
The University of Iowa
Department of Ophthalmology and Visual Sciences
August 3, 2020
Repeat each category three times:
Visual Acuity
|
| Confrontation Visual Fields |
Alignment Assessment
|
| Extraocular Muscle Ductions |
| Pupil Assessment |
Penlight Assessment
|
| Instillation of Drops |
If you have a cooperative human at home, please perform these skills on them. Ideally, do this three days in a row. One time, we will plan on having the clerkship director observe your skills via Zoom for Direct Observation of Physical Exam Skills
In the setting of current events, our ophthalmology curriculum has shifted from an in-person clinical curriculum to online, necessitating increased student responsibility for their learning and time management.
In this assignment, please reflect on your approach to self-directed, individual learning.
Please target about two paragraphs of reflection, no more than approximately 500 words.
We will discuss your thoughts at our feedback session mid-rotation.
Administrative goals: |
Practice goals:
|
For this session, students will be paired. One student will act as a patient, and their history and physical exam will be provided to them.
The other student will act as the examiner, and start by taking a history. Then, the examiner will ask the patient for physical exam information in oral boards style. For example:
Examiner: "I will check the patient's visual acuity with a near card, by asking him to cover one eye with the palm of his hand, wear his habitual glasses and hold the near card at 14 inches away."
Patient: "The visual acuity in my right eye is 20/20, and in the left eye is 20/40."
Examiner: "I will now check the confrontation visual fields by...." etc.
Then, students will switch roles. The history and physical exam provided to the next student will be a different case.
After this is completed, students will each write a note with the information they obtained and submit as Patient Note 2.
Chief Complaint
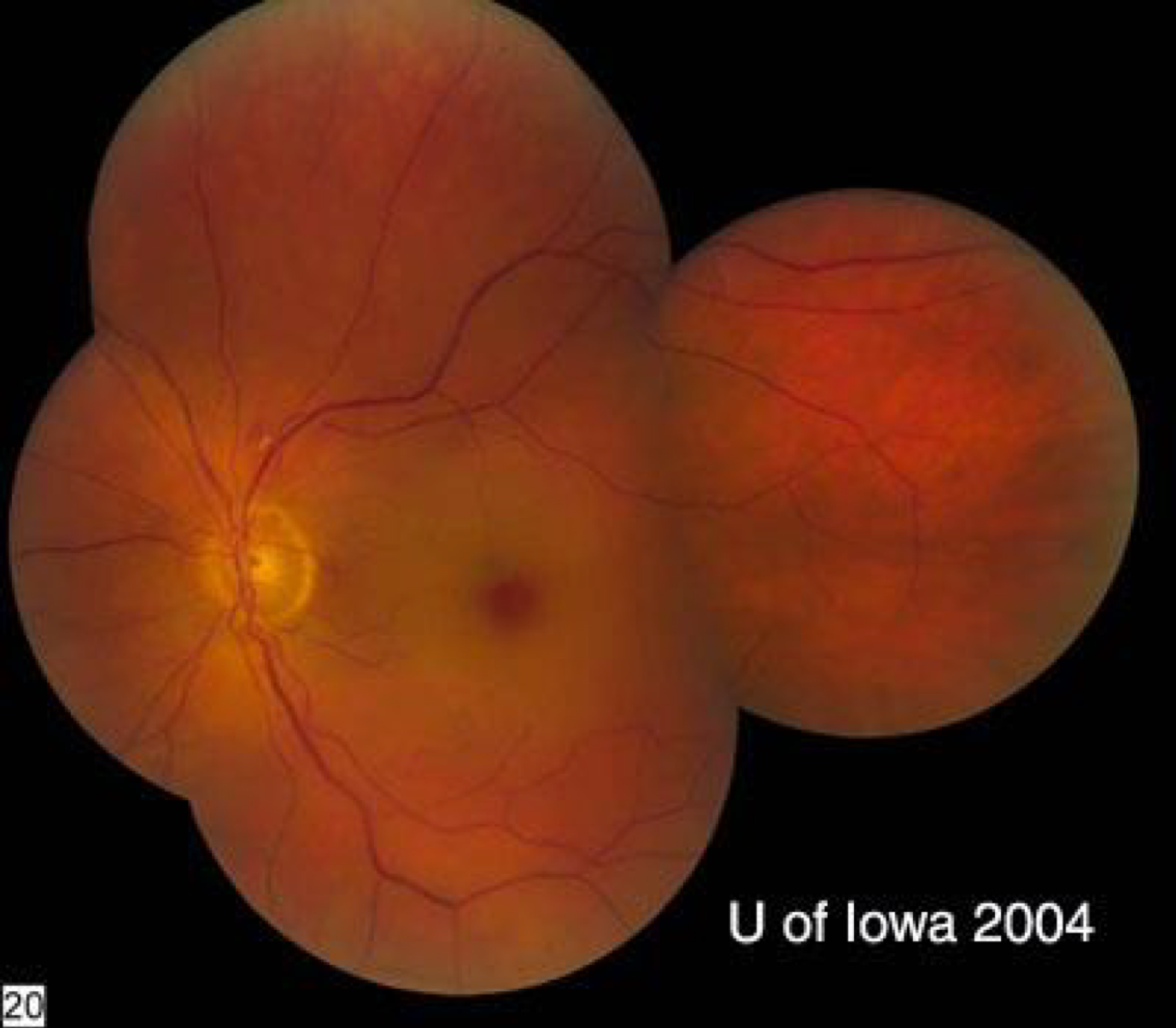
81-year-old with sudden, painless vision loss OS.
History of Present Illness
POHx
PMHx
FHx
SHx: Retired school teacher, lives alone
Meds: ASA, Plavix, nitroglycerine PRN and alfalfa pills
Allergies: None
ROS: denied headaches, jaw claudication, scalp tenderness, weight loss, and loss of appetite, otherwise as in HPI or negative
