
The University of Iowa
Department of Ophthalmology and Visual Sciences
August 11, 2015
Amblyopia is maldevelopment of the visual cortex in the brain during infancy or early childhood that leads to decreased central vision in the affected eye. The hallmark of amblyopia is decreased monocular vision that is not accounted for by other ocular pathology. Any abnormality that leads to irregular visual stimulation can cause amblyopia, including strabismus, anisometropia, or media opacity. Amblyopia causes more unilateral cases of reduced vision in childhood than all other causes combined, and it affects approximately 2-5% of all children (1,2). The pathology of amblyopia generally occurs by one of two mechanisms. First, a blurred or incomplete image on the retina during the period of visual development (from birth until approximately 10 years of age) inhibits cortical activity in the brain, ultimately leading to underdevelopment of vision in the affected eye. Second, in the setting of strabismus, misaligned eyes prevent the child from developing fusion of the images from each eye, which leads the brain to suppress the image from the deviated eye so as to avoid diplopia (3), which in turn reduces the visual potential of that eye.
Left untreated, patients can have significant visual impairment that persists throughout life. The long-term risk of binocular visual impairment is higher in patients with monocular amblyopia who are reliant on their non-amblyopic eye for clear vision. Van Leewen et al. determined that the lifetime risk of bilateral visual impairment for patients with amblyopia was 18%, nearly double that of individuals without amblyopia (4), emphasizing the long-term disability that can come from amblyopia if left untreated.
The key to treatment success of amblyopia is early detection. The goal of vision screening is to detect poor vision or risk factors for poor vision at a time when therapy can be initiated to achieve good visual outcomes. The U.S. Preventive Services Task Force currently recommends vision screening for children ages 3-5 (5); however, screening has been successfully implemented in infants as young as 6 months of age. The ideal treatment window for amblyopia is the first decade of life, because it is during this period that neural development occurs, and treatment after this critical time is dramatically less effective. Treatment includes correcting the underlying cause as well as correcting the amblyopia itself. Correction of the underlying problem may involve ocular muscle surgery for strabismus, surgical removal of media opacities such as cataracts, or the use of spectacles to improve refractive error. Patching or pharmacologic blurring of the non-amblyopic eye with atropine are used to strengthen the visual pathway of the amblyopic eye. A study published in 2002 indicated that greater than 75% of children under the age of seven can achieve visual acuity of 20/30 or better with treatment by either patching or atropine (6). Follow-up in that study showed that at age 15 years, about 60% of treated amblyopic eyes had visual acuity of 20/25 or better, suggesting that most children continue to have good visual acuity, although a mild residual amblyopia is common (7). Van Leewen et al. determined that the number needed to treat (NNT) to prevent one case of bilateral visual impairment in an amblyopic patient is only 12.5 (4), which emphasizes the high utility of treatment.
The American Association for Pediatric Ophthalmology and Strabismus recommends that elective instrument-based photoscreening, described in detail below, be performed between 6 months and 3 years of age (8). In 2011, the U.S. Preventive Services Task Force concluded that insufficient evidence was available to support vision screening before age 3. However, Longmuir et al. published a study in 2013 that examined 11 years' worth of data collected from the Iowa KidSight database, a volunteer organization that performs vision screening throughout Iowa, and analyzed the effectiveness of photoscreening for amblyopia in children ages 6 months to 6 years (9). No statistical difference was identified between screening outcomes of children younger than 3 years compared to children ages 3 to 6 years, supporting the use of vision screening in younger children. Additionally, Kirk et al. concluded that children with amblyopia who were identified before age 2 had post-treatment visual acuity outcomes that were, on average, one line better than children who were diagnosed between ages 2 to 4 years, which represents a substantial difference in visual acuity (10).
Vision screening modalities either screen for amblyopia directly or screen for the risk factors associated with amblyopia. Direct screening requires the patient to reliably respond to the examiner to assess visual acuity using a vision chart. Instrument-based testing on the other hand, does not test for a visual deficit directly, but tests for common risk factors associated with amblyopia. An advantage of instrument-based testing is that it does not require much participation from the child and can be performed in preverbal infants.
Tests of visual acuity directly test for the presence of amblyopia. Visual acuity testing has a subjective component and therefore responses to visual acuity testing should be interpreted in the context of the patient's age, ability, and level of cooperation. Ideally, the patient is able to identify letters or symbols on a chart a fixed distance away by naming or matching. As patient participation is fundamental, visual acuity testing must be performed in cooperative children. It is commonly not possible to test visual acuity with a matching or naming test until the child is 3 years old. Visual acuity testing in preverbal infants and toddlers is most commonly performed by assessing the fixation preference or by using forced preferential looking tests such as Teller cards. It is imperative that the testing distance is accurate and appropriate for the chart used. Commonly used vision charts for matching and naming tests include Sloan, HOTV, Lea symbols, and Patti Pics (11). It is also crucial when attempting to test for amblyopia that each eye is tested individually. Stick-on eye patches or pediatric occlusion glasses are useful to adequately cover the eye not being tested. Kennedy et al. evaluated the efficacy of traditional vision screening, including both visual acuity and stereo acuity testing, to detect amblyopia in 1245 kindergarteners. The results showed that compared to a formal ophthalmologic examination, vision screening identified 94.2% of patients with visual defects (12).
