both eyes, is the most frequent cause of amblyopia. The most common form of strabismus is an esotropia in infancy or early childhood which causes diplopia, or double vision [8]. In response to the discomfort of diplopia, the pediatric brain suppresses the visual input from one eye, leading to impaired visual development of the suppressed eye [2].

Deprivation Amblyopia
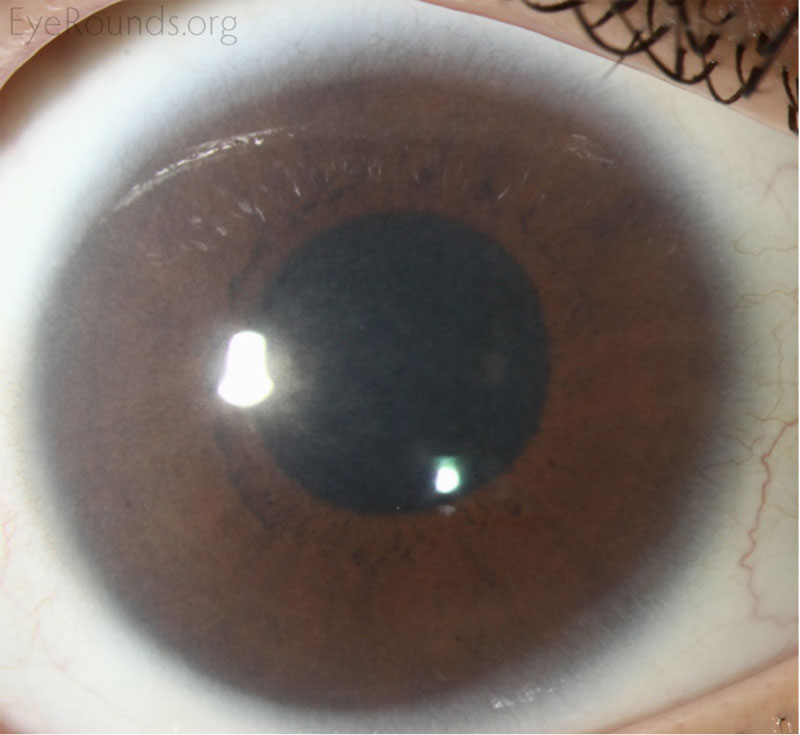
Although the least frequent cause of unilateral amblyopia at ≤3%, deprivation causes the most severe form of amblyopia [15]. Deprivation amblyopia occurs when there is a disruption of the visual pathway, which may occur secondary to a cataract (Figure 4), corneal opacity (Figure 5), blepharoptosis, periocular lesions, and vitreous hemorrhage [10]. Similarly, deprivation amblyopia can also be caused by the absence of visual stimuli, such as covering one eye for an extended period [2].

Refractive Amblyopia
Refractive amblyopia stems from refractive errors such as high hyperopia (>3.25D) [13], astigmatism, and most commonly from a differing refractive error between the two eyes known as anisometropia (interocular acuity difference of 3 or more logMAR lines) [14]. Generally, an eye with hyperopia or astigmatism is more at risk of developing amblyopia than an eye with myopia, as a myopic eye will maintain focus on near objects and avoid visual suppression [2].
Bilateral Amblyopia
Bilateral amblyopia can develop in children when the above conditions affect both eyes. Bilateral refractive amblyopia (e.g., isoametropic amblyopia) can develop with large amounts of uncorrected hyperopia and/or astigmatism in both eyes. Bilateral cataracts or corneal opacities can cause bilateral deprivation amblyopia. Regardless of the underlying cause, most children with bilateral amblyopia present with symmetric visual deficiencies at baseline [7].
The mechanism of bilateral amblyopia is thought to be related to failure of both eyes to achieve a clear foveal image resulting in abnormal development of the visual cortex bilaterally. Prevalence at the time of entry into school is estimated to be 0.5% [7].
Most patients with unilateral amblyopia are asymptomatic and their decreased visual acuity and stereopsis go unnoticed until detected on a routine visual screening exam. However, parents may bring their child to a physician with complaints of blurred vision, discomfort in one eye, clumsiness, or frustration with occlusion of their good eye. Similarly, common presenting complaints that may help detect underlying amblyopia are strabismus and leukocoria. In some cases of profound amblyopia, abnormal head positioning may be adopted to improve visual acuity [15,16].
Screening for amblyopia is incredibly important because most patients do not experience any symptoms until advanced stages of disease, and treatment of amblyopia in older children is generally much less effective [2]. To combat this, the American Association for Pediatric Ophthalmology and Strabismus (AAPOS) recommends attempts to perform photoscreening begin at the 12-month well-child visit and be repeated until the child can accurately perform visual acuity testing [1].
Photoscreening is the interpretation of specialized photographs of a child’s eyes to detect pathologies such as refractive error, corneal opacities, strabismus, or other external eye abnormalities which may be risk factors for amblyopia. Traditional vision screening, including both visual acuity and stereopsis testing, has been shown to detect up to 94% of patients with visual field defects [17]. Cellphone and tablet applications are also available to encourage more widespread amblyopia screening of school children [18].