EXAM
Chief Complaint
34-year-old with watery, red, irritated eyes; left more than right
History of Present Illness
POHx: Former contact lens wearer (five years ago), now only wears glasses for myopia. No eye surgery or trauma
PMHx: Healthy
PSHx: Tonsillectomy in childhood
FHx: Maternal grandmother with macular degeneration (in her 80s), paternal grandfather with recent cataract surgery
SHx: Married, works as an accountant
Meds: Daily multivitamin
Allergies: None
ROS: As in HPI, otherwise negative
EXAM

Please find an interesting case on AAO Medical Student website, the Indiana University case website, or EyeRounds, and write a patient note on this case.
Do not copy and paste into your note. If you do so, you will get reduced points. This should be your work, and you should understand all parts of your note. Write out all abbreviations.
Please include:
Please note 2 will be based on your history taking exercise.
Please include:
Prepare and present a 6 to 8 minute presentation on an ophthalmological diagnosis, which could be commonly encountered by a primary care provider or perhaps relevant to your own future career. You may use EyeRounds as the foundation for a 'patient' to present.
Suggested Format
Resources
Due Dates
By the Wednesday at 5:00 pm, notify the course director of your chosen topic
On Friday of your rotation, present your project to your peers and instructor at the morning learning session.
Examples of appropriate topics
|
|
This is not an exhaustive list – any topic covered in your Basic Ophthalmology textbook can be a good topic, or email the course director with your idea.
Scoring Component |
Value |
| Evaluations | 10 points (score x 2) |
| Written Exam | 60 points (percentage correct x 0.6) |
Discussion Sessions
|
30 points (6 sessions each worth 5 pts) |
| Professionalism | Loss of points |
| Requirements for Pass | Final Score: > 70 Final Exam: ≥ 60% Evaluation: ≥ 3.0 |
| Clerkship Failure | Final Score: 0-69.9 Failure to complete criteria regardless of points Attendance/Participation: Clerkship failure if more than 2 days missed Evaluation: < 3.0 Written Exam: score < 60% (eligible for one retake) Discussion Sessions: more than 1 missed Required clinical encounters incomplete |