The presence of amblyopia causes very small abnormalities in fixation in the amblyopic eye. Optical tracking is a method for measuring eye movement and has been proposed as a way to directly detect small abnormalities in fixation, and by extension, the presence of amblyopia. Unfortunately, most eye tracking devices using the corneal reflection or pupil are too insensitive to detect these small fixation changes. A reflection from the birefringent Henle fibers of the fovea has been imaged by one device that may be sensitive enough to detect the small fixation abnormalities present in amblyopia (13). Currently this device is being tested in a clinical setting in children and is not available to the public, but it may show promise to directly detect the presence of amblyopia in the future.
Optokinetic nystagmus is a reflex that develops around 6 months of life. It is a horizontal rapid refixation movement that is seen when the patient is attempting to follow a moving object with his or her eyes. It is tested by rotating an optokinetic drum in front of the patient. Optokinetic nystagmus can be used as a crude evaluation of an intact visual system. Lack of optokinetic nystagmus in one eye suggests amblyopia. However, this test lacks the precision necessary to have utility as a vision screening tool for amblyopia.
Neutral density filter testing has been shown to identify amblyopia and to help distinguish strabismic amblyopia from other causes. A neutral density filter reduces the intensity of all wavelengths of light equally. Von Noorden and Burian compared healthy eyes to amblyopic eyes due to strabismus and amblyopic eyes due to known organic pathology such as macular degeneration, optic nerve atrophy, and chorioretinitis (14). They demonstrated that use of a neutral density filter in healthy eyes reduces the visual acuity by a constant amount, while in eyes with strabismic amblyopia, vision was only slightly reduced, stayed the same, or actually improved. Vision in the amblyopic group with organic pathology showed a marked reduction in visual acuity with use of the filter. The conclusion was that neutral density filter testing could be used to identify amblyopic eyes and to differentiate causation between strabismus and other pathologies (14). This test has not been incorporated into screening programs for amblyopia to our knowledge.
Visual evoked potentials (VEP) are changes in voltage measured on the scalp over the occipital lobes with sensitive electrodes. The voltage changes when the eyes are viewing a visual stimulus. In theory, measuring the brain function directly may eliminate the need for a behavioral response from the child being tested. The use of VEP in vision screening has been tested by showing subjects progressively smaller sized visual stimuli until the VEP becomes extinguished; this threshold corresponds to the minimum angle of resolution for the child. This is known as a sweep VEP. In practice, for vision screening devices based on VEP, the child must be cooperative enough to fixate for at least 30 seconds on a screen and tolerate the electrode array being attached to the head. Simon et al. tested a version of the VEP device to screen for amblyopia in a group of children 6 months to 5 years old and compared the device to the gold standard, a comprehensive eye examination. The test could be completed by 94% of children, and they found a sensitivity of 97% and a specificity of 80% (15).
There are several ocular pathologies that often accompany amblyopia, but may also occur in the absence of amblyopia, including anisometropia, strabismus, media opacity, or reduced stereovision. Screening programs based on detection of these risk factors for amblyopia have been instituted across the country using devices that can function quickly at low incremental cost.
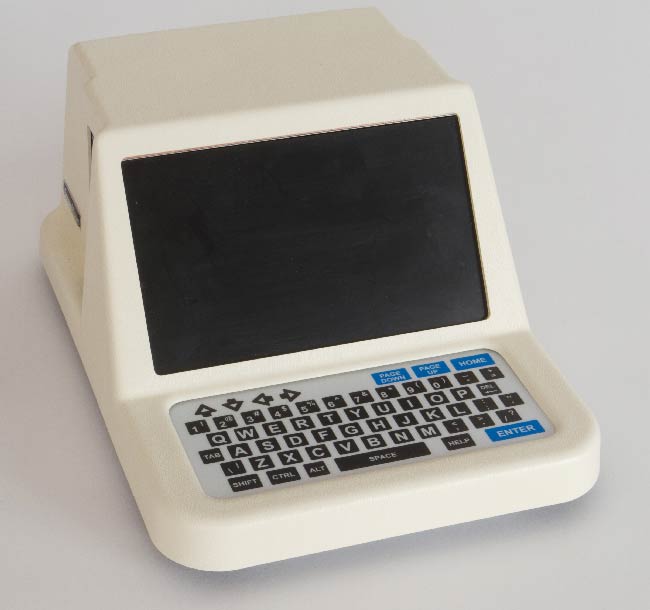
Photoscreening is the interpretation of photographs for ocular defects that may be associated with amblyopia. A photograph of the child's eyes is analyzed to detect pathology such as refractive error, media opacities, strabismus, or other external eye abnormalities such as ptosis (Figures 1-4). The photo can be interpreted by an ophthalmologist, a central reading center, or by computer (8). Based on pre-determined referral criteria, a selected population of patients with a positive screen are then referred to an ophthalmic professional for a comprehensive eye examination. In a nine-year retrospective analysis of 147,809 children, Longmuir et al.determined the positive predictive value (PPV) of photoscreening was 94.2% (16). The most commonly identified pathologies were refractive error (83.9%) and strabismus (12.1%). Only less than 1% of referred children were found to have a media opacity, but photoscreening had a 100% PPV for identifying media opacities (16). Currently available photoscreeners include the iScreen and Plusoptix (11). Most modern photoscreening devices allow the user to set the specificity and sensitivity criteria in order to tailor the number of referrals that will be generated depending on the needs of the screening program. The companies that provide the device may also provide an interpretation of the images that involves a subscription fee.