Children with a family history of strabismus or amblyopia, prematurity, or past eye misalignment are at higher risk of developing amblyopia and should be watched closely for early signs of the condition [19]. If recognized early, the vision-threatening consequences of amblyopia can often be minimized with appropriate management [2].
A more comprehensive guide to amblyopia screening can be found here: https://eyerounds.org/tutorials/amblyopia/index.htm
When amblyopia is suspected, a full ophthalmic exam is warranted. The exam must include age-appropriate visual acuity testing and a refraction (cycloplegic retinoscopy, autorefraction, or traditional refraction depending on the patient’s age and cooperation). Tests of stereopsis and binocular function such as the Graded Circles Stereopsis test and Worth Four-Dot test should also be performed [2].
A thorough external examination is also necessary to evaluate possible external causes including ptosis, lid hemangiomas, or other lesions that could lead to impairment of visual development. Anterior segment examination should be performed to assess for corneal, anterior chamber, vitreous or lens abnormalities [2].
Additionally, the remainder of the standard eight step ophthalmic exam should be completed to evaluate motility, ocular alignment, and pupillary function. Finally, a funduscopic examination is essential to evaluate the retina and identify pathologies that may cause disruptions in visual development [2].
Exam |
Methods and components to assess |
|---|---|
Visual Acuity and Refraction |
Assess using age-appropriate visual acuity methods and cycloplegic retinoscopy |
Pupils |
Look for anisocoria, reactivity of each pupil and assess for a relative afferent pupillary defect |
Extraocular motility and alignment |
Have the patient look in the nine cardinal positions of gaze and use cover/uncover testing to assess for subtle misalignments |
Intraocular pressure |
Assess via iCare, Goldmann applanation, or Tonopen |
Confrontational visual fields |
Assess each quadrant by having the patient count the number of fingers held up in each quadrant, or by reactivity to stimulus in the respective quadrant |
External examination |
Look for ptosis, lid hemangiomas, or other miscellaneous lesions/abnormalities |
Slit-lamp examination |
Lids/lashes/lacrimal system: Anatomy, contours, and lesions if present Conjunctiva/sclera: Injection and lesions Cornea: Epithelial disruptions, cloudiness, stromal opacities, endothelial lesions Anterior chamber: Cell and flare, chamber depth Iris: Pupil shape, transillumination defects, nodules Lens: Lens location, nuclear, cortical or subcapsular cataract Anterior vitreous: Inflammation, hemorrhage, pigmented cells |
Fundoscopic examination |
Optic nerve: Cup-to-disc ratio, Pallor, Symmetry Macula: Drusen, edema, exudates Vessels: Hemorrhage, size discrepancies |
Amblyopia is a diagnosis of exclusion; a careful history, thorough physical examination, and understanding of possible etiologies are required to diagnose this condition [2]. Following exclusion of other visual disorders as the underlying cause, amblyopia is diagnosed by identification of diminished visual acuity in one or both eyes in the presence of an amblyogenic factor [15].
In young children this diagnosis is especially elusive because visual acuity can be difficult to measure. However, acuity can be estimated by observing the child’s reactions when one eye is covered, including watching the child's ability to follow objects with one eye and noting increases in fussiness with eye occlusion. Additionally, the induced tropia test in which a 12-14 diopter prism is held over each eye and the visual behavior is observed can be used to determine if one eye is favored over another. Amblyopia should be considered as a diagnosis in children with asymmetric visual behavior [19].
Early detection and intervention are essential for optimal treatment of amblyopia, with best results when treated as early as possible and before the age of 9 years. In bilateral cases, treatment mainly consists of addressing the etiology of the diminished vision and monitoring improvement over time. However, often there is residual bilateral amblyopia even after correction of the underlying cause [20].
In some cases of anisometropic amblyopia, improvement may occur with refractive correction alone. However, in most unilateral cases, the mainstay of treatment is based on increasing visual stimulation of the amblyopic eye by forcing its use. Multiple methods are available to encourage use of the amblyopic eye including patching or pharmacologic penalization of the non-amblyopic eye [21,22,23].
Surgical Intervention
Amblyopia alone is not a surgical condition; however surgical intervention may help treat the underlying cause of amblyopia development. In patients with deprivation amblyopia, surgery may alleviate the source of deprivation such as a cataract, ptosis, or corneal opacities. Similarly, eye muscle surgery can correct strabismus-related amblyopia. In most cases of strabismus, completion of patching or atropine treatment before surgical correction is recommended.