Autorefraction is automated retinoscopy that determines the refractive error of each eye. Autorefraction requires the subject to remain still during the examination, and therefore requires more patient cooperation than photoscreening (depending on the speed of the machine). Autorefraction evaluates each eye independently, which limits the ability to screen for strabismus (7). Kemper et al. determined that for children ages 3-5, the sensitivity and specificity of monocular autorefraction for detecting amblyogenic pathology is 88% and 58%, respectively (16). The sensitivity for children younger than 3 years was 80%, though only 49% of the photos in this age group were considered "testable" and subsequently analyzed (17). Some of the currently available devices based on autorefraction technology include: Retinomax, SureSight and Spot (11). The Plusoptix device incorporates both photoscreening and autorefraction technology, and the Retinomax also has a keratometer fuction. The Vision in Preschoolers Study Group identified the Retinomax Autorefractor and the SureSight Vision Screener as more sensitive screening methods to detect amblyopia, compared to Lea Symbols visual acuity and the Stereo Smile II (18).
A variety of screening programs exist throughout the country. No single progam is used nationwide. Functioning programs include volunteer-based programs, school programs, and screening offered by general pediatricians. Most states have laws requiring a vision screening examination prior to enrolling in school. The Lions Clubs International is a service organization that has provided eye care services for nearly 100 years. They organize vision screenings that aim to identify amblyopia in preschool age children. For example, the Lions Club of Iowa partners with the University of Iowa Department of Ophthalmology and Visual Sciences and the University of Iowa Sight (UISight) program to host vision screenings at local community centers. They screen children ages 6 months to 6 years via photoscreening for amblyogenic risk factors.
There are also many school-based programs that will perform vision screening prior to entering kindergarten. The Vision in Preschoolers Study Group determined that, compared to one another, trained nurses and lay screeners have similar efficacy when performing preschool vision screenings (18). Lay screeners were able to successfully identify children in need of a more comprehensive ophthalmic examination with similar sensitivities to those of trained nurses. Requirements for vision screening in schools vary by state with only 8 states having no such policy (19).
Vision screening is also performed by general pediatricians. The American Academy of Pediatrics (AAP) recommends that pediatricians begin evaluating visual acuity as early as practically possible, which is generally interpreted as 3 years of age (20). To assess vision in children from birth to 3 years of age, the AAP recommends observing the patient's ability to fix and follow objects. The AAP also endorses elective photoscreening and autorefraction by pediatricians in children ages 6 months to 3 years, recognizing that adoption of this technology is highly dependent on insurance companies' payment policies for this service (8).
Ocular photographs obtained via electronic applications are the basis of the most productive pediatric vision screening programs. In 2012, Arnold et al. described a prospective study using a variety of portable vision screening devices, including the iScreen, Plusoptix, and Pediavision Spot (Figures 5-7), to detect amblyopia risk factors and identified sensitivities ranging from 72%-84% (21). In 2013, Vaughan et al. described the use of the iCheckKids photoscreening iPhone application to test preschool age children for refractive error and strabismus (22). Although none of the smartphone applications have currently been approved for vision screening, improvements in diagnostic accuracy are on the horizon. Smartphone photoscreening applications would allow widespread distribution of the technology needed to identify children at risk for amblyopia. Upcoming technologic advances have the potential to revolutionize pediatric vision screening.


The advantage of screening programs based on autorefraction or photoscreening technology is the low incremental cost. Once the program has invested in the device, the additional cost per screening event is quite low. Using comprehensive eye examinations by an ophthalmologist or optometrist to screen for amblyopia would be the most expensive and least efficient screening method. The comprehensive eye exam should be reserved as the confirmatory test for those that have a positive screen using other modalities.
Amblyopia is common in the pediatric population, affecting 2-5% of children (1,2). With early screening efforts and appropriate treatment, good visual outcomes can be achieved. The U.S. Preventive Services Task Force recommends vision screening for all patients aged 3 to 5 years. The American Academy of Pediatrics and the American Association for Pediatric Ophthalmology and Strabismus endorse instrument-based vision screening for patients beginning at age 6 months. With the help of volunteer-based organizations, school programs and general pediatricians, successful vision screening programs are widely available. Technological advances currently available and others on the horizon may make vision screening even more readily accessible.
Links below are for informational purposes only and do not imply an endorsement by the authors or the University of Iowa.
Donaghy CL, Larson SA. Vision screening for amblyopia. EyeRounds.org. posted August 11, 2015; Available from: http://www.EyeRounds.org/tutorials/amblyopia/