Patching
Application of an adhesive patch over the non-amblyopic eye is the first line and most common technique used to treat amblyopia. This forces stimulation of the amblyopic eye and promotes development of the associated visual pathway. Full time patching works most quickly and allows children to expect consistency but needs frequent follow-up to prevent risk of occlusion amblyopia development in the other eye. For some families, patching in shorter intervals, such as for 2 to 6 hours per day fits better with the child’s routine and is sufficient to treat mild-moderate amblyopia. Studies have shown that patching for 40 hours a week is nearly as effective as full-time patching, with lower risk of reverse amblyopia [20,21], although patching will extend over a longer time than with full time patching.
Although incredibly effective, patching is associated with high rates of noncompliance related to discomfort with use of the amblyopic eye and from wearing the patch itself. Compliance with therapy can be increased with time and parental education regarding patching therapy [21,22,23].
For a more detailed review of full time vs. part time patching therapy please visit http://www.eyerounds.org/cases/178-Amblyopia-Management.htm
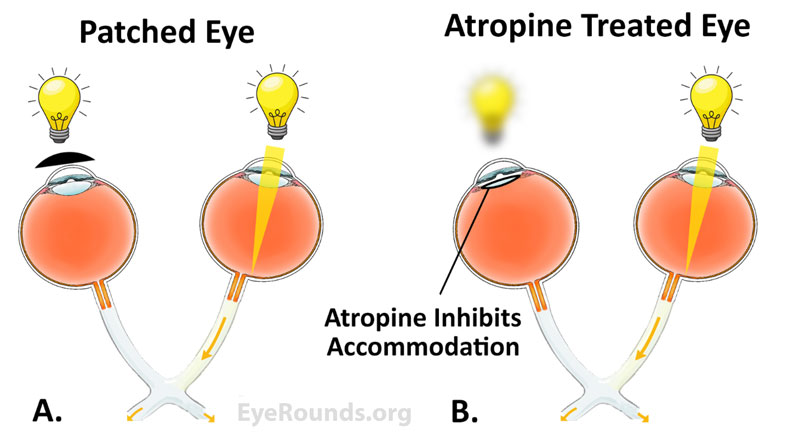
Pharmacologic penalization
Pharmacologic penalization of the non-amblyopic eye is another commonly used method to treat amblyopia. The pharmacologic agent used for this therapy is often topical atropine 1%. Administration of atropine causes paralysis of the ciliary muscle resulting in dilation of the pupil, paralysis of accommodation, and subsequent blurring of near vision. Dosing of atropine drops can differ between a drop daily, every other day, or on weekends only. To further blur distance vison of the non-amblyopic eye and promote further use of the amblyopic eye, refractive correction can be adjusted to further disadvantage the non-amblyopic eye [21,22].
Patching therapy has demonstrated more rapid visual improvement; however, atropine has the advantage of being much easier to administer and being preferred by families over patching [21,23]. Due to these advantages, atropine therapy has gained popularity in recent years.
Miscellaneous
Other methods available for treatment of amblyopia include optical penalization with an occlusive filter placed on the glasses lens and blur-inducing contact lenses, however these options are more easily removable. Currently dichoptic movies and video games that require use of both eyes are also under investigation as potential novel therapies for amblyopia. However, these methods have not yet shown to provide an additional benefit to vision or stereoacuity when compared to patching and spectacle use [24-27].
The prognosis of amblyopia is highly dependent on severity of the initial visual deficit and age at the initiation of treatment. The goal of amblyopia treatment is equal vision between the two eyes. If left untreated, amblyopia can lead to an irreversible lifelong decrease in vision. Unfortunately, even with effective treatment some level of residual amblyopia may remain, and in some cases, patients do not respond to therapy at all [2].
The best outcomes are seen in children who are treated before maturation of the visual pathways, typically before age 9. Treatment success is dependent on a young age at detection, early intervention, and appropriate compliance with treatment. If treated properly, more than 70% of patients experience significant vision improvement within 12 months [2].
Unfortunately, cessation of amblyopia treatment poses a risk of recurrence and even after successful treatment there may be some progressive visual decline with age. The greatest risks of recurrence are better visual acuity at the time of treatment cessation, higher number of lines improved during the previous treatment, and a prior history of recurrence [21].
Similarly, patients who stop patching abruptly rather than gradually prior to cessation have a higher risk of amblyopia recurrence. Regular follow-up during the amblyogenic years is required for all children who have been previously treated for amblyopia [2,21]. If detected in the second decade of life, most guidelines do not recommend beginning amblyopia therapy. Although mild improvement has been obtained in select cases of amblyopic treatment of older children, the degree of improvement is significantly less than that obtained in treatments started in the first decade of life [28].
Amblyopia is the most common cause of unilateral vision loss in children caused by suppression of visual pathway development. Patching therapy and pharmacologic penalization can be used to encourage proper visual pathway development, and in some cases surgical intervention may be required. In most cases, visual acuity can be improved if detected early, thus, screening for amblyopia is vital and should begin at 12 months of life.
Wolfel L, Hendricks T, Kemp P. Amblyopia: From One Medical Student to Another. EyeRounds.org. January 9, 2023; Available from: https://EyeRounds.org/tutorials/amblyopia-medical-students/index.htm